9 Tendon Transfers for Low Ulnar Nerve Palsy
Abstract
Various tendon transfer procedures have been described to help compensate and reestablish function in patients who have suffered low ulnar nerve palsy. Tendon transfer principles include using an expendable donor, synergistic function, similar excursion and power, straight line of pull, and one transfer for one function. While tendon transfers can help to improve function, the physician and patient should understand that permanent limitations are likely.
9.1 Key Principles
It is critical to understand the various deficits caused by a low ulnar nerve palsy and understand which tendon transfers restore which lost function.
There should be an individualized treatment plan for each patient.
The muscles affected in a low ulnar nerve palsy include the ulnar two lumbrical muscles, all interossei muscles, the adductor pollicis, deep head of the flexor pollicis brevis, and the hypothenar muscles.
Lumbricals and interossei muscles normally cause flexion of the metacarpophalangeal (MCP), extension of the proximal interphalangeal (PIP), and extension of the distal interphalangeal (DIP) joints. Paralysis of the intrinsic muscles causes inversion of the function causing clawing (MCP extension, PIP and DIP flexion) due to unbalanced contraction of the long digital extensor and flexors.
Clawing of the ring and small fingers: This occurs due to paralysis of both the interossei and lumbrical muscles to these two fingers, whereas the index and middle fingers remain unaffected because the lumbricals to these two fingers are left innervated by the median nerve.
Grip strength is also decreased because of the clawing in the fourth and fifth fingers.
Froment sign: when the adductor policis brevis is paralyzed, the force of the secondary thumb adductor—extensor policis longus (EPL)—results in thumb adduction and MCP extension. This causes stretching of the flexor policis longus (FPL) causing thumb IP flexion. This position with the thumb in adduction, MCP extension, and thumb IP flexion is called the Froment sign. Pinch is affected due to the paralysis of thumb adductor and the first dorsal interosseous both of which stabilize the thumb for pinching (► Fig. 9.1).
Wartenberg sign: paralysis of the third-volar interosseous, which normally adducts the digit, along with the unopposed abduction force of the extensor digiti minimi (EDM), causes abduction of the fifth finger called Wartenberg sign.

9.2 Expectations
The goal of surgery is to improve function. Communication with the patient to understand his or her functional deficits and shared decision making can help to construct the most appropriate surgical plan. The patient should understand that normal function cannot be restored. Small improvements in patients with catastrophic injuries or complete nerve palsy can be relatively impactful. At best, the patient will have noticeable weakness when comparing the repaired and unaffected side.
9.3 Indications
It is important to remember that patients treated with nerve repair may take 12 or more months to demonstrate improvement. Electromyographic (EMG) testing may help to evaluate nerve recovery, if any, after repair.
The neuromuscular junction is irreversible after 12 months from nerve injury. Within this period is considered appropriate for nerve repair/transfer, after which tendon transfers are indicated.
Transfers for low ulnar nerve palsy are indicated for correcting the claw deformity in the fourth and fifth digits, increasing the pinch power, and preventing thumb adduction.
9.4 Contraindications
Contracture: Patients with contractures within the motor groups affected by the ulnar nerve injury or contracture within the donor group is an absolute contraindication for tendon transfer surgery.
Polyneuropathy or no adequate donor tendon: There needs to be an acceptable donor muscle group. Muscle force drops at least one grade after transfer (based on the muscle force grading of 0–5); thus, the transferring muscle must not be compromised.
Infection: Active infection is a contraindication for tendon transfer surgery.
Spasticity: Patients with central nervous system deficits may be contraindicated for specific tendon transfers.
9.5 Special Considerations
MP hyperextension occurs with lack of intrinsic flexion against an unopposed and intact extensor digitorum communis.
Clawing is typically worst in the small and ring fingers due to median innervated lumbricals.
With a low ulnar nerve injury, the flexor digitorum profundus (FDP) to the small and ring fingers are intact, and therefore, can make the appearance of clawing more severe when compared to higher ulnar nerve injuries.
9.6 Special Instructions, Positioning, and Anesthesia
Regional anesthesia with sedation or with general anesthesia
Supine on hand table
Upper arm tourniquet
9.7 Tips, Pearls, and Lessons Learned
9.7.1 Correction of Clawing
Bouvier Maneuver
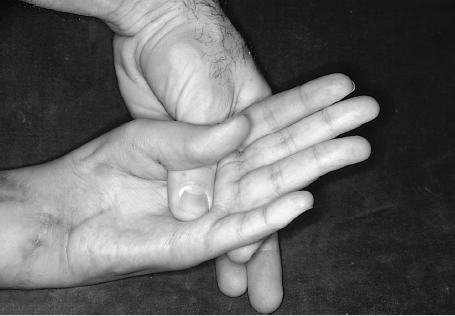
Prior to addressing a clawing deformity, it is important to perform a Bouvier maneuver. To perform this test, hold the MP joints in slight flexion, and ask the patient to extend the interphalangeal joints (► Fig. 9.2). A positive test is demonstrated when the patient can extend the IP joints, and confirms the competence of the extensor mechanism.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








