3 How Much Space Do I Need?
Abstract
How much space do I need? The amount of space needed for a dermatology clinic is inherently dependent on the program, and determined by the number of providers and staff, types of services offered, the anticipated productivity, and other special requirements. Various configurations of clinical and support areas may be used depending on physician preferences and desired workflow. The program matrix presented in this chapter is an interactive tool that can assist in figuring the number of rooms recommended in the clinical area, and reception desks in the reception area based on the number of staff and patients attended to per hour. The spatial matrix then follows, using assumptions from the program matrix to help determine the square footages for every room and for the dermatology clinic in total. These areas are often required by building code or have been calculated by recent trends in health care design. Engaging the appropriate professional can be instrumental in identifying these trends and evaluating the specific needs for each type of dermatology practice.
Top 10 Things You Need to Know
An ideal dermatology clinic design delivers a patient-focused experience without compromising functionality or operational efficiency.
Flexibility and adaptability are key design considerations when planning for multiple lines of service or multiple providers.
The initial step in space planning involves determining the number of providers, support staff, and the anticipated productivity (patients per hour) of the clinical team.
The general rule of thumb for medical and surgical dermatology practices is three to four examination/procedure rooms per provider.
Planning for nonclinical support space such as reception areas, restrooms, break rooms, and storage areas will follow.
Identifying the necessary number of rooms and support spaces without regard for room size is known as building a program. This is the starting point for working with your architect.
The amount of space necessary may also vary depending on the organizational pattern chosen. The ideal configuration varies based on your workflow priorities.
Spatial planning guidelines can assist in converting the program into a range of square footage, which will assist the dermatologist and architect in quantifying the necessary space.
Federal, state, and local regulations, as well as the American with Disability Act (ADA) regulations, will dictate some requirements of the medical office.
Engaging an architect experienced with outpatient health care can be instrumental in identifying the specific needs for each type of dermatology practice.
3.1 Introduction
An ideal dermatology clinic design delivers a patient-focused experience without compromising functionality or operational efficiency. Whether 2,000 square feet (sf) or 20,000 sf in size, layout and workflow have a direct impact on productivity and patient experience. Flexibility and adaptability of spatial configuration are key design considerations when planning for multiple lines of service or multiple providers. Defining the number of providers (physicians and extenders) and types of services are the first steps in determining how much space is necessary. Planning for nonclinical support space and choosing the ideal configuration will follow. Spatial planning guidelines can then assist in converting these considerations into a range of square footage, which will assist the dermatologist and architect in quantifying the necessary space.
aBuilding occupancy is the classification provided to structures primarily for building and fire code enforcements. Building and fire codes vary by location, and typically result from a combination of federal, state, and local ordinances. The International Building Code (IBC) is the most commonly used building code in the United States of America. According to IBC, a doctor’s office is classified as a Business Occupancy.
3.2 Number of Providers and Workflow
The initial step in space planning involves determining the number of providers, support staff, and anticipated productivity (patients per hour) of the clinical team. How many physicians and physician extenders will use the space? Will the providers work full-time and be present in clinic at the same time, or part-time with varying schedules such that the clinic rooms may be shared? Once built, the clinic design and size become limiting factors in the revenue potential of a particular site. Thus, determining how many providers the space needs to accommodate, and whether there is any room in the site and budget to build additional space for potential future growth, become considerations of utmost importance.
The number of providers and their anticipated schedules determine the planned workflow for the practice and the relationships between clinical areas and support spaces, such as laboratories, storage rooms, offices, restrooms, and administrative areas. The general rule of thumb for medical and surgical dermatology practices is three to four examination/procedure rooms per provider. Nurses’ stations and restrooms (staff and patient) will vary in number and size according to the number of staff and anticipated number of patients, which affect the occupancy of the building. 1 The following two scenarios illustrate the relationship between efficiency and spatial needs:
In scenario 1, two full-time providers work simultaneously. The typical clinical program would require six to eight examination rooms, two nurses’ stations, and two offices or dictation rooms to be shared by both providers.
bIn recent years, many physicians have replaced nonrevenue generating office space with revenue generating spaces, such as examination or procedure rooms. Rather than a dedicated office, some providers prefer smaller, more centralized spaces where they can process clinical notes between patient visits to improve efficiency.
The nonclinical program would consist of a waiting room, restrooms, and support spaces, which are generally determined by the number of patients and staff, and have no direct relationship to the number of examination rooms provided. Federal, state, and local codes are used to help in determining the minimum spatial requirements for these nonclinical spaces, and adequate space must be allotted to pass necessary inspections and obtain a license for occupancy.In scenario 2, two providers work on a part-time basis and are never in the practice at the same time. While the number of examination rooms, nurses’ stations, and dictation rooms can be cut in half, waiting spaces, restrooms, and general support spaces typically cannot due to building codes and federal standards such as ADA standards for accessible design. Regulatory codes will dictate clearances and minimum room sizes, and sometimes vary little even if the number of patients attended to in the practice is doubled. For example, the area requirement for a toilet room is the same whether 40 or 80 patients will use it on any given day.
Spatial calculations take into account the throughput (number of patients per hour) of the staff and providers as well as their schedules. 2 Since space is typically at a premium with regard to practice costs, every effort should be made to utilize space efficiently across the work week. Anticipating the day-to-day workflow of a medical practice is critical to establish the spatial configuration and planning of the new medical office.
3.3 Service Type
In dermatology space planning, there are generally four areas of focus: medical (including pediatric), surgical, cosmetic, and dermatopathology (often occurs in a separate space and will not be considered here). A practice may have a particular focus in one area, or may need space for multiple lines of service within the same clinic. The amount of space needed for clinical and support areas is directly related to and varies with the services rendered. In multiple-provider practices that provide a mix of services, the best layout for clinical areas may be grouped pods of standard-sized examination rooms with fewer, shared procedure rooms, whereas in surgical or procedural-heavy practices, larger procedure rooms that also suffice as examination rooms constitute the bulk of clinical space. In cosmetic-heavy practices, waiting rooms become more spacious, equipment storage space with direct access to the treatment rooms improves workflow and flexibility, and a retail space is usually incorporated into the spatial program. Consequently, when considering a combination of any of these subspecialties of dermatology, flexibility, and adaptability become key design considerations as they directly impact efficiency and workflow.
3.4 Spatial Configurations and Design Organizational Patterns
It often helps to think of zones or groups of areas with similar functions when laying out the plan for a new practice. The four different spatial configurations presented (▶Fig. 3.1, ▶Fig. 3.2, ▶Fig. 3.3, ▶Fig. 3.4) are examples of how the clinical and nonclinical functions of a dermatology practice may be arranged in ways that best serve the type of service and workflow anticipated, typically predetermined before the planning phase begins. Patient flow is shown in red, staff flow is shown in orange, and provider flow is in green.
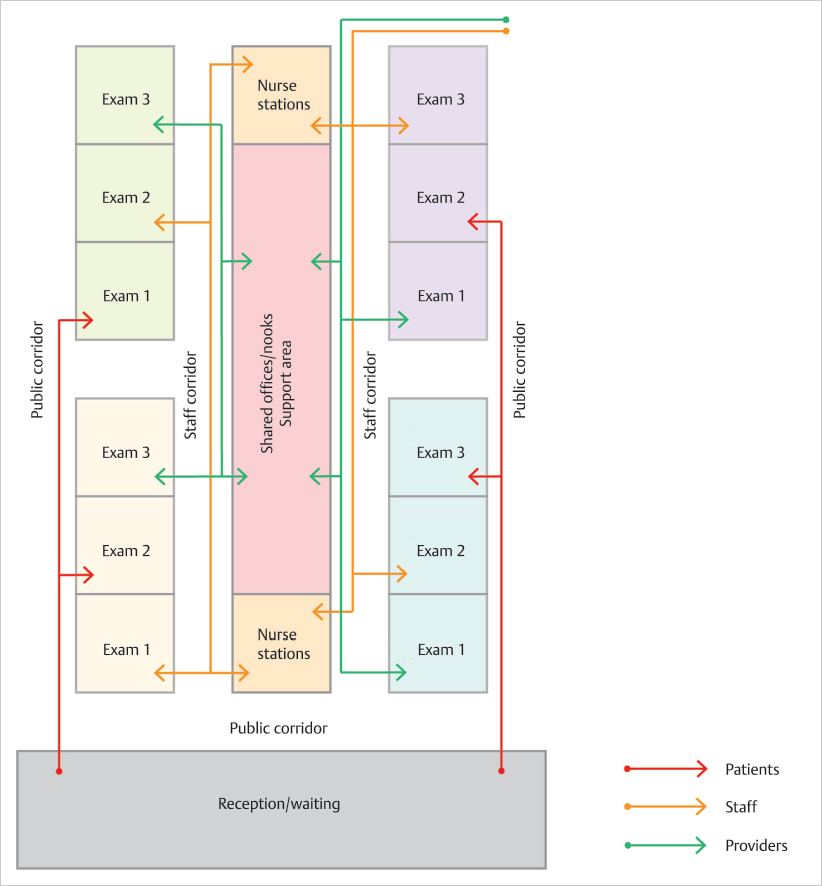
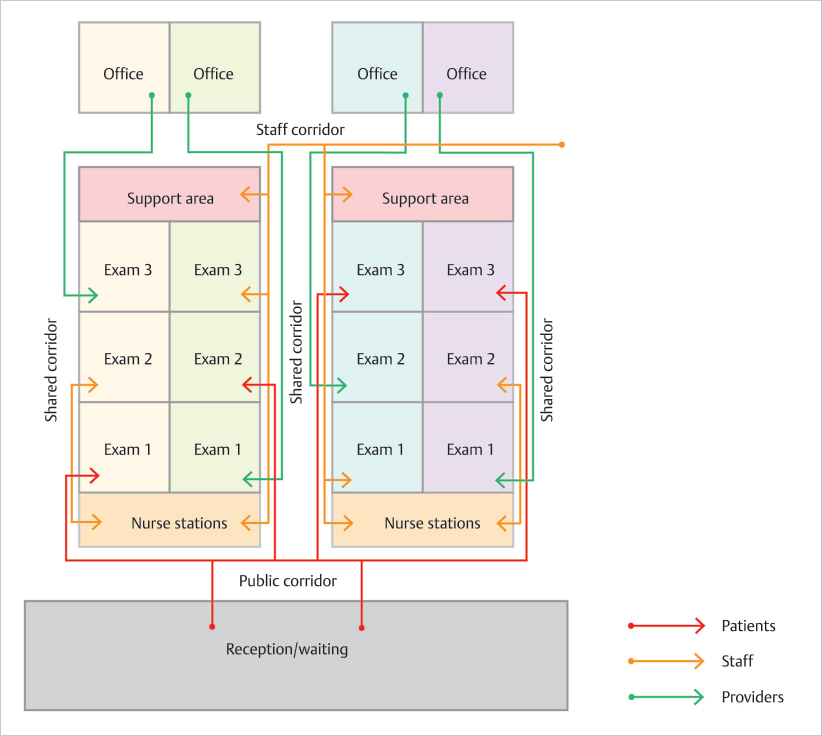
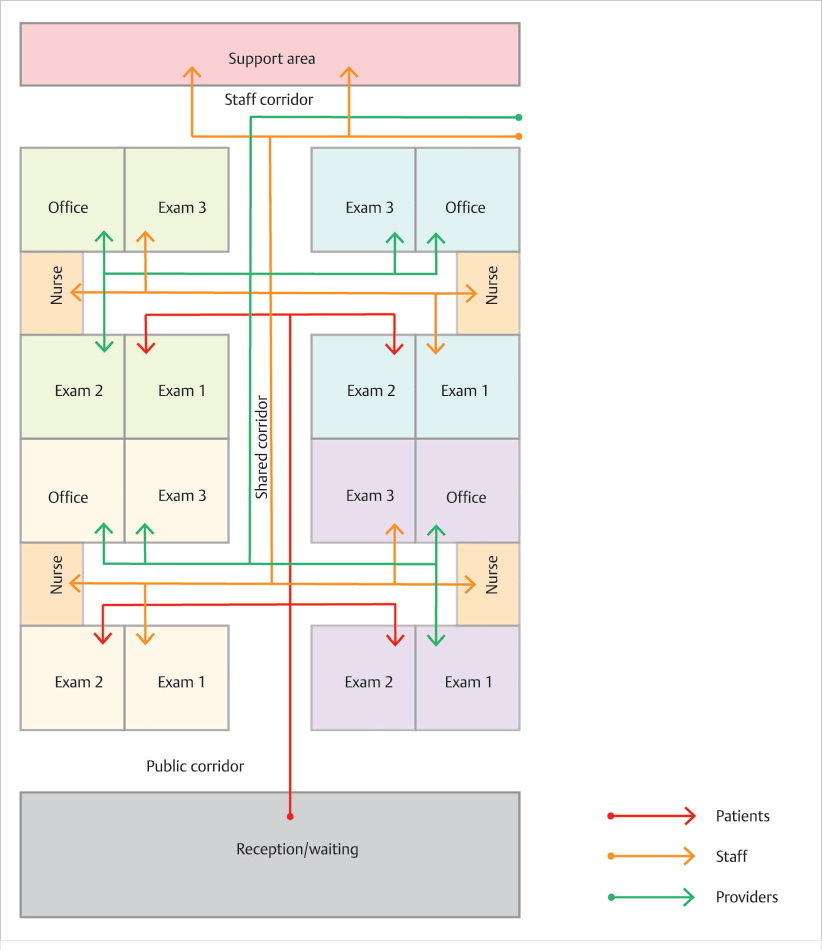
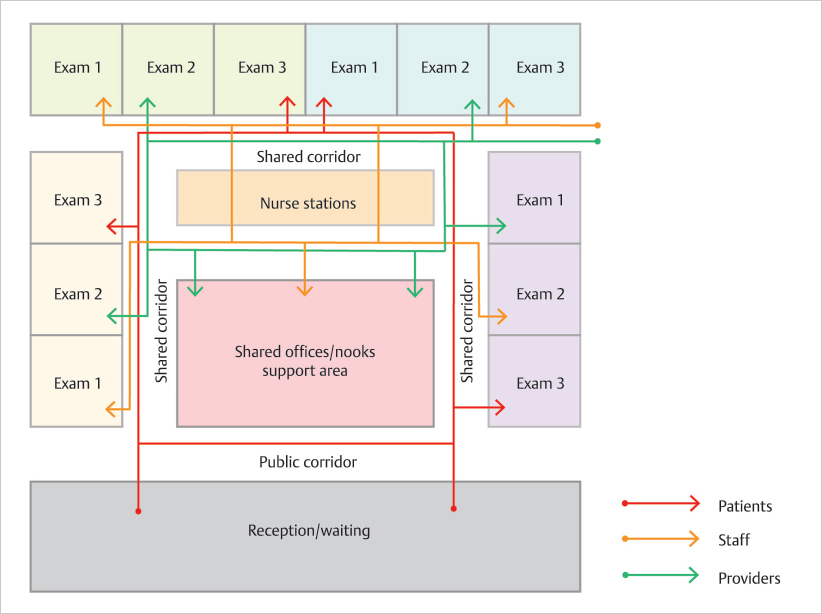
Areas for examinations and procedures are shown grouped according to providers, while workspaces such as physicians’ nooks or dictation rooms, instrument processing rooms, supply storage, restrooms, and laboratory spaces are assigned as support areas. The nurses’ stations are zoned separately, as they often function as a bridge between the public/waiting areas and the examination/procedure rooms. Both support areas and nurses’ stations should be designed with regard to the fewest number of steps necessary between the most frequently used spaces to optimize efficiency. 3
Visualizing different flow patterns between patients, staff, and providers at this stage will help make adjustments to better accommodate the workflow desired within the amount of space available. Each configuration has advantages and disadvantages, and your priorities may steer you toward a particular configuration. For example, is there flexibility in the number of examination rooms per provider? How important is it for the examination rooms to have access to natural light? Or is it important to separate patients from staff and providers?
The amount of space necessary may vary depending on the organizational pattern used. 4 Axial and cluster configurations take the most area, as a result of the number of corridors, but allow for a more controlled circulation and a clear separation of provider/staff areas from the patient/public areas. This contrasts with the radial configuration, where the less restrictive circulation allows for more flexibility of use, better visual connection between patients and staff, and a smaller footprint.
Consider which rooms you would prefer to have window access. In the grid pattern, providers’ offices are prioritized for exterior views and natural light intake. In the axial and cluster arrangements, the examination rooms tend to be placed internally, thus they are without windows. This layout compromises exterior views but improves patient privacy. The radial pattern, on the other hand, prioritizes patient views by placing the majority of the examination rooms on the perimeter and support rooms centrally.
3.5 Clinical and Support Areas Needed
Becoming familiar with the spaces required in a medical office prior to meeting with your architect will expedite the planning process. According to the guidelines of hospitals and outpatient facilities, the following clinical and support areas shall be provided regardless of the spatial configuration chosen: (1) examination, treatment, or procedure rooms, or a combination of these; (2) support areas for these clinical rooms, such as nurse station, clean supply storage, soiled holding room, equipment and supply storage, clean linen and soiled linen holding area, and laboratory spaces when applicable; (3) support areas for patients such as toilet rooms; (4) support facilities such as janitorial closets, and engineering and maintenance service rooms such as electrical closets, mechanical rooms, and telecommunications equipment room; (5) public and administrative areas such as vehicular drop-off and pedestrian entrances, reception, waiting space, public toilet rooms, interview space, or an area where private communications with patients shall be situated away from public areas; (6) equipment and supply storage; (7) staff lounge and toilet room(s); (8) space for business or nonclinical work; and (9) medical record storage when applicable.
Examination rooms should be accessible to the nurses’ station and patient toilet room(s), and have a minimum clear floor area of 90 sf.
cThe typical examination room has become larger in order to accommodate a computer station, in addition to accompanying family members or interpreters. The optimal examination room size is 10 ft x 10 ft (approx. 100 sf), although slight variations can occur without affecting the function of the room. For procedure rooms, especially in Mohs surgery suites, the optimal size is 12 ft x 12 ft (approx. 144 sf), where the examination table is centered in the room. Smaller rooms such as 8 ft x 10 ft or 9 ft x 9 ft, which used to be the common examination room size, are optimal for quick examinations such as surgical follow-up visits. In these configurations, the examination tables are placed at an angle or against a wall.
When centrally located, examination tables should have a 2 feet 8 inches clearance around the entire table. A documentation area (written or electronic) should be provided in each examination room, and at least one hand washing station should be provided for each of the four examination rooms.With regard to support spaces for examination rooms, the recommendations are as follows: (1) the nurse station shall include a work counter, communication system, space for supplies, and accommodation for written or electronic documentation; (2) when applicable, work areas for preparing, dispensing, and administering medications, including work counter, handwashing station, lockable refrigerator, lockable storage for controlled drugs, and sharps containers; (3) a space for clean supply storage
dSuch space can be in a room or cabinet located in or close to the nurse’s station.
; (4) a space for medical/hazard waste holding roomeMedical waste shall be disposed in clearly labeled containers, preferably separate from patient areas with direct access to the exterior, where it can be picked up by third-party vendors.
; (5) equipment and supply storage, including wheelchair and emergency equipment storage; (6) clean linen storage and soiled linen holding areafFor clean linens, the storage area can be in a dedicated room or cabinet located in or close to the nurse’s station. For soiled linens, the holding area can be separate or shared with hazard/medical waste, where it can be picked up by third-party vendors.
; and (7) when applicable, a space for soiled instruments and/or instruments processing room. 5Although these guidelines provide the general criteria for design of a medical facility, it is important to note that federal, state, and local regulations, as well as ADA regulations, will dictate some requirements of the medical office. Other aspects enforced by the regulatory codes are as follows: height and location of counters; size and location of toilet rooms; width of hallways; accessibility and clear floor space (wheelchair turnaround diameter) in examination/procedure rooms, workspaces, toilet rooms, etc.; width of door openings (32 inches minimum); and wall mounting heights, among other requirements.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





