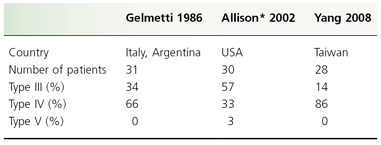
Table 83.2 Comparison of reviews of juvenile pityriasis rubra pilaris using Griffiths’ classification
* One patient had type V, one had mixed II–IV, and one progressed from type IV to type III.
Two other classification systems are presented for comparison. Gelmetti et al. [36] proposed four types based on the clinical duration of disease (Table 83.3), and listed primary and secondary diagnostic features resulting from analysis of 29 children (Table 83.4). The limitation of this system is that classification can only be carried out in retrospect, as it is not known whether or not in any particular patient the condition will resolve within the critical period of 1 year. The classification of Piamphongsant and Akaraphant [37], based on a study of 104 children and 64 adults, relied on the features at presentation (Table 83.5). However, 22 of their patients evolved from one type to another.
Table 83.3 Classification of pityriasis rubra pilaris proposed by Gelmetti et al. 1986 [36]
| Type | Time to clear | Percentage |
| Acute | <6 months | 51.7 |
| Acute with prolonged course | <1 year | 10.7 |
| Chronic | >1 year | 39.3 |
| Hereditary | – | 0 |
Note: All can have localized or diffuse lesions.
Table 83.4 Clinical criteria proposed by Gelmetti et al. 1986 [36]
| Primary diagnostic criteria |
| Follicular papules (knees, ankles, hands) |
| Keratoderma |
| Cephalic rash |
| Salmon colour |
| Secondary diagnostic criteria |
| Oedema (non-pitting) |
| Nail changes |
| Ectropion |
| Koebner phenomenon |
| Pruritus |
| Mucosal changes |
| Histology |
| Resistance to therapy |
Table 83.5 Classification of pityriasis rubra pilaris proposed by Piamphongsant and Akaraphant 1994 [37]
| Type | Clinical signs | Percentage |
| I | KD only | 20.2 |
| II | KD + KE + F (local) | 56.7 |
| III | KD + KE (face, trunk, limbs) | 19.2 |
| IV | KD + erythroderma + F (widespread) | 3.9 |
| V | KD + erythema + F | 0 |
KD, keratoderma; KE, scaly patches on knees and elbows; F, follicular plugging.
Pityriasis Rubra Pilaris Clinical Types.
Types I (Classic Adult) and II (Atypical Adult)
These are by definition, confined to adults and are described elsewhere [5].
Type III (Classic Juvenile)
Type III typically presents at age 5–10 years. Clinically it resembles type I (classic adult); however, type III may have a better prognosis than type I. The eruption starts as an orange–red macule, often on the upper torso or head and neck, covered with a fine scale described as bran-like (Figs 83.1–83.3). This early phase is often initially misdiagnosed as seborrhoeic dermatitis. Within a few weeks or months, further macules appear, and with the increasing numbers many perifollicular erythematous papules appear, containing an acuminate keratinous plug in the follicle. Lesions rapidly coalesce and spread in a cephalocaudal direction to become erythrodermic. Islands of sparing, a characteristic feature seen in widespread PRP, range in size up to 1 cm in diameter, are frequent and can be found in the middle of vast zones of erythema. They should not be confused with the uninvolved areas near the margins of spreading psoriasis, or with the geographical outline seen in erythrokeratoderma progressiva. At the outset or soon after, the palms and soles thicken and form a thick, even, yellow keratoderma (‘PRP sandal’) (Figs 83.4 and 83.5). The scalp is covered with pityriasiform scale and the face is bright orange–red and taut, often producing ectropion in severe cases. The nails may be normal, or may gradually become thickened, yellowed and curved. Longitudinal striae, or terminal hyperaemia (half-and-half nail) may be seen. The hair and oral mucosa are unaffected. In the erupting stage, there may be marked pruritus, sometimes with a burning sensation, but this improves as the disease stabilizes. The eruption reaches a peak and often begins to resolve spontaneously after several months to a year.
Fig. 83.1 Type III pityriasis rubra pilaris: confluent orange–red erythema spreading cordially; note follicular lesions.
Courtesy of Dr William Griffiths.

Fig. 83.2 Type III pityriasis rubra pilaris: sharply demarcated, salmon-coloured erythematous scaly patch on the back.
Courtesy of Dr Albert Yan.

Fig. 83.3 Type III pityriasis rubra pilaris: erythematous scaly plaques on the face and neck. Note sparing in the sun-protected area of the neck.
Courtesy of Dr Albert Yan.

Fig. 83.4 Dorsum of the hands showing salmon coloured erythema. Note the follicular papules peripheral to the erythema.
Courtesy of Dr Albert Yan.

Fig. 83.5 Salmon-coloured erythema with some scaling on the palms. Keratoderma is a variable feature in pityriasis rubra pilaris.
Courtesy of Dr Albert Yan.

Type III may be preceeded by a febrile illness or infection. Griffiths estimated that 16% of type III patients clear spontaneously in 3 years, but the series by Yang et al. [28] documented a protracted course of longer than 3 years in two-thirds of patients with type III and IV disease.
Type III was most common paediatric type in Allison et al.’s [25] series from the USA; however, type IV was most prevalent in two other paediatric series by Yang et al. [28] in Taiwan and Gelmetti et al. [36] in Italy. Type III can rarely transform into type IV.
Type IV (Localized Juvenile)
This circumscribed form usually presents in prepubertal children. Palmoplantar keratoderma is a cardinal feature. Erythematous grouped follicular papules appear on the knees and elbows, and occasionally the anterior shins (Figs 83.6 and 83.7). The lesions are non-pruritic. The skin between the follicular lesions may become erythematous and scaly, forming a red scaly plaque with marked follicular prominence. Minor lesions consisting of faint red macules with a fine scale or grouped follicular keratotic plugs are often found elsewhere on the trunk and on the scalp. Confluent scalp involvement is not seen in this type.
Fig. 83.6 Type IV localized pityriasis rubra pilaris: prominent follicular scales on an erythematous plaque on the knee.
Courtesy of Dr William Griffiths.

Fig. 83.7 Type IV localized pityriasis rubra pilaris: scaly plaques on the knee.
Courtesy of Dr Albert Yan.

Type V (Atypical Juvenile)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








