3 Flexor Tendon Repair (Zone 1)
Abstract
Zone 1 flexor tendon injuries encompass several different types of repair techniques. Considerations for zone 1 flexor tendon injuries include surgical approach, tendon retrieval, and tendon repair. Depending on the injury pattern, fracture fixation, tendon-to-bone repair, or tendon-to-tendon repair may be required. When repair fails or is not feasible, additional salvage techniques may be necessary.
3.1 Description
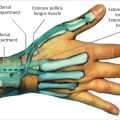
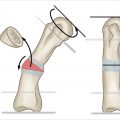
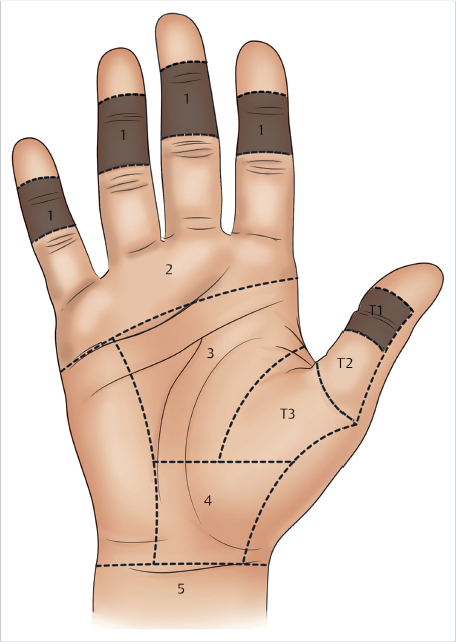
A zone 1 flexor tendon injury is an injury to the flexor digitorum profundus (FDP) tendon that is between the flexor digitorum superficialis (FDS) insertion on the middle phalanx and the FDP insertion on the distal phalanx (► Fig. 3.1). There are several techniques and methods of fixation for zone 1 flexor tendon lacerations. Fixation options include direct tendon-to-tendon repair, use of bone tunnel, or a bone anchor. The method of repair is dependent on the presence of an adequate distal tendon stump, presence and size of segmental tendon defect, and surgeon preference.
3.2 Key Principles
The flexor tendon should be repaired without tendon advancement of more than 1 cm, which may result in the quadriga effect (inability to completely flex the fingers due to the tethering of one, preventing full excursion of the adjacent fingers). The goal is to achieve fixation able to withstand early motion rehabilitation.
3.3 Indications
Zone 1 flexor tendon injuries should be repaired in the majority of patients with a viable digit. In patients with severe or chronic injuries, an FDS-only digit can be managed with distal interphalangeal (DIP) joint fusion; however, most cases allow for an attempted FDP repair or reconstruction.
3.4 Contraindications
Primary zone 1 FDP repair is contraindicated in otherwise nonviable digits. Relative contraindications include patients with severe segmental tendon damage as well as patients that cannot participate in therapy. Primary repair may not be technically feasible in patients with a chronic FDP laceration with significant retraction.
3.5 Special Considerations
Patients with acute flexor tendon injuries should be treated surgically within 1 week of the injury, if possible. Delay in repair can result in adhesion formation and may reduce tendon excursion. This may make mobilization for repair more difficult intraoperatively and limit motion postoperatively. Adequate repair technique allowing for early postoperative motion is important to maximize outcome after surgery. 3 , 2 This should be monitored and therapy protocols adjusted depending on patient progress.
3.6 Special Instructions, Positioning, and Anesthesia
The patient should be positioned supine with the extremity on a hand table. Wide awake local anesthesia with no tourniquet allows for patient participation to actively test the repair, tendon gliding, and joint motion, which minimizes the risk of postoperative rupture. 3 With sedation, the patient may be awoken enough to test the repair. General anesthesia is also an option, although the surgeon will not be able to evaluate the repair integrity intraoperatively.
3.7 Tips, Pearls, and Lessons Learned
If the tendon is retracted within or proximal to the A4 pulley, incising the flexor sheath proximal to the area of retraction allows access to the tendon stump. The tendon can be advanced by carefully pushing the tendon forward through the sheath. This can be done by using two forceps to alternately grasp and advance the tendon to feed it distally. Alternatively, a passing suture can be placed through the tendon and retrieved with a suture passer through the A4 pulley.
A milking maneuver with the wrist in flexion can help advance the tendon distally. When this is ineffective, a separate zone 3 incision may be required. A suture passer or pediatric feeding tube can be passed from distal to proximal through the flexor sheath. The proximal tendon stump can be sutured to the feeding tube or looped through the suture passer, which is then pulled back through, thus pulling the tendon distally.
Trimming the end of the tendon, if frayed or bulbous, may allow for easier passage through the sheath or pulley. The tendon can be held in place with a syringe needle placed transversely through the A4 pulley capturing the tendon within the pulley. This will help prevent retraction of the tendon for an easier repair.
If the level of repair is close to the A4 pulley, the tendon must not be too bulky in order to glide through A4 easily. If there is difficulty, the distal aspect of A4 can be vented with a longitudinal incision without significant functional consequences. 4 , 5 This is best assessed with the patient wide awake and actively flexing the digit.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree