6 Breast-Conserving Therapy: Decision-Making and Anticipating the Unfavorable Aesthetic and Functional Result
The Goals of Breast-Conserving Therapy
The goals of traditional breast-conserving therapy (BCT) include tumor resection with negative margins, nodal assessment when indicated to direct adjuvant chemotherapy, and the bedrock concept separating BCT from mastectomy, the preservation of healthy breast parenchyma with the maintenance, if not the improvement, of breast aesthetics. When these goals are met the oncologic safety of breast conservation therapy is as irrefutable today as it was when it was introduced following the Milan Trials more than 20 years ago. Combining tumor removal, whether lumpectomy, partial mastectomy, quadrantectomy, or segmental mastectomy (choose your term; they are all loosely defined) with adjuvant radiotherapy is without question an effective method for treating stage I or II breast cancer. The results of multiple studies have demonstrated parity between BCT and mastectomy in regard to overall and disease-free survival. 1 – 5 This remains true as long as a certain subset of patients are avoided, namely those with multicentric or multifocal disease.
Tumor resection with negative margins leads to recurrence-free and disease-free survival.
Of course, the factors that predispose patients to recurrence following BCT will equally predispose an equivalent population treated with mastectomy to recurrence. 6 These factors include young age at recurrence, intrinsic tumor characteristics, not performing chemotherapy, and a failure to achieve adequate surgical margins. 6 – 8
The appeal of BCT to a large proportion of the breast cancer population is also clear. The promise of outpatient surgery in most cases, a smaller scar, no surgical drains, and preservation of the majority of the patient’s breast—and what is most important, the nipple-areola complex (NAC)—is a welcome option for many. Certainly, the perception that BCT represents cumulatively “less treatment” is one that is difficult to refute with the nonmedical patient population.
When Does the Promise of Breast-Conserving Therapy Fail to Deliver?
Unfortunately, the dual goals of maximum disease-free survival and the preservation of breast aesthetics don’t always follow a parallel course. Although several studies over the last twenty years have demonstrated good to excellent aesthetic results of BCT in well over 85% of the patients being treated, these studies typically used the treating physicians as the judges of the outcomes and did not include input from the patients being treated. 9 , 10 In more recent studies that included an assessment of cosmesis by the patients, nearly 100% of patients noted asymmetry and 28% to 35% of the patients reported dissatisfaction with the aesthetic results of their treatment. 11 , 12 These studies would indeed suggest that the simultaneous goals of adequate oncologic treatment and the maintenance of breast aesthetics are not easily obtained, but rather represent competing interests. 13
The definition of success in the treatment of early-stage breast cancers has evolved beyond the simplistic outcomes of low recurrence rates and patients embracing the early perception of “less treatment” as it applies to BCT versus mastectomy. Without long-term patient satisfaction with all of the outcomes of care, including excellent overall and disease-free survival, acceptable breast aesthetics not limited to symmetry, and increasingly, the concept of functional breasts, treatment can hardly be defined as complete and successful. 12 , 14 By “functional breasts” we mean that there is adequate symmetry of breast volume, shape, and the breast footprint, 15 including the inframammary fold (IMF) position. This allows the patient to comfortably and confidently wear any type of bra and clothing without resorting to the use of external prostheses, specially constructed undergarments, or bulky outer clothes. 16

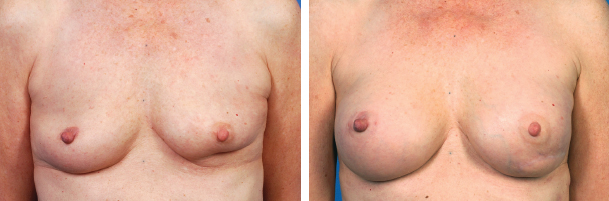
As a result of a lumpectomy and radiotherapy in the inferior pole of her right breast, this patient developed asymmetry of volume and shape as well as a discrepancy in the position of her inframammary fold, making it difficult to keep her bra strap in place.

This patient underwent BCT to the right breast that led to a volume asymmetry requiring her to wear a 250 cc partial prosthesis to feel comfortable in clothing.
A cancer-free patient whose IMFs differ in height by 3 cm will probably have difficulty wearing a bra, because the bra strap will ride up on the side with the lower IMF, causing discomfort and requiring constant adjustment. Equally, a patient enjoying her ninth disease-free year after cancer treatment who needs to wear a 250 cc external prosthesis to feel that her breasts are symmetrical in clothing may not be as satisfied with her “breast preservation” as hoped for at the beginning of her treatment. 11 , 17 A patient left with a glaring contour deformity, even if it is only visible when she has no clothes on, may still cringe at the sight of her breasts every time she changes clothes or looks down in the shower years after her “oncologically successful” treatment. It is hard to imagine that these patients can ever truly move past their cancer history because of the daily reminders. 18 , 19
We have entered a new era of patient expectations in regard to the results of breast cancer treatment and breast reconstruction. In part, this is because of the blurring of lines between the results seen in patients treated with risk-reducing mastectomy for genetic disorders and those treated for actual cancer. Of course, the challenges of reconstruction in someone who is spared chemotherapy, radiotherapy, and even the sacrifice of her NAC in a risk-reducing procedure are far less than the challenges in treating a patient with cancer. Increasingly, a large subset of women have the expectation that their breasts will not only look the same after cancer treatment, but indeed expect an improvement in the shape, ptosis, and perceived size of their breasts. Although this expectation has in part been created by treating surgeons, the proliferation of information on the Internet and in cancer support groups has contributed as well. 20
Today’s patients have an expectation that their breasts will not only look the same after cancer treatment but will also have an improvement in shape, ptosis, and perceived size.
Predicting a Poor Aesthetic Result in BCT: Managing Dead Space
One of the most difficult questions plastic surgeons are asked by patients deciding between BCT and mastectomy with reconstruction is “Will my breast look okay after a lumpectomy and radiation?” 21 This question cannot be answered by a simple “Yes” or “No.” This question is often left to the plastic surgeon by the treating breast surgeon who will actually be performing the resection. This ostensibly occurs because of an understanding that if the patient is dissatisfied with her result, it is the plastic surgeon who will be relied on for advice and further treatment. Complicating the challenge of predicting the aesthetic results of another surgeon’s resection is the difficulty of predicting the impact of the radiotherapy that must accompany lumpectomy for satisfactory oncologic care. Although this team-oriented approach is ultimately beneficial for the patient, it is helpful if all members of the team are sensitive to factors that have an impact on final cosmesis.
Box 6-1 Predictive Patient and Surgical Factors for Treatment After BCT
Estimated volume of the tumor relative to the overall breast
Location of the tissue to be resected
Patient’s desire for a change in the size of her breasts
Potential for the creation of direct contact between deep dermis and fascia
Fortunately, there are several straightforward predictive factors that can be assessed before any surgery that can help to identify the course of treatment that will provide the patient with the highest degree of satisfaction.
This patient stated that she had wanted larger breasts for many years, but she had focused on her cancer care related to treatment of a left breast cancer. After BCT, a muscle-sparing latissimus dorsi flap reconstruction was followed by bilateral breast augmentation with implants. Placement of the breast implants was delayed until after the introduction of nonirradiated, healthy tissue from the back into the irradiated breast.
It is essential to ask the patient whether she has any desire to change the size of her breasts, either larger or smaller. For a patient who wants larger breasts, BCT alone will always fail to satisfy. For a patient who wants to reduce the size of her breasts, a breast reduction executed as part of an oncoplastic approach is far preferable to a breast reduction done months or years after BCT, when the breast has already been irradiated. 22 , 23

This patient with small breasts had a relatively modest 80 g lumpectomy that resulted in significant asymmetry.
The surgeon must also consider the size of the proposed resection relative to the overall volume of the patient’s breast. This is ultimately a question of dead space. The reality is that significant dead space within a soft tissue construct like the breast will ultimately collapse, resulting in distortion of the breast architecture. 13 , 24 In smaller-breasted patients, the removal of as little as 12% to 20% of their overall breast volume can create a volume discrepancy that is aesthetically unpleasant and functionally difficult. Resection of up to 30% of the total breast volume may be tolerated in larger-breasted women without the need for reconstructive techniques. However, these patients should still be informed that a symmetry procedure may be required on the opposite breast to permit comfortable bra fitting. The increased use of preoperative imaging in the planning of breast cancer surgery has facilitated our ability to truly assess the volume of tissue that will need to be resected to obtain adequate margins. 14 , 25 – 28
Even small resections can lead to significant distortion of the breast when the tissue is removed from aesthetically sensitive areas. These areas include the superomedial breast or cleavage area and the area directly under the NAC. One should also consider what the likely effect of radiotherapy will be on the position of the NAC as tissue retracts during healing from surgery, as fibrosis occurs following radiation, or both. Resections immediately adjacent to the NAC will often result in retraction of the NAC as the dead space adjacent to the NAC collapses.

This patient underwent resection of a tumor, leaving the deep dermis in contact with the fascia, which led to nipple retraction after healing and radiotherapy. Autologous fat grafting of the right breast and a contralateral mastopexy improved her symmetry and reduced the retraction.
The resection of a specimen that leaves no breast tissue between the dermis and the serratus or pectoral fascia will inevitably result in adherence of the dermis to the fascia once healing occurs. In cases where the specimen is resected from the extreme lateral or inferior borders of the breast, the defect may not be severe. However, virtually everywhere else in the breast, this adherence can cause NAC distortion or contour deformities of the breast itself.
Anticipating the Impact of Radiotherapy
The addition of radiotherapy to lumpectomy is a key component of BCT in most patients. However, it is the addition of radiotherapy to the milieu that is considered by many to be one of the least predictable influences on the development of breast deformity and asymmetry after treatment. 29 , 30 Several patient factors that most surgeons agree contribute to worse outcomes after BCT include breasts that are smaller, more ptotic, and have a higher proportion of fatty tissue than glandular tissue. 31
The total prescribed radiation dose, including higher boost irradiation energy, can have a negative impact on long-term cosmesis. 32 In addition to total dosage, the radiation delivery technique has been further evaluated and is a distinct variable. The use of accelerated partial-breast irradiation (APBI) using three-dimensional conformal radiotherapy versus whole-breast irradiation has also been found to have an adverse impact on cosmesis at 3 years after treatment as well as progressive deterioration of breast cosmesis. 33 However, other studies with significantly smaller study groups have found that APBI delivered through brachytherapy results in better cosmesis than whole-breast irradiation. 34 The fractionation schedule of whole-breast irradiation may also play a role, at least in terms of acute skin toxicity. Hypofractionated whole-breast irradiation, or delivery of the dose over a shorter time frame, results in fewer acute and short-term skin toxicities than conventional fractionation. 35 , 36 The long-term correlation of these findings to overall breast cosmesis and pain-free survival has not been confirmed.
Radiotherapy delivery factors to be considered include APBI versus whole-breast irradiation; external beam radiotherapy versus brachytherapy; and a hypofractionated versus a conventional fractionated delivery schedule.
Can Radiotherapy be Avoided?
It has been found that patients over 70 years of age who have estrogen receptor–positive breast tumors will likely have similar survival outcomes, with or without the inclusion of radiotherapy after lumpectomy. 37 The results of BCT in such a patient group would be significantly more predictable. Patients with collagen vascular disease, particularly scleroderma or active systemic lupus, have an enhanced response to radiation, with aggressive development of radiation-induced fibrosis in their tissues. 38 These patients are not considered candidates for BCT. Women with a previous history of mantle irradiation for the treatment of Hodgkin’s lymphoma who present with breast cancer should at least be engaged in a frank discussion of the possibility of contralateral cancer developing at some point and what the role of mastectomy might be in reducing that risk. 39 Although BCT may be considered in these patients, the impact of additional radiotherapy should be weighed carefully.
Managing Expectations and Shared Decision-Making
As noted earlier, the consultation process when helping a patient decide between BCT and mastectomy with reconstruction does not usually end in an easy “Yes” or “No” answer. In breast reconstruction the wishes, expectations, and tolerance of treatment that patients bring to their care affect many of the choices that are made. It is essential to gain an understanding of the patient’s overall tolerance of possible asymmetry in her breasts, potential contour deformities in the treated breast, the strength of her desire to preserve breast tissue, and the possibility of delayed partial breast reconstruction months or years after completion of oncologic treatment. This information is used in conjunction with a reasonable assessment of what the aesthetic impact of BCT will be on a patient’s breasts, given the parameters discussed previously, to present a picture of what might be required to obtain satisfactory results if BCT is pursued versus a mastectomy with or without reconstruction.
The surgeon must assess the patient’s overall tolerance of potential breast asymmetry and contour deformities in the treated breast, the strength of her desire to preserve breast tissue, and the possibility of partial breast reconstruction delayed for months or years later. For an optimal outcome, the patient must be included in the decision-making regarding her treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








