7 Flexor Tendon Repair
7.1 Flexor Tendon Repair
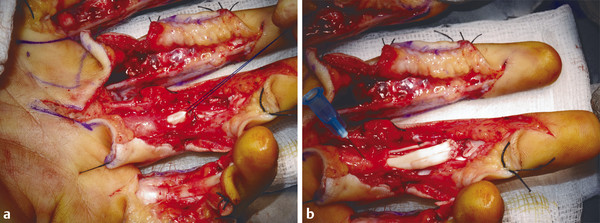
The case illustrates a patient who grasped a knife with a clenched fist and subsequently has multiple zone 2 flexor tendon divisions (Fig. 7‑1). These injuries can be time consuming to repair and require technical skill and appropriate hand therapy. Single-digit flexor tendon injuries can be repaired under local anesthetic and adrenaline technique, however, in multitendon injury, as in the case above, general anesthetic is supplemented with regional anesthetic and tourniquet.

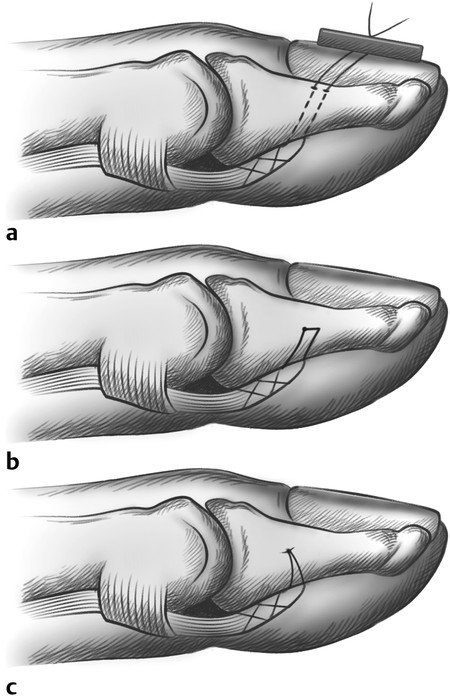
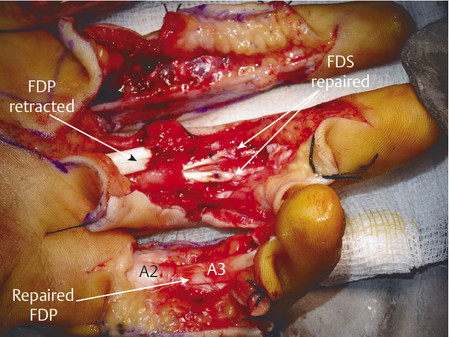
Anatomically, these injuries are divided into five zones. Zone 1 injuries occur distal to the flexor digitorum superficialis (FDS) insertion (Fig. 7‑2, Fig. 7‑3). If the flexor digitorum profundus (FDP) tendon becomes detached from the bone, a number of techniques have been described to reattach the tendon to bone. These range from Mitek mini anchor, pullout technique with button, and transosseous repairs (Fig. 7‑4 a–c). Zone 2 has its distal boundary at the FDS insertion and proximal boundary at the distal palmar crease. Zone 2 was known as no man’s land and had poor outcomes historically, until Kleinert popularized direct repair with postoperative rehabilitation exercises. Zone 3 injuries occur in the palm, zone 4 in the carpal tunnel, and zone 5 in the wrist and forearm.
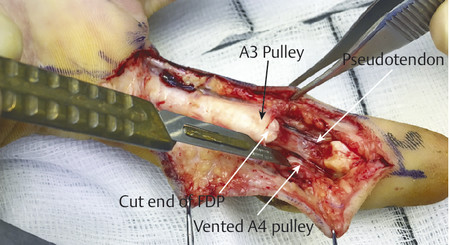
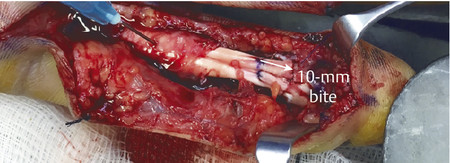
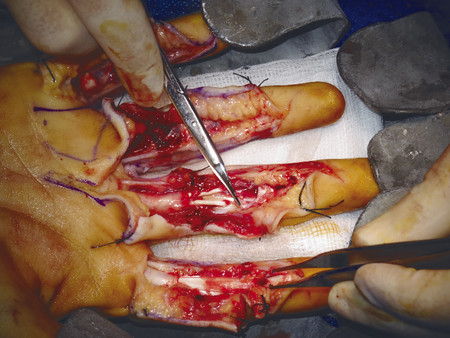
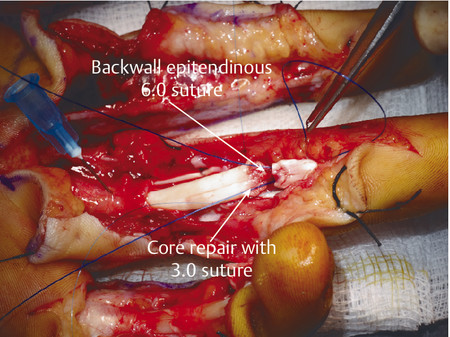
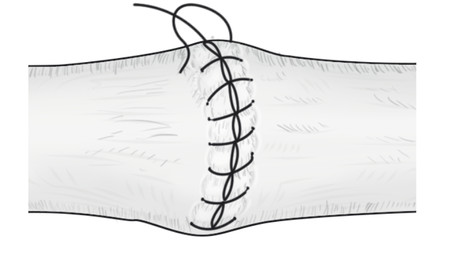
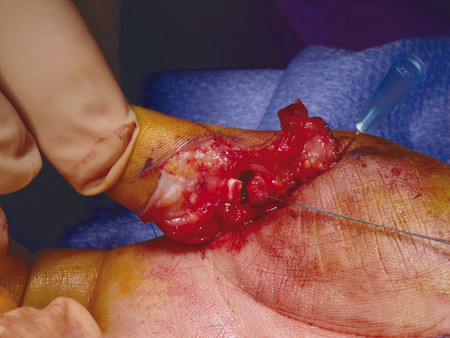
In the case illustrated earlier, a midlateral incision was performed to repair the damaged structures in zone 2 (Fig. 7‑5, Fig. 7‑6, Fig. 7‑7, Fig. 7‑8, Fig. 7‑9, Fig. 7‑10, Fig. 7‑11, Fig. 7‑12). Generally, a four-strand modified Kessler repair is performed for the core stitch to minimize the gapping and an epitendinous repair provides an additional 25% strength to the tendon repair (Fig. 7‑13, Fig. 7‑14). At least a 10-mm bite should be taken with the core suture to provide optimal strength. The blood supply to the flexor tendons is dorsal with a relatively avascular volar zone. One should try to preserve the pulleys, mainly the A2 and A4, but, not at the cost of limiting tendon glide. Some surgeons advocate venting to facilitate glide after repair. Indeed, sometimes it is necessary to vent the entire A4 pulley for tendon repair; as long as the A2 pulley is preserved, tendon bowstringing is minimized. Furthermore, in some cases it is not possible to repair both FDS tendons as this will impede FDP excursion, and increase the work of flexion. A dorsal plaster of Paris is used to protect the repair at the end of the procedure (Fig. 7‑15).

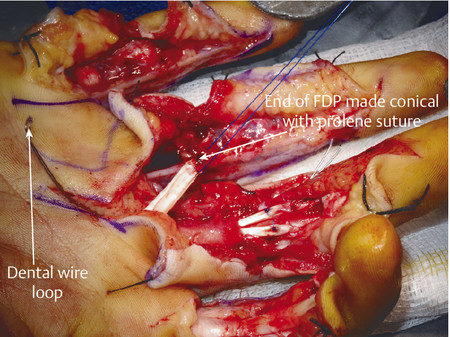
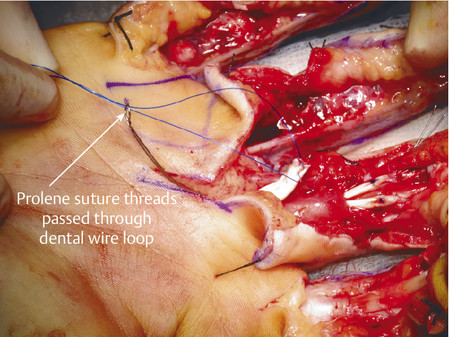



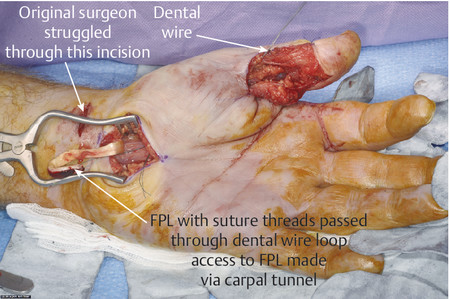
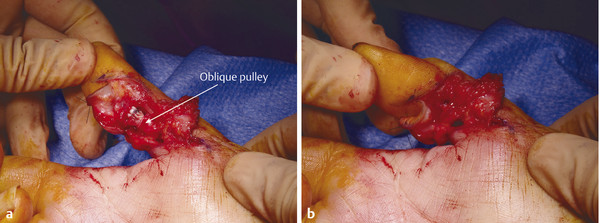
The same principles of tendon repair apply with the flexor pollicis longus (FPL) repair; however, access is best achieved through Bruner-type incisions (Fig. 7‑16, Fig. 7‑17). The FPL can retract to the carpal tunnel and the dental wire technique for retrieval is useful (Fig. 7‑18). Once retrieved, the FPL should be repaired with a four-strand modified Kessler and epitendinous repair with preservation of the oblique pulley to prevent bowstringing (Fig. 7‑19).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree