Abdominal Flaps and Implants
Maurice Y. Nahabedian
Introduction
The desire to achieve symmetry following mastectomy and breast reconstruction is a reasonable and attainable goal. Women who have had breast reconstruction following mastectomy expect it and virtually all surgeons will do what they can to deliver it. Often times, symmetry will be achieved with the initial reconstructive attempt whether it be using prosthetic devices or autologous tissue (1,2,3,4). However, there are situations that may arise in which initial symmetry is not achieved and secondary procedures may be needed (1,2,3,4). These asymmetries can be of many varieties and require secondary procedures on the ipsilateral breast, contralateral breast, or bilateral breasts. The specific secondary procedure can include prosthetic augmentation of a contralateral natural breast or prosthetic augmentation of an ipsilateral breast that has been reconstructed with autologous tissue. Other options include reduction mammaplasty, mastopexy, autologous fat grafting, and contouring procedures. All of these options have been successfully applied and warrant detailed explanations regarding specific indications and techniques; however, this chapter will focus only on prosthetic augmentation following breast reconstruction with abdominal flaps.
There are four abdominal flaps that are currently used for autologous breast reconstruction that include the pedicle transverse rectus abdominus rectus (TRAM), free TRAM, deep inferior epigastric perforator (DIEP), and superficial inferior epigastric artery (SIEA). A detailed explanation of these flaps will not be provided in this chapter but is provided in the specific chapters in this text. The fact that three of these flaps require microvascular techniques is important because it can influence the timing in which a prosthetic device is inserted. With a pedicle TRAM, an implant can be inserted at the initial procedure because the implant will not usually jeopardize the blood supply to the flap. Spear et al. reviewed his experience with simultaneous prosthetic augmentation following pedicle TRAM flap surgery in 14 patients (5). Within this group of patients, three developed infection (18%) and 3 had partial flap loss (18%). These results suggest that perhaps a delayed insertion may be preferable as a means of reducing the internal pressure that is applied to the flap and to minimize the infection risk. When a microvascular flap reconstruction has been performed, an implant can be inserted simultaneously however, it is more often the case that it be inserted in a delayed fashion. Simultaneous insertion of a prefilled device can potentially compromise the circulation through a fresh microvascular anastomosis; however, the simultaneous insertion of a postoperatively adjustable device may be considered.
Prosthetic augmentation of the contralateral rather than reconstructed breast has been the focus of some investigations. Simultaneous insertion of a contralateral implant at the time of the initial TRAM flap has been previously described (5,6). Chang et al., have described this approach in 10 women who had pedicle TRAM flaps and simultaneous contralateral augmentation (6). All women had small to medium size breasts. A small saline device was inserted in the subpectoral position. There were no postoperative implant failures with excellent aesthetic results obtained in 9/10 (90%). Spear et al., have described contralateral prosthetic procedures in 18 women following pedicle TRAM flap surgery (5). A difference from the Chang study was that 10 women had contralateral reconstruction in which 2 women had the devices inserted before the TRAM flap, 5 women had the devices inserted simultaneously with the TRAM flaps, and three women had devices inserted following the TRAM flap. In eight women, a contralateral augmentation was performed. In all 18 cases, the device was a round or contoured saline device. All 18 women tolerated this procedure well with no postoperative infections or other morbidities related to the flap.
In preparation for this chapter, the author has reviewed his experience with breast reconstruction using abdominal flaps in concert with prosthetic devices. Of 732 women that had breast reconstruction with an abdominal flap, there were 24 identified that had breast reconstruction with an abdominal flap and prosthetic devices. The time interval for these 24 women was from June of 1998 to February of 2008. Of these four had a pedicle TRAM, four had a free TRAM, and 16 had a DIEP flap. A bilateral procedure was performed in 15 women and a unilateral procedure in 9 women. The total number of reconstructed breasts that were augmented with a prosthetic device was 39. The devices were inserted in a delayed fashion for 35 breasts and simultaneously in 4 breasts. Simultaneous insertion was performed in two women that had bilateral pedicle TRAM flaps.
This chapter will focus on secondary procedures using prosthetic devices for the breast reconstructed with an abdominal flap. The review will include indications, device selection, device insertion techniques, complications, and outcomes.
Indications
The indications for prosthetic augmentation of the reconstructed breast are several. In cases of unilateral reconstruction in which there is some degree of asymmetry, a woman will have two choices. These include modification of the contralateral breast using techniques such as reduction mammaplasty, mastopexy, or prosthetic augmentation in addition to augmentation of the reconstructed breast with a prosthetic device. Although autologous fat grafting is also an option for augmentation of the reconstructed breast, it will not be reviewed here but will be reviewed in a subsequent chapter. In cases of bilateral reconstruction, the final outcome may not meet the patients’ expectations in terms of volume, dimensions, or projection. In these cases, a delayed insertion of a prosthetic device is useful. In cases, in which the patient desires autologous
reconstruction and it is anticipated that the final breast volume will be shy of expectations, the devices can be inserted simultaneous provided that careful attention be directed to the location of the vascular pedicle.
reconstruction and it is anticipated that the final breast volume will be shy of expectations, the devices can be inserted simultaneous provided that careful attention be directed to the location of the vascular pedicle.
Despite the concerns of some surgeons, there are others that have demonstrated the safety and efficacy of simultaneous implants and abdominal free flaps (7,8). Miller et al. have demonstrated the feasibility of simultaneous prosthetic devices and free flap breast reconstruction using adjustable devices (7). In their description, the postoperatively adjustable device was inserted in a submuscular pocket that was formed by the pectoralis major muscle, the serratus anterior, and the muscular portion of the TRAM flap. The saline chamber of the device will filled to 60–80% of capacity. In this series of five patients, there were no anastomotic failures; however, 2 women did develop a seroma following drain removal. The authors concluded that this technique was safe and obviated the need to use a tissue expander. Serletti and Moran utilized a similar technique in one woman following bilateral free TRAM flaps and simultaneous insertion of saline implants placed in the submuscular position (8).
The main contraindication for prosthetic augmentation of a breast reconstructed with an abdominal flap is when the flap has been radiated postoperatively. This will often result in clinical or subclinical evidence of soft tissue fibrosis which will limit the amount of elasticity required to accommodate an implant. The risk of infection, delayed healing, exposure of the device, and poor outcome is increased (9). Prosthetic augmentation can be considered if the radiation was delivered before the flap reconstruction.
Device Selection
When combining an abdominal flap with an implant, there are several details that must be considered. The first is that even through a reconstructed breast may look and feel like a natural breast; it does not behave like a natural breast. There is a plane of scar tissue between the pectoralis major muscle and the flap. In the case of a pedicle TRAM, the rectus abdominis muscle that enters the breast pocket inferomedially and is positioned on top of the pectoralis major muscle. In the case of a microvascular breast reconstruction, there is a vascular pedicle that is anastomosed either to the internal mammary or thoracodorsal system. These anatomic features will impact the selection and placement of the prosthetic device.
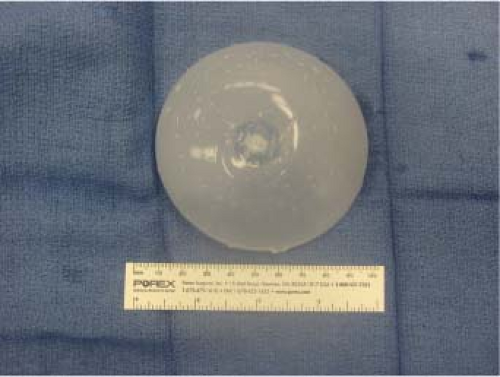
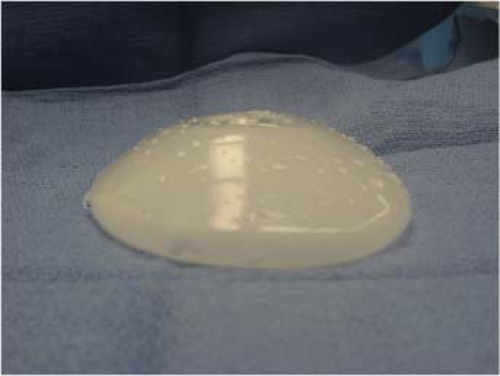
There are several types of implants that this author has used in the setting of prosthetic enhancement of a breast reconstructed with abdominal tissue. These include smooth saline implants, postoperatively adjustable implants of the Becker Type (Mentor Corporation, Santa Barbara, CA), and silicone gel implants (Figs. 58.1 to 58.3). It is preferred to use devices that are adjustable either intraoperatively or postoperatively rather than prefilled devices because of the ease of insertion. The elasticity of a breast reconstructed with a flap is less than that of a natural breast because of the surrounding scar tissue that has developed. Because of this reduced elasticity, larger devices (greater than 200 cc) are rarely used. A typical implant will be in the range of 100–150 cc in volume, although they can be larger when appropriate and in properly selected patients. The devices are usually smooth surface and round. Textured or contoured devices can be used but are not generally preferred
by this author except in the cases where a Becker implant is used. The smooth surface has an advantage in that it will allow the device to settle into the breast pocket and contour naturally over time. When a postoperatively adjustable device is used, the implant can be filled to a certain amount intraoperatively and then adjusted postoperatively based on soft tissue elasticity and compliance. The remote port can be placed on the lateral chest wall or beneath the inframammary fold. These ports come in a small and large size and are selected based on the degree of body fat. Thinner patients will usually receive the smaller remote port and heavier patients will receive the larger port.
by this author except in the cases where a Becker implant is used. The smooth surface has an advantage in that it will allow the device to settle into the breast pocket and contour naturally over time. When a postoperatively adjustable device is used, the implant can be filled to a certain amount intraoperatively and then adjusted postoperatively based on soft tissue elasticity and compliance. The remote port can be placed on the lateral chest wall or beneath the inframammary fold. These ports come in a small and large size and are selected based on the degree of body fat. Thinner patients will usually receive the smaller remote port and heavier patients will receive the larger port.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree