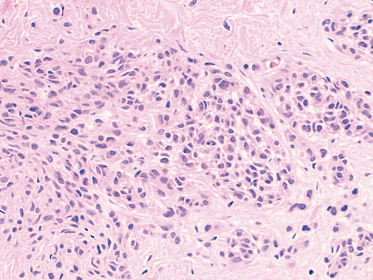
Fig. 4.2 High-power view of naevus cells in the dermis showing regular cells with monomorphic dense nuclei and ample pale eosinophilic cytoplasm.
The blue naevus is a dermal lesion composed of finely branching melanocytes containing cytoplasmic melanin granules situated between the collagen bundles of the upper and mid-dermis. The cellular variant is a much larger nodular lesion often found on the buttocks and consisting of nests and fascicles of pale staining melanocytes together with islands and bundles of spindle and epithelioid cells with abundant cytoplasm and little pigment.
References
1 Mirago N. The relationship between melanocytic and peripheral nerve sheath cells. Part 1: melanocytic nevus (excluding so-called ‘blue nevus’) with peripheral nerve sheath differentiation. Am J Dermatopathol 2000;22:217–29.
2 Herron MD, Vanderhooft SL, Smock K et al. Proliferative nodules in congenital melanocytic nevi: a clinicopathologic and immunohostochemical analysis. Am J Surg Pathol 2004;28:1017–25.
3 Barnhill RL, Cerroni L, Cook M et al. State of the art, nomenclature, and points of consensus and controversy concerning benign melanocytic lesions: outcome of an international workshop. Adv Anat Pathol 2010;17:73–90.
4 Magro CM, Crowson AN, Mihm MC Jr et al. The dermal-based melanocytic tumor: a categorical approach. J Am Acad Dermatol 2010;62:469–79.
Dermal Nodules
The dermal nodule carries a wide differential diagnosis both clinically and histologically. Dermal nodules are usually surgically excised by a general or a plastic surgeon. The most common is the pilomatrixoma which has a characteristic histological appearance with nests of basaloid cells and eosinophilic ghost cells. Calcification occurs in more than two-thirds, and is usually in the ghost cells. A foreign body giant cell reaction is common (Fig. 4.3).
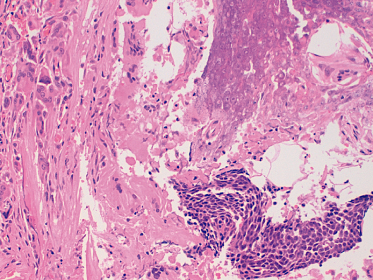
Fig. 4.3 Photomicrograph of a high-power field from a pilomatrixoma showing an island of basaloid cells in the bottom right half of the field, lightly calcified ghost cells in the top right-hand field and a collection of foreign body giant cells on the left.
Spindle cell lesions carry a wide histological differential diagnosis and may need immunostaining for confirmation. Neural tumours can usually be diagnosed without difficulty, and express S-100 protein (Fig. 4.4). The dermatofibroma (also called fibrous histiocytoma) can show a wide variety of appearances depending on which components predominate: fibroblast-like cells, histiocytes, some of which may be xanthomatous or multinucleate, or blood vessels. Immunostaining for factor XIIIa and D2-40 demonstrates strong diffuse immunoreactivity in the spindle cells [1]. Juvenile xanthogranulomas show different appearances depending on the age of the lesion, with early lesions being predominantly mononuclear followed by the classic Touton cell-rich stage and finally a stage with a spindle cell pattern and a variable component of mononuclear and multinucleated cells. Immunostaining shows positivity for CD68, fascin, factor XIIIa and α1-antitrypsin. The myofibroma consists of characteristic short fascicles of plump spindle-shaped cells separated by thin bundles of collagen. Vascular spaces resembling those of a haemangiopericytoma are often found in the centre, giving most lesions a biphasic pattern. Necrosis, hyalinization, calcification and focal haemorrhage may also be present in the centre. Immunostaining is positive for vimentin and smooth muscle actin. Dermatofibrosarcoma protuberans extends into the subcutis and is composed of bundles of small spindle cells with plump nuclei in a characteristic storiform or cartwheel pattern. Scattered mitoses are present but atypical mitoses are rare. Immunostaining for CD34 shows 50–100% of cells to be positive. Staining for factor XIIIa is negative. The Gardner fibroma is a bland hypocellular proliferation of spindle cells and haphazardly arranged collagen (Fig. 4.5).
Fig. 4.4 Photomicrograph of a field from the middle of a nerve sheath tumour which presented as a dermal nodule. Note fascicles of spindle cells with the fascicles tending to run in the same direction. Immunostaining for S-100 protein was positive.
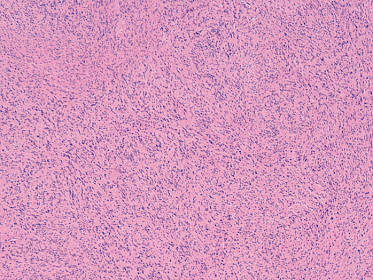
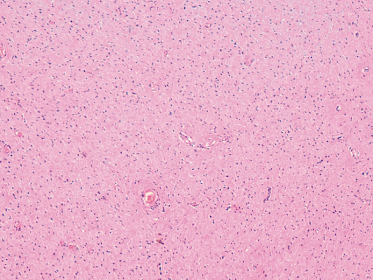
Fig. 4.5 Photomicrograph of a field from the middle of a Gardner fibroma which presented as a dermal nodule. Note hypocellularity of lesion, haphazardly arranged collagen bands and spindle cells.
Granuloma annulare demonstrates one or more areas of necrobiosis surrounded by histiocytes and lymphocytes in the superficial and mid-dermis. Variable numbers of multinucleate giant cells are present. In some cases the histological changes are subtle and there are no formed areas of necrobiosis.
Reference
1 Bandrchi B, Ma L, Marginean C et al. D2-40, a novel immunohistochemical marker in differentiating dermatofibroma from dermatofibrosarcoma protuberans. Mod Pathol 2010;23:434–8.
Vascular Lesions
A very important part of the workload in paediatric dermatopathology consists of the diagnosis of vascular cutaneous lesions. Many larger lesions undergo needle biopsy by an interventional radiologist prior to definitive treatment. The International Society for Vascular Anomalies classification identifies two categories of superficial vascular anomalies in infancy and childhood: vascular malformations and vascular tumours.
Vascular malformations are divided into two groups: fast-flow and slow-flow, based on clinical and radiological findings and are classified histologically according to the predominant type of vessel involved: lymphatic, venous, arterial or mixed – involving any combination. Most fast-flow cutaneous malformations are arteriovenous malformations
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








