27 Surgical Approaches to the Midface Complex
Introduction
Correction of the aging midface is an integral component of comprehensive facial rejuvenation. This central feature has largely been ignored through most of the history of facial plastic surgery. However, over the past 20 years midfacial rejuvenation has evolved as a versatile and indispensable adjunct to the field of facial plastic surgery. This chapter defines midface anatomy and the aging changes of the midface, reviews the history of midface procedures, and describes the common approaches currently utilized for rejuvenation.
Anatomy
Knowledge of the layers of midface and structures contained within is essential to understanding aging changes and their correction. The boundaries of the midface include the inferior orbital rim and nasojugal groove superiorly, the melolabial fold inferomedially, and the zygoma laterally. The layers of the midface in the superior aspect differ from the layers within the inferior aspect. Starting from the “floor” to the “roof” of the superior midface, the layers include the bone, periosteum, preperiosteal fat, suborbicularis oculi fat (SOOF) pad, orbicularis oculi and facial muscles (levator labii superioris alaeque nasi, levator anguli oris), subcutaneous fat, and skin. In the lower midface the layers include the bone, periosteum, facial musculature (zygomaticus major and minor), malar fat pad, subcutaneous fat, and skin ( Fig. 27.1 ).
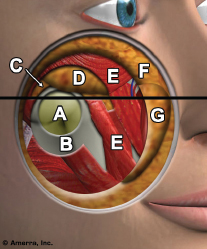
The layers of the midface attenuate and fuse inferomedially to form the melolabial or nasolabial crease. The malar fat pad is located between the inferior border of the orbicularis and the melolabial fold. This malar fat has been found to be anatomically indistinguishable from the subcutaneous fat of the infraorbital cheek skin. Sasaki and Cohen 1 performed cadaver studies that indicated the greatest average depth of the malar fat pad was ∼6 mm, whereas the thickness at the melolabial fold was 2.2 mm. There are no demonstrable connections between the malar fat pad and the underlying superficial musculoaponeurotic system (SMAS) in this area.
In addition to these layers, three fascial connections are present that serve to attach the dermal roof to the bony floor. This includes the lateral orbital thickening, which is a broadly based band over the frontal process of the zygoma, the orbicularis retaining ligament, which separates the prezygomatic space from the preseptal space of the lower eyelid, and the zygomaticcutaneous ligaments, which originate from the inferior aspect of the zygoma ( Fig. 27.2 ). For purposes of review, the prezygomatic space is bounded by these three ligaments, and the preseptal space is the tissue plane between the orbital septum and the orbicularis oculi. 2 The lateral orbital thickening and the orbicularis retaining ligament condense with one another and serve as a durable anchor that tethers the midfacial structures from a superolateral position. Penetrating through the periosteum and preperiosteal fat, the second division of the trigeminal nerve ramifies into the cutaneous sensory branches of the midface.
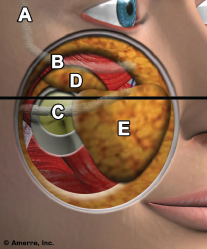
Sensory innervation of the midface is supplied by the second division of the trigeminal nerve (infraorbital nerve) along with the zygomaticofacial and zygomaticotemporal nerves. Sacrifice of the infraorbital nerve should be avoided as it is usually accompanied by permanent dysesthesia of the midface. Preservation of the zygomaticofacial and zygomaticotemporal nerves is also preferable, although the resultant sensory deficit tends to be temporary.
Aging Changes
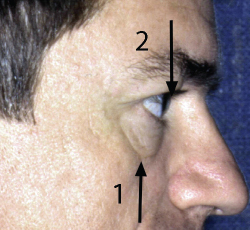
Specifically, there are seven anatomical changes that signify midface aging: exposure of the nasojugal groove, paucity of soft tissue over the inferior orbital rim, presence of a double convexity of the lower eyelid/cheek complex, loss of malar fullness, increased distance from the lower eyelid to the malar fat pad, an inferomedial descent of the malar fat pad resulting in a deepening of the nasolabial fold, and a lateral infraorbital crescentic hollow. Often this is accompanied by a pseudoherniation of the orbital fat, which will accentuate the lower eyelid/cheek double convexity and prominence of the orbital rim (Figs. 27. 3 and 27.4).
This compromise of the anatomical integrity is attributable to a combination of factors, including solar damage, thinning of the dermis, redistribution or atrophy of fat, gravitational forces, obesity, and heredity. The result is inferomedial descent of the midface structures, tethered superolaterally by the lateral orbital thickening and the orbicularis retaining ligament. This movement occurs against the melolabial fold, deepening the crease and augmenting the prominence with redundant tissue. Superiorly, the malar fat migration contributes to the crescent-shaped hollow below the lower edge of the orbicularis oculi muscle, deepens the nasojugal groove, and makes the infrazygomatic cheek concavity more prominent. The anatomy of midface ptosis has also been well described by Lucarelli et al. 3 They demonstrated that attenuation of the orbitomalar, zygomatic, and masseteric cutaneous ligaments occur, but that midface ptosis results mainly from the inferior migration of skin and attached malar fat pad with relative sparing of the deeper tissues.
Patients less commonly present with malar bags; however, this chapter does not cover that topic in great depth. Malar bags represent excessive edema of the skin/subcutaneous tissues, manifesting as a bullae over the malar prominence, whereas malar festoons are the result of redundant orbicularis muscle below the orbital rim. Direct excision remains the primary treatment for bothersome malar bags, replacing this tissue redundancy with a thin scar. Laser resurfacing has also been used to address mild to moderate malar bags with mixed results, and a series of two or three fractionated laser treatments showing more promise. Extended blepharoplasty via a skin/muscle flap approach has been noted to provide some correction for both malar bags and festoons.
To adequately assess the midface, standard frontal, oblique, and lateral photographs of the face are essential. A bird’s eye view (i.e., a view from the top of the patient’s head, aligning the chin and nasal tip) is often helpful as a comparison of midface position for preoperative and postoperative views. On frontal views, the distance from the lower eyelid margin to the beginning of the soft tissues of the youthful midface is comparable with the distance from the eyelid to the infraorbital rim. This distance increases with age and the surrounding structures descend, contributing to the double convexity of midface aging ( Figs. 27.3 and 27.4 ).


Additionally, when this double convexity is prominent, one should make note as to whether the lateral view shows the orbital rim to be posterior, anterior, or on the same plane of the cornea. If the plane of the orbital rim is posterior to the anterior plane of the cornea, the patient is said to have a negative vector, indicating that orbital fat repositioning, fillers, or malar augmentation are excellent options for lower eyelid and midface restoration ( Fig. 27.5 ). When a negative vector is present, these patients are often at risk for scleral show, which may be exacerbated by orbital fat removal. Ideally, the infraorbital region manifests a smooth convexity that masks the underlying infraorbital rim and nasojugal groove. 4 Fullness of the malar eminence is desirable as it will accentuate the eyes, and this feature is commonly emphasized in the application of makeup. As darkness gives the appearance of recession and light gives the appearance of coming forward, the application of a makeup that is darker than skin color underneath the malar eminence gives the illusion of an elevated cheek. Similarly, lighter makeup in the nasojugal groove can help hide the shadow of the valley or depression.
History
Midface rejuvenation has evolved significantly over the past few decades. Paul Tessier 5 described the subperiosteal dissection of the midface in the late 1970s, paving the way for others to explore their respective techniques for similar rejuvenation of the midface. Hamra 6 went on to describe the composite rhytidectomy, which added a midface component to the rejuvenation by elevating the orbicularis oculi with the SMAS flap and superomedially fixating the muscle to the orbital rim. In the mid1990s, Hamra further elaborated on periorbital fat preservation and arcus marginalis repositioning. 7 Ramirez then extended his endoscopic forehead lift to the midface, later suspending the SOOF, malar periosteum, and the buccal fat pad of Bichat. 8 Owsley and Zweifler 9 also described an extended rhytidectomy to address midface subperiosteally, and in 1998, McCord 10 et al discussed the transblepharoplasty subperiosteal midface lift for tear trough and melolabial fold correction. This entailed a subperiosteal dissection of the midface, release of the periosteum, and suspension of the midface to the periosteum of the lateral orbital rim. A canthoplasty or canthopexy was utilized to support the lower lid. Gunter 11 later performed a similar procedure, however, without the lower lid canthoplasty or canthopexy except in cases of significant eyelid laxity. Goldberg 12 followed by elaborating on lower blepharoplasty fat repositioning that may be used in conjunction with midface lifting.
Preoperative Assessment
When evaluating patients preoperatively, it is important to verify whether the patient is a good candidate for midface repositioning, or whether additional or alternative procedures may be indicated. A patient with weak malar projection may benefit from a malar implant, or excessively hollow cheeks may be improved with submalar implants. Soft tissue fillers may be used to temporarily address inadequacies of the cheek or midface; however, large volumes are usually required to achieve this transient effect. Fat transplantation is also a consideration for loss of volume. Patients in their 30s or 40s may be good candidates for melolabial plication or suture suspension if they are interested in less downtime. Of course, patients who undergo a subperiosteal midface lift must be counseled that swelling may persist for 3 to 6 weeks, and the eyes may appear to look Asian until the edema resolves. For patients who are interested in total midface rejuvenation, it is appropriate to rank the procedures in order of most to least effective for the patient’s anatomy and interests. This will allow patients to consider their options when deciding on multiple rejuvenative procedures, such as blepharoplasty, forehead lift, facelift, and resurfacing. As with all cosmetic procedures, a complete history and physical examination is necessary, along with a standard preoperative interview that explores patient motivations, psychological fitness, and emotional stability.
Surgical Techniques
The most commonly used surgical approaches to the midface include the transtemporal subperiosteal midface lift (TTML), the transblepharoplasty subperiosteal lift (TBML), and the transblepharoplasty SOOF lift. Less commonly, melolabial plication and direct excision of the nasolabial folds are options. Choice of procedure depends on a variety of factors, including preferred outcome, tolerance for downtime, training bias, and concomitant procedures. The TTML may be easier to perform with an endoscopic forehead lift as they share dissection planes and temporal incisions. Similarly, the transblepharoplasty approaches are more easily done with concomitant skin/muscle flap blepharoplasty. Table 27.1 briefly compares the merits of each approach.
Transtemporal Subperiosteal Midface Lift
The TTML is often performed in conjunction with an endoscopic forehead lift, and it can be achieved via an open or endoscopic approach. The subperiosteal layer is commonly utilized for the endoscopic forehead lift, and this plane is easily extended inferiorly to address midface ptosis. Please refer to Chapter 15 for details on the forehead/browlift procedure. The TTML is also frequently performed with a lower facelift, after all aspects of the lower lift have been completed, with the exception of skin redraping and closure.
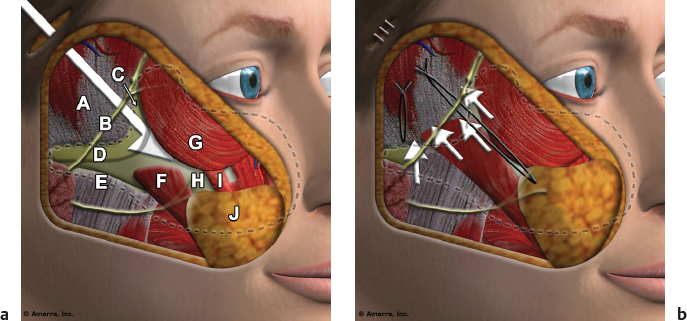
It is the authors’ preference to begin the TTML by performing the dissection over the maxilla and medial zygoma through a transconjunctival blepharoplasty approach. The rationale for this is the direct exposure to the subperiosteal plane of dissection, the complete release of the medial twothirds of the periosteum and arcus marginalis at the inferior orbital rim, the extent of the subperiosteal dissection medially to the pyriform aperture and the ease of identification and preservation of the infraorbital nerve. This allows for easy communication from the temporal approach to the medial midface after that dissection has been completed, and avoids the use of an endoscope. In addition, if fat pseudoherniation is present in the lower eyelid it can be addressed at that time. Other options for this dissection are endoscopically or under direct vision from the temporal dissection or transorally with direct visualization.
The transconjunctival incision is made with a needlepoint cautery on the cutting mode 2–3 mm below the tarsus and continued through the retractor muscle. The dissection proceeds in the preseptal plane down to the level of the orbital rim, and it is best accomplished with two cotton-tipped applicators, using a pushing motion with one and countertraction with the other. The periosteum is incised on the anterior aspect of the orbital rim and the subperiosteal dissection is completed under direct vision, extending medially to the pyriform aperture, inferiorly to below the level of the nasal ala and laterally almost to the zygomaticofacial nerve, preserving the infraorbital nerve. The arcus marginalis is released at the level of the orbital rim and fat pseudoherniation, if present, is addressed and attention is turned to the temporal dissection.
The temporal approach to the midface traverses deep to the superficial temporal fascia. This fascial layer is the superiormost extension of the SMAS layer, and it is continuous with the galea across the forehead. The superficial temporal fascia is the most superficial of the temporal fascial layers, and it contains the frontal branch of the facial nerve and the temporal artery and vein. The relationship of the neurovascular structures within the superficial temporal fascia is analogous to that of the facial nerve and mimetic musculature found within the SMAS inferiorly. Pitanguy’s line is used as a landmark for the frontal branch, delineating a line that runs from the lobule to the lateral canthus. As this line crosses the zygoma, at roughly the midpoint from the helical root to the lateral canthus, this approximates the location of the frontal branch of the facial nerve. 13 Dissection in the temporal region is on top of the fascia overlying the temporalis muscle and deep to the superficial temporal fascia, as this will protect the facial nerve. In this plane one encounters bridging veins lateral to the lateral orbital rim that run from superficial to deep, traversing the temporal fascial planes. This vein, also known as the sentinel vein, is an important landmark that heralds the proximity of the frontal branch of the facial nerve within 1 cm, and it should be preserved to avoid arborization of facial venous networks. When necessary, this vein is cauterized only along the deep aspect to avoid thermal injury to the overlying nerve. 14
The plane of dissection in the TTML is below the superficial temporal fascia and on top of the true fascia of the temporalis muscle. As the dissection reaches the orbital rim and the zygomatic arch, the true temporalis fascia splits into superficial and deep layers, separated by the intermediate fat pad. This is distinct from the deeper fat pad of Bichat, which overlies the temporalis muscle and is deep to the temporalis fascia just described. The fat pad of Bichat is significant as violation of this plane may lead to atrophy of the fat with resultant temporal wasting. At the level of the zygomatic arch, the superficial layer of the temporalis muscle fascia attaches to the superolateral surface of the zygomatic arch and the deeper layer attaches to the superomedial aspect of the zygomatic arch. Additional protection of the frontal branch of the facial nerve can be provided by incising the temporalis fascia ∼1 to 2 cm above the zygomatic arch and proceeding in the plane of the intermediate fat pad down to the zygomatic arch, and staying directly on the bone when dissecting over the arch. Gosain et al 15 confirmed with cadaveric studies that the frontal branch of the facial nerve ramifies as an average of three additional branches across the zygomatic arch, with all specimens possessing a distinct anterior and posterior trunk. These anatomical relationships confirm the need to remain beneath the superficial layer of the true temporalis fascia when exposing the zygomatic arch. This can be safely achieved by starting at the root of the zygoma and proceeding anteriorly in the subperiosteal plane to the body of the zygoma. 16
The temporal incision extends from the inferior aspect of the tragus, either in front of or along the margin of the tragus, superiorly into the temporal area about 5 cm, curving slightly anteriorly toward the hairline. If performed in conjunction with a lower facelift, all aspects of the lower lift are completed with the exception of skin trimming and closure. The temporal dissection proceeds down through the superficial temporal fascia to the level of the temporalis fascia, noted by its glistening white appearance. This plane is bluntly extended superomedially to the temporal line and inferomedially, beyond the conjoined tendon, to the subperiosteal layer at the frontal process of the zygoma. As mentioned previously, care is taken to avoid disruption of the sentinel vein, as this runs close to the frontal branch of the facial nerve and disruption of this vein can result in postoperative prominence of the cutaneous veins of the temporal region. Adequate release of the conjoined tendon is critical to avoid postoperative bunching after suspension of the midface. The arcus marginalis is also released, with care to preserve a 1-cm cuff of tissue around the lateral canthal periosteal attachment. Failure to preserve this periosteal cuff can lead to lateral canthal distortion.
The subperiosteal dissection proceeds inferiorly on the lateral body of the zygoma down to the level of the junction of the body with the zygomatic arch. An incision is made through the temporal fascia proximately 1–2 cm above and parallel to the zygomatic arch, exposing the intermediate fat pad. Attention then turns to dissecting the soft tissues in front of the helicofacial junction down to the level of the temporal fascia and exposing the root of the zygomatic arch. The periosteum is incised at the root of the zygomatic arch and dissection proceeds anteriorly along the arch in the subperiosteal plane, connecting with the intermediate fat pad just above the arch, thereby protecting the frontal branch of the facial nerve. Anteriorly this connects with the previous subperiosteal dissection at the orbital rim and lateral zygoma. Periosteal elevation continues over the body of the zygoma to connect with the subperiosteal dissection previously performed through the transconjunctival blepharoplasty approach. The zygomaticofacial nerve exits the zygoma below the lateral aspect of the infraorbital rim, and this should be preserved (although disruption of this nerve does not result in longterm sensory deficits).
For maximum midface mobility, the dissection proceeds inferiorly a few centimeters over the origins of the masseter muscle, starting with release of the soft tissues over the temporomandibular joint and proceeding anteriorly along the zygomatic arch. This dissection over the origins of the masseter muscle continues below the body of the zygoma as well. It has been found that when the subperiosteal elevation is carried inferiorly over the origins of the masseter muscle along the entire extent of the zygoma, the direction of pull can be almost vertical.
Once the midface is adequately mobilized, it is first suspended either by suturing the malar fat pad, the periosteum, or both to the temporalis fascia in a predominantly superior vector. 13 , 17 Suspension has also been achieved utilizing the Endotine (Coapt Systems, Inc.) device. The Endotine device is an absorbable device that has a long, flat strap with a head full of short suspension tines at one end. The malar repositioning is achieved by embedding the tines underneath the periosteum and soft tissues of the cheek adjacent to the melolabial fold. The other end of the strap is suture fixated to the superficial layer of the temporalis fascia giving the desired lift. This suspension method has been occasionally used by the authors in patients with very deep melolabial folds or very ptotic malar fat pads. Saltz 18 has reported excellent experience with this device.
As mentioned, if the dissection has proceeded over the entire extent of the zygomatic arch and over the origins of the masseter for a few centimeters, the pull can be more vertical. A second suture is placed through the SMAS and associated connective tissue at the level of the superior tragus and advanced directly superior 1–2 cm and secured to the temporal fascia ( Fig. 27.6 ). This not only helps to further elevate the midface but also increases elevation of the lower face, as is shown in the accompanying video. Skin incisions are closed in the preauricular area with sutures and the temporal portion of the incision with staples. When this procedure is combined with an endoscopic forehead lift, the dissection is in a continuous plane from the forehead to the midface. If a simultaneous lower facelift has been performed, the skin is redraped, trimmed, and the incisions closed in the usual fashion ( Video 27.1).
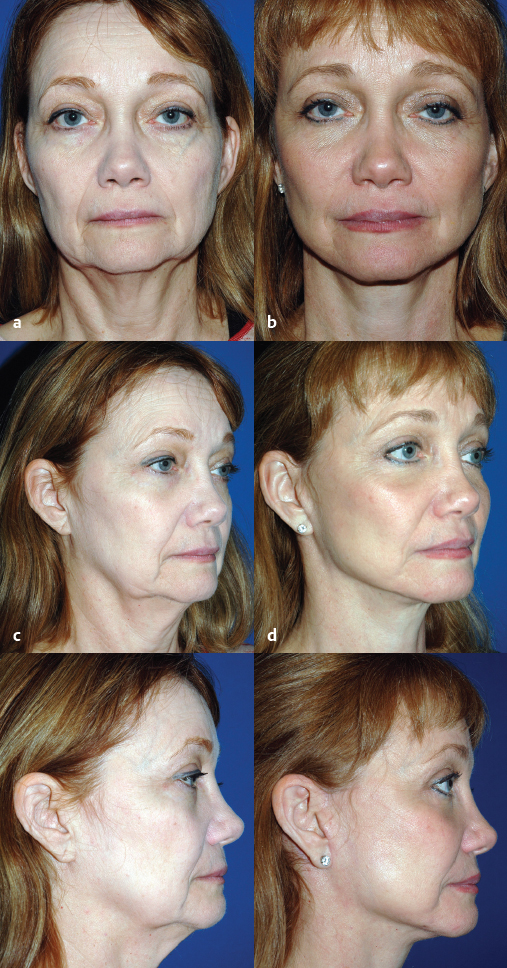
Advantages of the TTML include the ease of concomitant forehead lift and avoidance of skin/muscle flap blepharoplasty incisions that may result in eyelid malposition. The predominantly superior vector is reasonably effective in suspending the aging midface structures ( Figs. 27.7–27.9 ). Ransom 19 reported improvement in the eyelid/cheek contour with concomitant transconjunctival lower blepharoplasty and TTML. Disadvantages are risk of injury to the frontal branch of the facial nerve, lateral canthal distortion resulting in an Asian appearance, widening of the intermalar distance with repositioning of the origins of the zygomaticus major and minor muscles to a more superior position, and significant postoperative edema that necessitates a longer recovery time. Facial nerve injury is usually avoided when in the appropriate plane of dissection over the zygomatic arch, and most neuropraxias are temporary. Lateral canthal distortions also resolve with time and are best prevented with limited release of the arcus marginalis and periosteum in the immediate vicinity of the lateral canthus. Elevation and repositioning of the origins of the zygomatic major and minor muscles adds fullness to the area lateral to the orbits and can increase the appearance of the intermalar distance but this usually resolves over time.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








