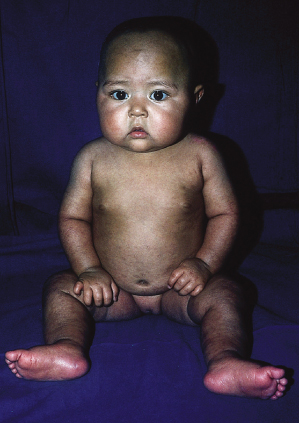
In kwashiorkor, the classic skin changes consist of areas of hyperpigmentation and occasional fissuring (‘enamel paint’) in areas subject to pressure (Figs 65.3, 65.4). Other cutaneous manifestations are erythema, desquamation, thinning, petechiae, ecchymosis and purpura (Fig. 65.5).
Fig. 65.3 Kwashiorkor: severely affected child with desquamation, crusts, hyperpigmentation and skin necrosis.

The most frequent cutaneous alterations in 100 infants with kwashiorkor were shiny varnished-like skin (64%), dark erythematous pigmented macules (48%), xerotic ‘crazy-paving’ skin (28%), residual hypochromia (21%), large-scale desquamation (18%), hyperchromia (11%) and erythema (11%) [12].
Superimposed bacterial and mycotic (Candida) infections are seen in approximately 75% of patients with kwashiorkor. The hair is sparse, thin and depigmented. Periodic episodes of malnutrition cause bands of normal pigmentation and discoloration in the hair known as the ‘flag sign’ (Fig. 65.6).
In both marasmus and kwashiorkor, primary and secondary cutaneous lesions may occur [13]. The non-specific histopathological features include epidermal atrophy, hyperkeratosis and occasionally acanthosis.
Management.
The management of the acute phase of protein-energy malnutrition frequently needs a multidisciplinary approach. The skin lesions in malnutrition regress as soon as the child receives adequate dietary intake or the inducing factors (infection, malabsorption, malformation, etc.) are corrected.
Dietary supplementation with linoleic acid and zinc is important. During the acute phase, the cutaneous lesions should be treated with lubricating ointments. If bacterial infection is present, a topical antibacterial agent is indicated. Superimposed candidal infection should be treated with appropriate topical agents.
Prognosis.
The prognosis of severe protein-calorie malnutrition in infants has improved in recent years. An overall mortality of less than 10% is reported in most centres. The usual causes of death are diarrhoea and bronchopneumonia. In uncomplicated malnutrition the mortality is below 5%.
With adequate treatment, the prognosis of the mucocutaneous lesions is excellent (Figs 65.7, 65.8).
References
1 Kliegman RM, Behrman RE, Jenson HB, Stanton BF. Part V Nutrition. In: Kliegman: Nelson Textbook of Pediatrics, 18th edn. Philadelphia: W.B. Saunders, 2007.
2 Altinkaynak S, Selimoglu MA, Ertekin V, Kilicarslan B. Serum ghrelin levels in children with primary protein-energy malnutrition. Pediatr Int 2008;50:429–31.
3 Amadi B, Fagbemi AO, Kelly P et al. Reduced production of sulfated glycosaminoglycans occurs in Zambian children with kwashiorkor but not marasmus. Am J Clin Nutr 2009;89:592–600.
4 Mosby TT, Barr RD, Pencharz PB. Nutritional assessment of children with cancer. J Pediatr Oncol Nurs 2009;26:186–97.
5 Van den Broeck J, Willie D, Younger N. The World Health Organization children growth standards: expected implications for clinical and epidemiological research. Eur J Pediatr 2009;168:247–51.
6 Vujic D, Petrovic M, Radovanovic LJ et al. Uporedni pregled nutricionog statusa bolesnika lecenih hemodijalizom i peritoneumskom dializom. Srpski Arhiv Za Celokupno Lekarstvo 1991;119:194–7.
7 Raya Muñoz J, Arroyo Nieto A, del Arbol JL et al. Valoración del estado nutricional en pacientes ingresados en un servicio de Medicina Interna. Rev Clin Española 1991;188:178–84.
8 Fattal-Gemman M. L’immunocompetence chez les personnel agées. Ann Pharm Franc 1992;50:13–24.
9 Larrea J, Torrent JM, Altabas MT et al. Consecuencias inmunológicas de la desnutrición:valoración con multitest. Nutr Hosp 1991;6:94–7.
10 Chandra RK, Sarchielli P. Nutritional status and immune responses. Clin Lab Med 1993;13:455–61.
11 Good RA, Lorenz E. Nutrition and cellular immunity. Int J Immunol 1992;14:361.
12 Lowy G, Meilman I. Kwashiorkor. Aspectos clinicos e dermatológicos. Med Cut ILA 1975;3:181–92.
13 Ruiz-Maldonado R. Cutaneous manifestations of malnutrition and trace element deficiencies. In: Caputo R, Gelmetti C (eds) Proceedings of the 5th International Congress of Pediatric Dermatology. Milan: Cilay-Pharma, 1989.
Fatty Acid Deficiency
Deficiencies of essential fatty acids are seen in low-fat diets, severe malabsorption, long-term parenteral nutrition and mostly in association with protein-energy malnutrition. Essential fatty acids (linoleic, linolenic and arachidonic) have multiple functions; in the skin, they contribute to the formation of lamellar granules [1]. Essential fatty acids are unsaturated fatty acids that must be obtained from the diet. Cutaneous manifestations of fatty acids deficiency are dry, scaly and leathery skin, with underlying erythema, intertriginous erosions and alopecia. Systemic features include growth failure, abnormal liver and kidney function, poor wound healing and delayed skin hypersensitivity. Treatment is with essential fatty acids replacement. The prognosis depends on the severity of co-existing nutritional deficiencies [2,3].
References
1 Prendiville JS, Manfredi LN. Skin signs of nutritional disorders. Semin Dermatol 1992;11:88–97.
2 Friedman Z. Essential fatty acids revisited. Am J Dis Child 1980;134:397–408.
3 Abushufa R. Essential fatty acid status in patients on long term home parenteral nutrition. J Parenter Enteral Nutr 1995;19:286–91.
Vitamin Deficiencies
Vitamins are organic elements that, in minimal amounts, act as catalysts of cellular metabolic processes essential for the adequate functioning and growth of tissues [1]. Both excess and deficiency of vitamins may cause mucocutaneous alterations. In industrialized countries, vitamin deficiencies are usually due to metabolic or organic disorders, and excess of vitamins is usually iatrogenic. In developing countries, vitamin deficiencies are mainly of dietary origin and are linked to malnutrition.
The mucocutaneous alterations caused by vitamin deficiencies are discussed below.
Vitamin A
Vitamin A is a fat-soluble vitamin abundant in milk, liver and animal fats. The major dietary and cellular forms of vitamin A are retinol, retinol ester, β-carotene, retinaldehyde and retinoic acid [2].
In developed countries, two-thirds of vitamin A intake consists of preformed retinol (retinol ester) of animal origin. In developing countries, provitamin A, carotenoids of vegetables and fruits are the predominant source of vitamin A; 6 µg of carotene is equal to 1 µg of retinol, and the daily requirement for children is 500–1500 µg. Deficiency of vitamin A is diagnosed by determining the plasma concentration of retinol [2].
Vitamin A plays an important role in the functioning of eyes, the immune system and skin. At the molecular level, it stabilizes membranes. Excess or deficiency of vitamin A may cause the breakage of lysosomal membranes. Vitamin A promotes the early inflammatory response, synthesis of collagen and angiogenesis. Its most important role in the skin relates to cornification and keratinization [2,3].
Cutaneous lesions caused by vitamin A deficiency consist of follicular papules with a central keratotic plug, primarily located on the extensor extremities. This finding must not be confused with keratosis pilaris (see Chapter 123), a common autosomal dominant skin disorder that is not related to vitamin A deficiency. The skin may also be dry and scaly, and the hair sparse and fragile. Ocular abnormalities include night blindness in mild vitamin A deficiency and xerophthalmia, Bitot spots and keratomalacia leading to blindness, particularly in children with severe vitamin A deficiency. Vitamin A deficiency has been associated with high morbidity and mortality from infection, particularly from measles [3,4]. Supplements of vitamin A (400 000 IU) are an inexpensive and effective way of preventing death and complications in children with measles.
Excess of vitamin A of dietary origin is extremely rare. Most cases are due to oral therapy. The main cutaneous manifestations are erythema, skin fragility, desquamation, mucosal dryness and diffuse alopecia. Lethargy, anorexia and weight loss are seen in patients with hypervitaminosis A. Radiological bone changes and painful limbs are conspicuous in children [5].
Carotenoderma is the orange–yellow skin pigmentation due to high intake of β-carotene that is the natural provitamin A. It is a frequent condition in children, which disappears when dietary habits are regulated [5] (see Chapter 171).
Vitamin B2 (Riboflavin)
Riboflavin is a hydrosoluble vitamin that is abundant in foods of animal origin, green leaf vegetables and yeasts. It is a component of the co-enzymes flavin mononucleotide and flavin–adenine dinucleotide, which are involved in a number of metabolic pathways and oxidative phosphorylation. The daily requirement for children is 1–1.5 mg. Riboflavin deficiency is diagnosed through measurement of erythrocyte glutation reductase.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree