Based on histological findings, the primary target of the inflammatory reaction in lichen striatus is the keratinocyte in the basal and suprabasal layers. The occurrence along the lines of Blaschko also favours the keratinocyte as the target cell [1].
Familial cases of lichen striatus are rare and occur mostly in siblings, usually simultaneously, suggesting a common environmental trigger [29–31]. There is, however, a report of a Japanese family with a boy and his mother affected at 3 years of distance [37]. Familial occurrence is unlikely via the somatic mutation mechanism because these mutations take place by chance. An epigenetic mosaicism has been suggested to contribute to skin diseases following the lines of Blaschko [38]. These skin diseases might be caused by visualization of the actions of transposable elements that are partly expressed and partly silenced at an early developmental stage. Epigenetic rather than genomic mechanisms fit better the familial observations of lichen striatus.
Pathology.
Lichen striatus lacks specific pathological findings. A mixed lichenoid–spongiotic pattern that may vary according to the age of the lesion has been described by several authors (Fig. 86.3) [4,39–41]. According to Reed et al. [41], histopathological examination of 23 cases was not sufficient to differentiate lichen striatus from lichen nitidus and lichen planus.
Fig. 86.3 Lichen striatus: predominant spongiform pattern with marked lymphocytic exocytosis (haematoxylin–eosin–saffron stain, original magnification ×64).
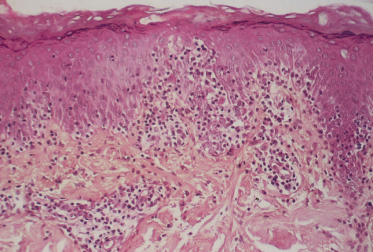
The largest study of the pathology of lichen striatus included 41 childhood cases [39]. The authors concluded that histological examination was diagnostic in 50% of cases. The diagnosis should be based on the following features: (i) a focal band-like infiltrate with (ii) variable exocytosis and (iii) a collection of histiocytes in the dermal papillae. Slight acanthosis and focal parakeratosis, together with satellite cell necrosis, have been described. Additional features of interest include the alignment of the infiltrate along hair follicles and eccrine ducts [1,2,32] and, occasionally, a dense deep dermal lymphocytic infiltrate [32,42] and intraepidermal vesicles filled with Langerhans cells and CD8+ T-lymphocytes. CD8+ intraepithelial lymphocytes are sometimes scattered but are most often located in clusters around necrotic keratinocytes, thus supporting the hypothesis of a cytotoxic process directed towards keratinocytes [1]. Most of the small lymphocytes in the upper dermis and epidermis are positive for CD7 [2]. According to Gianotti et al. [2], the age of the lesion does not influence the ratio of non-specific to diagnostic histological changes. In 50% of cases, non-specific findings were noted.
Clinical Features.
Lichen striatus is not rare, but it may frequently go undiagnosed [1,3,22,43]. It is more common in children than in adults and is mostly found in young children (median 2–3 years). Recruitment or reporting bias may have led to the preponderance of older patients (age 5–15 years) that is documented in the literature [3]. Large series indicate a female predominance [22,43]. The lesions are distributed on the trunk in around one-third of cases and on the limbs in the remaining two-thirds. Pruritus is moderate and uncommon (around 10% of cases). Clinical features of atopy and minor signs of atopic dermatitis are commonly associated [22] (Fig. 86.4). Psoriasis (Fig. 86.5) and vitiligo [3] can be associated. The mean duration is 6–9 months (4 weeks to 10 years; median around 6 months). Relapses may occur within the first 4 years [1,22].
Fig. 86.5 Lichen striatus in a 7-year-old girl with psoriasis. (a) Lichen striatus with psoriasiform features of the thigh suggesting the Koebner phenomenon; (b) typical chronic psoriasis on the back.

Lichen striatus is acquired and not congenital. The most characteristic feature is the linear arrangement of inflammatory lesions, ranging in extent from a few centimetres to an entire limb or half of the trunk (Fig. 86.6). The lesions are erythematous, papular and sometimes vesicular and eczematous [44]. Often there is a lichenoid appearance (Fig. 86.7), but Wickham’s striae are absent. A perforating variant has been described [45].
Fig. 86.6 Lichen striatus in a 16-month-old boy. (a) Blaschko line arrangement of lesions; (b) detail showing lichenoid papules.

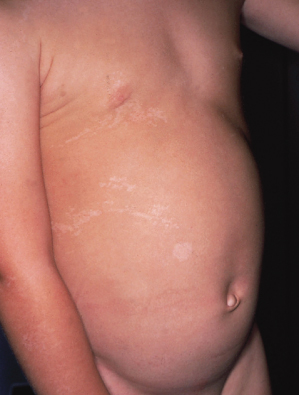
The linear eruption appears in 2–3 weeks and usually disappears in several months, leaving depigmentation in 50% of cases (Fig. 86.8) [1]. Hyperpigmentation has also been noted [46]. The lesions may form in a single line or occur in grouped divided lines. Streaks may be discontinuous. Hemi-corporeal forms with multiple streaks are exceptional, as are bilateral forms [47]. The authors found that lesions occur more commonly on the left side of the body, and particularly on the upper left side (trunk and arms) [1], but this was not confirmed in a larger series [22]. Facial involvement is less uncommon than previously thought [22] but can be difficult to diagnose if a limited portion of a Blaschko’s line is involved because of less frequent access to biopsy (Fig. 86.9). Follicular involvement with transient focal hair loss [40] and nail dystrophy are sometimes noted before typical cutaneous lesions have been observed [48,49]. Nail involvement can be isolated [50].
Fig. 86.8 Lichen striatus: hypopigmented stage in a 2-year-old boy; differential diagnosis includes hypomelanosis of Ito.
Prognosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree












