Borderline Leprosy
In borderline leprosy, the granulomas consist of diffusely spread epithelioid cells and lymphocytes and macrophages containing acid-fast bacilli. The nerve bundles show moderate Schwann cell proliferation, but such cells are usually recognizable. Acid-fast bacilli are found in moderate numbers (BI = 2–5+).
Lepromatous Leprosy
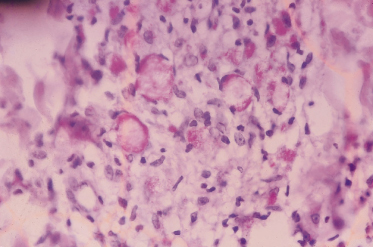
The diffuse granuloma in lepromatous leprosy is separated from the atrophic epidermis by a clear Grenz zone (band of Unna) and consists of macrophages with foamy cytoplasm loaded with acid-fast bacilli (BI = 6+), the so-called lepra or Virchow cells (Fig. 70.2). Lymphocytes and plasma cells are very scanty and spread haphazardly between the macrophages. The lymphocytes in lepromatous leprosy are predominantly CD8 cells. The CD4/CD8 ratio is <1 [56].
Fig. 70.2 Granuloma in lepromatous leprosy. Macrophages loaded with acid-fast bacilli (lepra cells = Virchow cells) (Fite–Faraco stain).
Acid-fast bacilli can be demonstrated in histological sections and slit-skin smears. These are generally made from four to six different sites in suspected leprosy cases, like two skin lesions, the earlobes, the nasal mucosa and the back of the fingers. The smears are then stained for acid-fast bacilli according to the Fite–Faraco method [55] and examined with the microscope using a ×100 oil immersion objective. The numbers of bacilli in a smear, the BI, is recorded according to the following scale:
- 0 = no bacilli found
- 1 + = 1 to 10 bacilli in 100 microscopic fields
- 2 + = 1 to 10 bacilli in 10 microscopic fields
- 3 + = 1 to 10 bacilli in an average microscopic field
- 4 + = 10 to 100 bacilli in an average microscopic field
- 5 + = 100 to 1000 bacilli an average microscopic field
- 6 + = 100 to 1000 bacilli or many clumps in an average microscopic field.
The BI is arrived at by adding the values from all the skin sites examined and by dividing the total number of sites.
It is just as important to examine the percentage of the bacilli that stain solid (morphological index, MI). To determine the MI, at least 100 bacilli, preferably 200, are examined [57]. Bacilli that stain irregularly, or are fragmented or beaded, are dead. The MI is a useful indicator of progress in patients under treatment and changes more rapidly than the BI. Patients become non-infectious even with first dose of MDT, though MI may become zero in about 6 weeks. A rise in the MI while a patient is receiving treatment indicates lack of compliance by the patient, incomplete absorption of the drug or that the bacilli have become resistant to the drug.
Clinical Features.
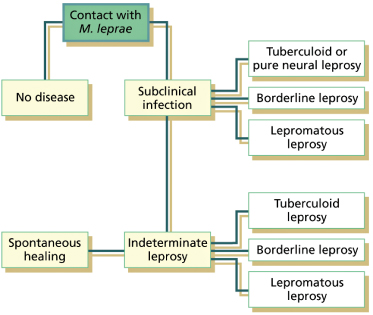
Leprosy can manifest itself in different ways. The various clinical manifestations are not due to infection with different strains of M. leprae, but reflect the variations in the tissue response of the host to the presence of M. leprae in the body. Thus, they are manifestations of different host–parasite relationships. The different clinical forms of leprosy form a spectrum with tuberculoid leprosy at one end and lepromatous leprosy at the other. Between the two poles are the borderline tuberculoid, mid-borderline or borderline borderline, and borderline lepromatous forms (Fig. 70.3). To this classification, which was introduced by Ridley & Jopling and based on immunology [58], two subpolar forms were introduced, namely the subpolar tuberculoid and subpolar lepromatous leprosy [59]. The skin lesions are in general similar to those found in adult patients. However, in children the lesions are usually not so clear-cut, and smaller and less numerous than in adults [60]. Exposed parts are the most common sites involved in children,
In children, the spectrum of leprosy is reported to be incomplete and largely confined to tuberculoid, borderline tuberculoid, mid-borderline and indeterminate forms [60]. It is a paradox that children, who have poor cell-mediated immunity, rarely present with multibacillary disease.
Tuberculoid Leprosy (TT)
Tuberculoid leprosy is characterized by one or a few well-defined lesions that show central healing (Fig. 70.4). In dark skins they are hypopigmented and in light skins they appear as copper coloured. In the lesions, loss of sensation (hypo-aesthesia or anaesthesia) can be demonstrated, except when localized on the face, where there is a rich supply of sensory nerves. The surface of the lesion is dry because of impaired sweating. Hairs can be reduced in number or even absent.
Fig. 70.4 Tuberculoid leprosy. Solitary, well-defined, hypopigmented lesion, with tendency to central healing, in a 12-year-old boy. Note some small satellite lesions.

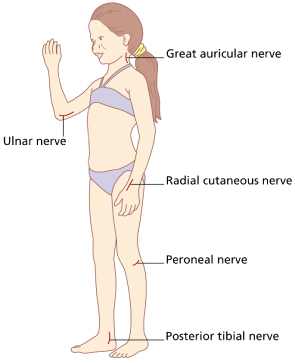
In tuberculoid leprosy, the peripheral nerves, mostly solitary, can be thickened and painful. In order of frequency, the nerves most often involved are the ulnar, posterior tibial, peroneal, radial cutaneous and great auricular (Fig. 70.5). Loss of sensory perception in the areas supplied by the enlarged nerve can be found. Muscular paresis or paralysis with or without contracture also can be seen but are infrequent in children [60]. Besides involvement of the large peripheral nerves, there may be enlargement of a small superficial nerve near a skin lesion. This finding is of great diagnostic significance. Bacteriological smears are negative or slightly positive (0–1+); the lepromin reaction is strongly positive.
Borderline Tuberculoid Leprosy (BT)
This is the most common spectrum of disease encountered in children other than indeterminate leprosy. The skin lesions of BT leprosy resemble those of tuberculoid leprosy; however, there are many more lesions (usually 3–10), showing variation in size and contour and a tendency to symmetry. The lesions are less well defined and there may be areas where the margin streams off gradually into the normal skin. Pseudopodia and satellite lesions are frequently found near the edge of the lesion (Fig. 70.6). The size of lesions tends to be larger and at times it may cover the entire limb of a child (Fig. 70.7). Loss of sensation is less intense than in the lesions of TT. Dryness, scaling and erythema or hypopigmentation of the lesions are also less conspicuous than in TT. Nerve involvement is much more widespread and frequently severe. Several of the large peripheral nerves may be irregularly thickened in an asymmetrical pattern. Nerve damage is one of the characteristics of BT leprosy, resulting in anaesthesia and/or muscle paresis or paralysis in the distribution of the damaged nerve and finally deformities. Bacteriological smears are slightly positive (1–2+) and the lepromin reaction is positive.
Fig. 70.6 Borderline tuberculoid leprosy. Erythematous plaque with lip involvement. Note some small satellite lesions.

Mid-Borderline Leprosy (BB)
Borderline leprosy is the most unstable form in the leprosy spectrum and represents usually a transient stage in the course of the disease. It can downgrade or reverse. This form of disease is rare in children and shows clinical features of tuberculoid as well as of lepromatous leprosy – in other words, dimorphous features. Thus, borderline leprosy is also called dimorphous leprosy. There are many skin lesions, but not as many as in lepromatous leprosy. The lesions (macules, plaques, nodules), which are reddish or brownish in colour, may vary greatly in size, shape and distribution. The edges may be well defined in one area and ill defined elsewhere. Some lesions show irregular borders, streaming and satellites, giving them a geographical appearance. Very characteristic but rare are the so-called ‘Swiss cheese’ punched-out lesions. These lesions are erythematous plaques with ill-defined outer edges and a punched-out centre with a well-demarcated edge. Nerve damage is variable in this form of leprosy. Bacteriological smears are positive (BI 3–4+) and the lepromin reaction is weakly positive.
Borderline Lepromatous Leprosy (BL)
Lepromatous spectrum of disease is relatively uncommon in children. The skin lesions in BL (macules, plaques, punched-out lesions, papules and nodules) are similar to those found in lepromatous leprosy. However, they are more distinct, more variable in shape and are not distributed absolutely symmetrically in the body as in lepromatous leprosy patients. Signs of nerve damage within the lesion, such as loss of sensation, decreased sweating and hair growth, start sooner in BL than in lepromatous leprosy. There occur slightly infiltrated numerous macules with a copper hue, round or oval about 2–3 cm in diameter. With disease progression, papules, nodules and plaques may develop, with sloping margins which merge imperceptibly into normal skin. Areas of apparently normal skin can be found between the lesions. Annular punched-out lesions that look like inverted saucers are common. Large peripheral nerves become enlarged sooner than in lepromatous leprosy. Bacteriological smears are highly positive (BI 4–5+) and the lepromin reaction is doubtful (+/–).
Lepromatous Leprosy (LL)
Lepromatous leprosy represents the other pole of the spectrum, with the patient unable to resist the infection, leading to uncontrolled multiplication of the bacilli. These are found in high concentrations in the skin and nerves, mucous membranes of the upper respiratory tract, lymph nodes, spleen, liver, testes and other organs. The early skin lesions of lepromatous leprosy are macules, which are numerous and symmetrically distributed. They are ill defined, slightly hypopigmented or erythematous and have a shiny surface. As the disease progresses, the lesions coalesce, so that the whole body is uniformly affected. In the early lesions there is no sensory loss.
In advanced disease, general infiltration of the skin develops as plaques, papules and nodules, of which some may ulcerate. Thickening and folding of the skin are most pronounced in the face, causing the classic lion-like facies or ‘facies leontina’. This severe form of lepromatous disease is rare in children. Nerve involvement in advanced disease is bilateral and symmetrical, resulting in ‘glove and stocking’ type anaesthesia. Other findings that can be found in lepromatous leprosy patients are loss of eyebrows and eyelashes (madarosis), gynaecomastia, testicular atrophy, oedema of the hands and feet and trophic ulcerations. More serious findings are deformities such as collapse of the nose, claw hands and foot drop. Bacteriological smears are always highly positive (BI 6+) and the lepromin reaction is negative.
Indeterminate Leprosy
Indeterminate leprosy is one of the most common forms of leprosy seen in children. This early and unstable form occurs in those whose immunological host response has not yet declared itself. It is characterized by one or a few vague hypopigmented or faintly erythematous macules with rather ill-defined borders (Fig. 70.8). Hair growth and nerve functions are usually not affected. These lesions may be slightly drier than normal adjacent skin and occasionally present with a creased or wrinkled appearance. There may be a suggestion of hypo-aesthesia; however, usually there is no morphological change except for a slight change in skin colour. The lesions are localized commonly on the exterior surface of the limbs or the buttocks, or on the face. Indeterminate leprosy is the first sign of the disease in 20–80% of patients.
Fig. 70.8 Indeterminate leprosy. Solitary hypopigmented, ill-defined lesion on the face in a 10-year-old child.

In most leprosy control programmes, indeterminate leprosy is frequently overdiagnosed [61]. The diagnosis of indeterminate leprosy can only be confirmed when a biopsy has shown the presence of bacilli or typical neural infiltration, or when there is definite impairment of sensations. Biopsy may show perineurovascular infiltrate, but AFBs are mostly not demonstrable by newer molecular diagnostic methods. About 75% of the patients with indeterminate leprosy heal spontaneously, whereas the other 25% develop one of the other forms of leprosy, depending on the cell-mediated immune response. When the clinical diagnosis of indeterminate leprosy is doubtful and histology is not available or inconclusive, it is appropriate to keep a child under close supervision for few months to observe the disease course rather than labelling a patient as having leprosy and make them suffer the stigma.
Special Forms
Three other types of leprosy are sufficiently distinctive to allow separate descriptions but they are rarely seen among children. These are the pure neural leprosy, histoid leprosy and Lucio leprosy.
Pure neural leprosy is characterized by damage and enlargement of one or more of the larger nerve trunks. There are no skin lesions present and slit-skin smear in negative. Nerve biopsies show that the majority of these patients belong to the tuberculoid end of the spectrum [62].
Histoid leprosy is a special manifestation of lepromatous leprosy and was first described by Wade in 1963 [63]. It is characterized by papules and sharply demarcated, firm nodules. Histoid leprosy has been reported generally to manifest in patients after long-term dapsone monotherapy, irregular or inadequate therapy. However, there are also reports of disease developing as relapse after successful treatment or even appearing de novo without a prior history of any antileprosy treatment. Clinically, the histoid lesions commonly appear as smooth, shiny, hemi-spherical, dome-shaped, non-tender soft to firm nodules which may be superficial, subcutaneous or fixed deeply under the skin and plaques or pads appearing on otherwise normal-looking skin. The lesions are usually located on the face, back, buttocks and extremities and over bony prominences, especially around the elbows and knees. On histological examination, spindle-shaped cells containing M. leprae are found. Bacteriological smears are highly positive (BI 6+) and the lepromin reaction is negative.
Lucio leprosy (lepra bonita), first described by Lucio and Alvarado in 1852 [64], is characterized by a diffuse shiny infiltration of all body skin with widespread sensory loss. As the disease progresses, the eyelids become thickened, giving the patients a sleepy and sad appearance. Madarosis is often the first sign. Patients may complain of numbness of the hands and feet, nasal congestion and epistaxis, hoarseness of the voice and oedema of the feet. The skin contains large numbers of M. leprae. Bacteriological smears are highly positive (BI 6+) and the lepromin reaction is negative. Lucio leprosy is considered the most anergic of the entire immunological spectrum of leprosy.
Diagnosis.
The diagnosis of leprosy is mainly based on the clinical signs and symptoms of the disease. A case of leprosy is a person having one or more of the following three cardinal signs, and who has yet to complete a full course of treatment [65]: hypopigmented or reddish skin lesion(s) with definite loss/impairment of sensations; involvement of the peripheral nerves, as demonstrated by definite thickening with loss of sensation in the area of distribution; and positive skin smear for acid-fast bacilli. Only in rare instances is there is a need for laboratory investigations and histopathology for confirmation of diagnosis. A skin biopsy should be taken wherever facilities are available from the most representative skin lesions to confirm the clinical diagnosis and for histological classification. The skin biopsy should include the full depth of the dermis and should be taken from the most active edge of a lesion. A nerve biopsy is necessary when pure neural leprosy is suspected.
Prognosis.
Leprosy can be cured. The introduction of MDT in 1982 has resulted in a drastic reduction in the prevalence of leprosy [66]. It was this success that led the World Health Organization to achieve the goal of eliminating leprosy as a public health problem by the year 2000 at global level [7]. After completion of MDT, the overall relapse rates are about 0.1% [65]. Relapses though very rare in children, it strongly correlate with a high BI (4+) at the baseline [67]. The prognosis in children who have received the full treatment course is excellent [10,68]. Despite a decline in the number of new cases, management of reactions, prevention and care of disabilities are of unprecedented significance in leprosy control programmes. Promisingly, more effective, operationally less demanding and more patient-friendly new-generation MDT regimens are on the horizon, which will significantly accelerate the process of attaining the leprosy elimination goal at all levels and make the world free of leprosy (see below).
Differential Diagnosis.
The clinical presentation of leprosy is highly variable and in all its stages it can mimic a great variety of other dermatological and neurological disorders. Macular leprosy lesions must be differentiated from common paediatric dermatoses like vitiligo, tinea versicolor, naevus anaemicus, naevus depigmentosis and pityriasis alba.
The differential diagnosis of pityriasis alba with indeterminate leprosy can be difficult when lesions are restricted to the face, because loss of sensation may be very difficult to demonstrate in such lesions. The lesions of pityriasis alba may be single to few in number, occur usually over the face or occasionally on the upper trunk. The lesions are erythematous to begin with and while resolving, leave ill-defined, round to oval, slightly scaly hypopigmented patches. They often show seasonal variation and self-resolution. The lesions do not show loss of sensation, impairment of sweating or hair growth, or nerve thickening. Biopsy is rarely required which will show changes of spongiotic dermatitis.
Onchocerciasis is an endemic disease in West and Central Africa, Sudan, Mexico and Guatemala, characterized by vague hypopigmented macules on the back and thighs. They can be differentiated from lepromatous leprosy by the demonstration of microfilariae in skin smears.
Annular leprosy lesions may resemble granuloma annulare, tinea corporis, lichen planus, syphilis and granuloma multiforme. The cause of granuloma multiforme is unknown. It occurs in parts of East and West Africa and Indonesia. The early lesions are papulonodular and they develop into well-defined plaques of various sizes and shapes, and annular lesions. They are localized predominantly on the upper parts of the body. Localization on the dorsum of the hands, as seen in granuloma annulare, is rare. The disease occurs in adults and is seldom seen in children. There is no loss of sensation in the lesions and no enlarged peripheral nerves. Histologically, degeneration of collagen (necrobiosis) and many foreign body giant cells are seen in the dermis.
Infiltrated leprosy lesions may mimic lupus vulgaris, sarcoidosis, discoid lupus erythematosus, cutaneous leishmaniasis (especially the disseminated anergic form in which the Leishmania
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree