4 Flexor Tendon Repair (Zone 2)
Abstract
Zone 2 flexor tendon lacerations are notoriously difficult injuries to manage and have historically led to poor outcomes after attempted repair. Even with excellent tendon repair, complications such as adhesion formation, rupture, and stiffness remain possible. Thus, a thorough understanding of surgical anatomy and technique is required. The goal of repair is accurate coaptation of the tendon ends with sufficient strength to allow early postoperative rehabilitation; a strong and smooth surgical repair will also reduce the likelihood of adhesion formation. Because of the importance of postoperative therapy, patient selection, compliance, and education must not be overlooked.
4.1 Description
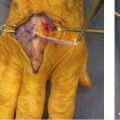
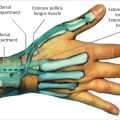
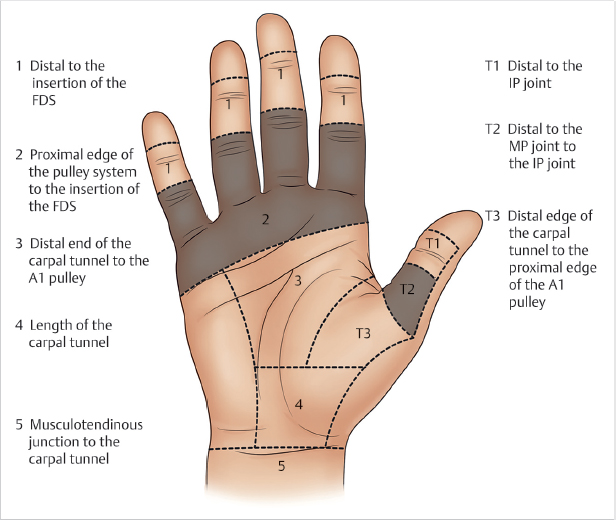
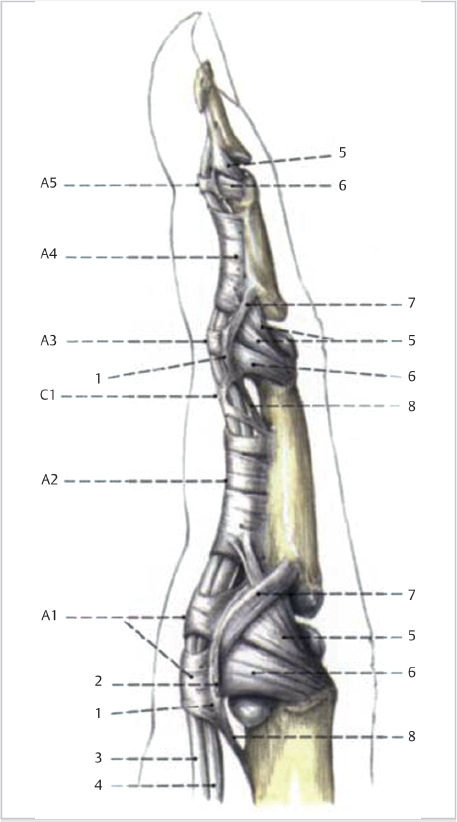
Zone 2 flexor tendon injuries occur between the A1 pulley proximally and the flexor digitorum superficialis insertion distally (► Fig. 4.1). In this region, the flexor digitorum superficialis and profundus tendons lie within a tight fibro-osseous sheath with a series of pulleys that prevent bowstringing (► Fig. 4.2). Within this sheath, the two tendons are covered by fibrous epitenon. Together, the fibro-osseous sheath and epitenon play a critical role in the smooth gliding of the tendon. The superficialis is split by the profundus and its two slips turn sideways and insert on the middle phalanx in an upside-down manner.
Zone 2 was historically named “no man’s land” because injuries here invariably led to adhesion formation and poor outcomes. However, in the 1960s, Kleinert and others first reported good outcomes after primary repair, stressing the importance of meticulous atraumatic surgical technique and early postoperative rehabilitation. 1 Subsequent advancements in suture technique, design, and postoperative therapy have drastically improved outcomes. 2 , 3 , 4 , 5
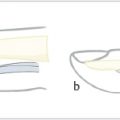
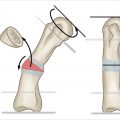
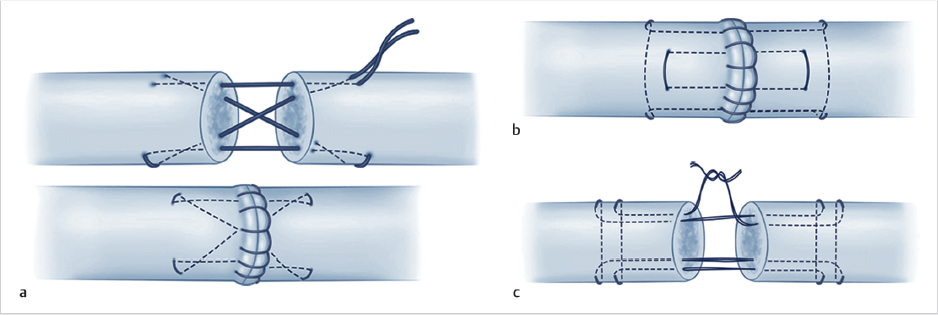
As described by Strickland, core sutures should have the following characteristics: easy placement, secured knots, smooth juncture at tendon ends, minimal gapping, minimal interference with vascularity, and sufficient strength to permit early motion. 6 Although there are many core suture techniques, it is known that multiple suture strands (> 4) provide superior load to gapping and failure. 7 Classic suture techniques such as the Kirchmayr and modified Kessler are still common; however, newer techniques such as the Strickland, Cruciate, Becker, and Winters-Gelberman are becoming more common due to increased repair site strength 7 (► Fig. 4.3). A peripheral epitendinous suture is recommended to increase repair site strength and reduce gapping. 8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree