This article presents a review of 3D video analysis for use in patients with facial paralysis. The difficulties inherent in quantifying the degree of facial paralysis and the effect of therapeutics that has led to the use of videos and computer-assisted 3D analysis are discussed, which can yield quantifiable results of treatment, allow the description and quantification of facial paralysis, and become a tool in the planning of operative procedures. The authors provide a step-by-step overview of video analysis, and present case studies from two specific techniques they have used in reconstruction surgery.
The exact local extent and degree of facial paralysis as well as their implications on the different functions of the mimetic muscle system, on the aesthetic appearance of the face, and on the patient`s sequelae are difficult to assess. The authors’ first experiences with the International Muscle Transplant Registry had shown that the traditional scoring systems for facial palsy are not suitable for an exact and scientific evaluation. As a consequence the authors concentrated research on the possibilities of 3-dimensional (3D) measuring of movements in the face during standardized mimic activities initially using a VICON videosystem, and later a digital caliper (Faciometer) developed in tight cooperation with the Laboratory for Biomechanics of the Swiss Federal Institute of Technology, Zurich.
However, from the beginning it was the authors’ aim to document the facial movements by taking standardized videos and to quantify the facial movements by computer-assisted 3D analysis of the video film. This idea was realized by a completely new development.
Methods
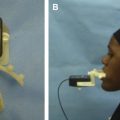
The equipment consists in its entirety of a system for taking videos in front of two special mirrors arranged at a sharp angle, a calibration grid, a digital video camera, and a computer workstation. For this system the video is transferred to the hard disk to prepare the selected sequences by an editing program for analysis. When the real image and the two mirror images in all single pictures have been analyzed point by point by the computer, these final data are stored on a compact disk (CD). A visualization program gives easy access to the stored data.
Taking the Video
At first the standardized static and dynamic points to be measured are marked in the face. The 3 static points (tragus points of both sides and the central nose point) define a triangle, to which all dynamic points are related during the facial movements. The definitions of the static and dynamic points are explained further in an article published in 1994. To calibrate the system a calibration grid is brought between the two mirrors and is filmed. Afterwards, the head of the patient is positioned between two mirrors arranged at a sharp angle. By this method a frontal image and side-view mirror images from the left and right side of the patient`s face are taken by the camera, including all marked points. All standardized facial movements are now recorded by the video camera 3 times:
- 1.
Maximal lifting of the eyebrows
- 2.
Closing of the eyes as if for sleeping
- 3.
Maximal closing of the eyes
- 4.
Maximal showing of the teeth
- 5.
Maximal closing of the eyes and showing of the teeth at the same time
- 6.
Smiling with showing the teeth
- 7.
Smiling with closed lips
- 8.
Pursing the lips and whistling
- 9.
Pulling the corners of the mouth downwards.
To document the influence of the facial palsy on speech the video with sound track is continued, while the patient counts from 1 to 10 and pronounces his or her name and address.
3D Analysis of the Video
After transferring the digital video film from the camera to the computer picture by picture, all static and dynamic points of the face in the frontal and the two mirror views are marked with the cursor of the mouse in a constant order indicated by the program. The measurement has to be calibrated by doing the same to one picture of the calibration grid and its two mirror images. After this has been done for all standardized facial movements, the data are recorded on a CD.
Visualization of Patient Data
A visualization program gives easy access to the data. The change of the distance over time of any 2 standardized points can be shown on a graph for each of the standardized movements and for both sides of the face. An exact measurement can be performed at each phase of the movement. Parallel to this a video clip of this movement can be reviewed, or the picture of the resting face and the picture of the maximum of this movement can be seen. A qualitative documentation in the video clip occurs in parallel with a quantitative measurement.
By way of 2-dimensional (2D) graphs, the movement of each dynamic point is visualized for each of the movements. The movement of all points can be shown 3-dimensionally at the same time and for each of the standardized facial movements.
Changes in speech can also be observed on the acoustic track by comparison of the recordings during the different video sessions.
Results
The design of the mirror system has been shown to be suitable for children as well as for different sizes of adults. The dimensions and the angle between the two mirrors has never limited the possibility to have the frontal view and both mirror images of the face on the same picture.
The algorithm to reconstruct the 3D points used is a modified Tsai algorithm. This algorithm compensates the lens distortion but not the distortion of the mirrors. If 2 points with a distance of 50 mm are measured, the accuracy of the distance is better than ± 0.25 mm. If the distance is smaller, the accuracy is even better. The reproducibility of a point is better than ± 0.2 mm.
Results
The design of the mirror system has been shown to be suitable for children as well as for different sizes of adults. The dimensions and the angle between the two mirrors has never limited the possibility to have the frontal view and both mirror images of the face on the same picture.
The algorithm to reconstruct the 3D points used is a modified Tsai algorithm. This algorithm compensates the lens distortion but not the distortion of the mirrors. If 2 points with a distance of 50 mm are measured, the accuracy of the distance is better than ± 0.25 mm. If the distance is smaller, the accuracy is even better. The reproducibility of a point is better than ± 0.2 mm.
Discussion
Most techniques to document and measure facial movements developed during the past 10 years are not able to give a detailed insight into the actual function of the facial muscles. Even in recent reports on the functional outcome of large series of free muscle transplantation for facial paralysis, the authors’ documentation system was not used for functional assessment although it was published as early as 1994. Information indicates that the authors were the first to use 3D tracing of skin surface markers to analyze facial movements for the first time; this technique was published in 1992 followed by a more extensive description in 1994. At that time the authors also developed the Faciometer, an electronic caliper system for easy clinical application. This simple instrument for 3D measurements fulfilled an important role during standardized quantification of facial paralysis and its improvement by surgical treatment within the International Registry for Neuromuscular Reconstructions in the Face. Because of disadvantages, including the necessary contact with the skin of the patient, the patient-fatiguing process of measuring, the missing possibility of later data analysis, and the missing correlate to the quality of the facial movements, the authors pursued further development and refinement of the system.
The new mirror system was the great breakthrough, because it was the basis for 3D analysis of a video. Instead of multiple cameras, the two mirrors add two perspectives of the moving face. The frontal view of the face together with the two mirror images on one video film are not only used for 3D measurements of the different standardized facial movements, but also give an insight into the quality of the facial movements from 3 different views at the same time. A very complex computer program has been developed for analysis of the videos.
Visualization of the analyzed data is easy and quick for all movements recorded. The movement of a selected single point in the paralyzed side of the face can be displayed on a 2D graph (x,y; x,z; or y,z axes) and compared with the corresponding point on the healthy side. The changes of the distance between any 2 points documented can be shown on a graph for any of the facial movements. Selecting a representative distance for each of the facial movements is important. In the authors’ opinion this kind of presentation, together with pictures of the resting position and position of maximum movement, seems to be ideal for publication of a functional result for a patient. A video clip of every movement can be reviewed and stopped at any point in time during the movement, to be studied in more detail. 3D graphs of the displacement of all registered points during a selected facial movement give a good survey on the dynamics of the face, the degree of asymmetry, and on synkinesis eventually initiated by this facial movement.
Clinical experience
Decision-Making Process with the Help of 3D Video Analysis, Part One: Dynamic Reconstruction of Eye Closure by Muscle Transposition or Functional Muscle Transplantation?
Using the aforementioned technique the authors performed the first quantitative study of 3D preoperative and postoperative eyelid movements in patients treated for facial paralysis. Between February 1998 and April 2002, 44 patients were treated for facial palsy, including reconstruction of eye closure. Temporalis muscle transposition to the eye was used in 34 cases, and a regionally differentiated part of a free gracilis muscle transplant after double cross-face nerve grafting was used in 10 cases. Patients’ facial movements were documented by the authors’ video-analysis system preoperatively and 6, 12, 18, and 24 months postoperatively. For this comparative study, only the data of patients with preoperative and 12-month postoperative measurements were included ( Figs. 1–4 ).