5 Flexor Tendon Injuries (Zone 3–5)
Abstract
Flexor tendon injuries within zones 3 to 5 represent those confined to the palm and distal forearm. They can be debilitating with resultant loss of basic hand function. A thorough understanding of the anatomy, surgical approach, reconstructive options, and rehabilitation is required to provide the best opportunity for functional recovery in these anatomic regions. Proper exposure with identification and repair of neurovascular structures and repair of injured tendons with sound surgical technique can ensure successful outcomes and recovery.
5.1 Description
The majority of literature on flexor tendon injury focuses on the management of zone 2 lacerations. Although much of this is applicable to flexor tendon injuries in other zones, several key differences exist between zones. Surgeons must be familiar with these differences when evaluating, treating, and rehabilitating patients with zones 3 to 5 flexor tendon injuries.
5.2 Classification
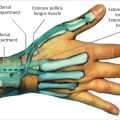
The classification of the zone of injury is through the following standard anatomical boundaries: zone 3 marks the area of the palm between the carpal tunnel and the flexor tendon sheath, or from the distal aspect of the transverse carpal ligament to the proximal border of the A1 pulley; zone 4 describes the area within the carpal tunnel; and zone 5 is from the proximal border of the transverse carpal ligament to the musculotendinous junction in the proximal forearm See Fig. 4.1.
5.3 Key Principles
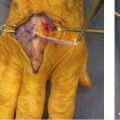
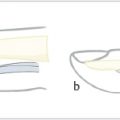
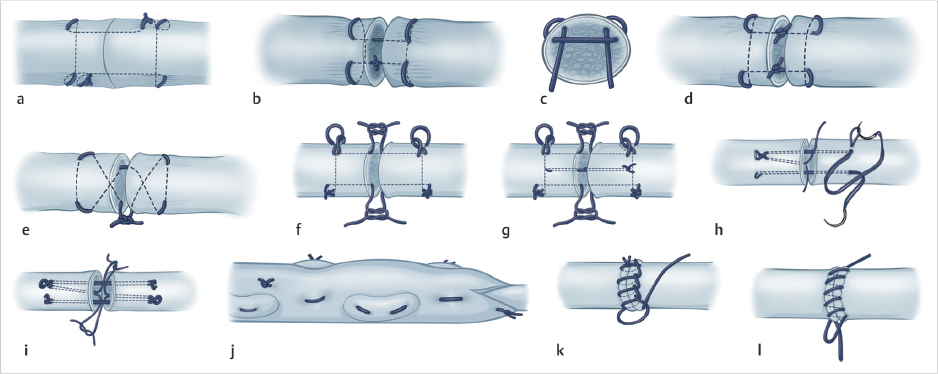
Given the close proximity of tendons, nerves, and blood vessels in the hand and forearm, combined injuries are common, and there should be a low threshold for surgical exploration and identification of the surrounding neurovascular structures. Primary tendon repair is preferred and possible in the majority of zones 3 to 5 injuries. A minimum of a four-strand repair and an epitendinous suture is recommended (► Fig. 5.1). Early active motion rehabilitation protocols should be employed to optimize functional outcomes after these injuries.
5.4 Expectations
Zones 3 to 5 injuries are more forgiving than zone 2 injuries due to excellent tendon nutrition, a bed that is less prone to adhesions, and fewer surrounding retinacular structures, thereby easing repair and promoting tendon gliding. As such, good to excellent outcomes in range of motion and tendon function should be expected. However, concomitant neurovascular injury can complicate recovery and functional outcomes after such combined injuries. 1 , 2
5.5 Indications
Complete lacerations or > 60% transection of the flexor tendons in zones 3 to 5.
5.6 Contraindications
Contraindications include severe multitissue injuries to the hand and fingers, contaminated wounds, significant soft tissue loss over the flexor system, and patients that are unable to participate in rehabilitation. These instances may require staged tendon repair or reconstruction after an adequate wound bed and soft tissue coverage have been established.
5.7 Diagnosis
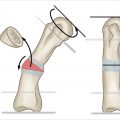
Similar to other zones, complete transection of a flexor tendon in zones 3 to 5 will present with inability to flex the digit at the interphalangeal joints along with loss of the natural resting cascade of the hand (► Fig. 5.2). Given the close proximity of the vascular palmar arch and neurovascular bundles, detailed examination of the peripheral nerves and vessels around the zone of injury and distally is imperative. The Allen’s test must be performed when examining pulses as retrograde flow through palmar arches may mask vascular injuries. There should be a low threshold for surgical exploration as innocuous lacerations may hide the extent of deep structural injury, and the preoperative examination is often unreliable in these patients. 3

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree