8 Prophylactic Subcutaneous Mastectomy
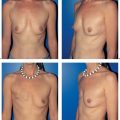
Subcutaneous mastectomy is defined as the complete removal of all breast tissue while leaving the nipple–areola complex intact. Dissection on the gland leaves more breast tissue than strict subcutaneous dissection (removal of 90 % vs. 95–98 %). In our view, removal of the nipple–areola complex in prophylactic surgery is not justified, since the resulting aesthetic compromise outweighs any gain in oncological safety.
The introduction of silicone gel implants in the 1960s and early 1970 s helped popularize the notion of complete removal of all vulnerable breast tissue, followed by implant reconstruction. Widespread use of the technique was based on the belief that the resulting breast had a natural appearance and feel. Over time, however, it became evident that inadequate soft-tissue coverage of the implant could lead to major surgical complications—resulting in poor or even disastrous cosmetic outcomes, with the associated psychological distress.
The goal of the operation as originally defined—removing as much at-risk tissue as possible, while at the same time recognizing the aesthetic and psychosexual importance of the breast—also proved unattainable. Resection leads to impaired sensation in the breast skin and complete denervation of the nipple. Subsequent implant reconstruction often involves complications such as capsular contracture, a foreign-body sensation, coldness, and displacement, and the corresponding loss of natural appearance. Subcutaneous mastectomies are therefore beingcarried out less and less often.
However, the value of this technique was confirmed in a study by Hartmann (1999), who confirmed that the risk of developing cancer declines in direct proportion to the amount of breast tissue removed—which in clinical terms is logical. In high-risk patients, the likelihood of developing breast cancer could thus be reduced by 90% by prophylactic mastectomy. This possibility had long been viewed skeptically, and the study confirmed the oncological effectiveness of subcutaneous mastectomy.
In view of the increasing incidence of breast cancer and the identification of gene mutations that can lead to it, the issue of preventive mastectomy is currently being reassessed. In addition, the development of autologous tissue reconstruction has been a major step forward in avoiding the complications associated with implants.
Indications
From the physician’s point of view, there is no medical reason for performing subcutaneous mastectomy. Malignant changes or intraductal atypia have to be managed with a breast-conserving operation or by mastectomy. Lobular carcinoma in situ—once considered a classic indication for subcutaneous mastectomy—is no longer viewed as necessarily precancerous, and treatment thus consists of clinical observation without immediate surgical implications. Surgery is also no longer indicated for atypical intraductal or lobular hyperplasias, which were previously viewed as precancerous lesions.
Surgical treatment of the very rare cases of diffuse papillomatosis (with or without atypia) should be discussed with the patient on the basis of the individual case.
Ultimately, it is the patient’s personal decision whether sub-cutaneous mastectomy is appropriate. All the potential draw-backs of this surgical procedure have to be clearly explained and thoroughly discussed.
Factors that argue in favor of subcutaneous mastectomy in individual patients range from psychological distress in patients with cancer phobia to detection of a BRCA1 or BRCA2 gene mutation. A family history of breast cancer can also be an indication for prophylactic mastectomy, particularly if the tissue concerned is difficult to examine using routine surveillance procedures. In the United States, prophylactic mastectomy is often considered to be indicated in patients who have cancer in the contralateral breast.
Surgical Technique
It should be mentioned initially that there is no surgical standard of care for subcutaneous mastectomy. Generally speaking, surgery only makes sense in conjunction with reconstruction. This increases the degree of variation, however, since the choice of reconstruction can also influence the type of resection.
Some surgeons carry out subcutaneous mastectomy in the same way as a modified radical mastectomy. A long transverse incision is made across the breast, for wide surgical exposure, and the nipple–areola complex is resected. In our opinion, this procedure should no longer be used. Instead, aesthetic factors should also be givendue consideration in prophylactic surgery, as they can help minimize physical and psychological damage.
Some surgeons prefer to dissect a thicker flap of skin and glandular tissue (particularly in combination with implant reconstruction). However, this reduces the effectiveness of the procedure. Dissection on the glandular tissue achieves a 90% reduction of breast tissue. Extensive subcutaneous mastectomy, using strict subcutaneous dissection similar to a total mastectomy, removes 95–98 % of breast tissue.
So far as we are aware, there have been no prospective and randomized studies conclusively demonstrating the superiority of one technique over the other. It can be indirectly concluded from the study by Hartmann, however, that the risk of developing cancer decreases in proportion to the amount of breast tissue removed.
The classic approach is the inframammary fold incision. Unfortunately, this incision is associated with poor surgical exposure, particularly in the superomedial and superolateral quadrants (with an increased risk of recurrent bleeding).
A periareolar incision around half the perimeter achieves far better exposure. Depending on the breast size, the incision can be elongated laterally Precise excision of tissue immediately behind the nipple is possible under direct visualization. The exposure of the superolateral quadrant with the predominant vascular supply is also clearly superior to that provided by an inframammary incision.
Tumescent infiltration of subcutaneous tissue with a saline/epinephrine solution helps facilitate dissection with minimal bleeding. We therefore carry out the operation with the following steps.
After infiltration of subcutaneous tissue with about 200 mL of tumescent fluid, a semicircular incision is made around the inferior areolar perimeter and then carried laterally. The proper plane of dissection in prophylactic mastectomy is immediately above the glandular tissue (deep subcutaneous tissue). In contrast to modified radical mastectomy, the dissection plane is not in the subcutis; it is not assumed that there is infiltration of atypical cells beyond the glandular tissue, as in oncological surgery. Preserving as much subcutaneous tissue as possible has the advantage of sparing the subdermal vascular plexus while providing more favorable implant coverage, with better mobility, warmth, and breast skin sensation. Although a more “aggressive” dissection plane can be chosen if autologous tissue reconstruction is planned, deep subcutaneous dissection has benefits in with regard to ensuring blood circulation and resensitizing the skin flap.
Behind the nipple, the lactiferous ducts are sharply transected under direct vision. The nipple is carefully cored out, with care being taken to avoid the risk of nipple necrosis. Subcutaneous dissection continues to the periphery of the breast until the glandular tissue has been completely dissected free. Next, the glandular tissue is dissected off the chest wall from medial to lateral. It is not necessary to include pectoral fascia. Special attention should be given to dissecting the axillary tail in order to remove all glandular tissue, if possible. Meticulous hemostasis is imperative. Larger veins in the subcutaneous tissue should be ligated rather than coagulated, to avoid damaging the skin.
The use of a head lamp is strongly advised, as it greatly improves the visualization of the surgical field.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree