20 Ablative Laser Facial Skin Rejuvenation
Introduction
Current technology and techniques for facial skin rejuvenation have expanded significantly since the publication of Carniol’s Laser Skin Rejuvenation. 1 Laser resurfacing is only a portion of the armamentarium of most facial plastic surgeons. In addition to ablative resurfacing lasers, there are now fractional lasers, nonablative lasers, and light devices that can be used to diminish epidermal lesions, stimulate neocollagen production, and tighten skin. Furthermore, as technology and techniques have improved, we have been able to offer our patients a broader range of improvement, select the optimal available technology, and set higher standards for our results. Besides addressing texture, rhytids, and laxity, we also can address scars, telangiectasias, vascular lesions, dyschromias, and lentigines. By addressing all of these issues we can optimize our patients’ results. Acne and acne scars can also be treated with ablative lasers, 2 nonablative lasers, 3 and fractional lasers.
Ablative resurfacing lasers require a longer recovery and have a higher side effect profile than fractionally ablative resurfacing or nonablative lasers. However, it should also be noted that they usually produce a more dramatic result. Ablative resurfacing can be performed with the carbon dioxide (CO2) or erbium:yttriumaluminum-garnet (Er:YAG) lasers. Ablative laser resurfacing is most commonly used for photoaging, rhytids, laxity, and scarring. While rhytids and dyschromias are highly responsive to ablative resurfacing, scars may be less responsive.
The depth of resurfacing can be varied depending on the desired result. Recently, superficial erbium laser resurfacing has become popular to reduce epidermal lesions, dyschromias, and rhytids. Nonablative lightbased devices include the 1064 nm Nd:YAG, 1320 nm Nd:YAG, 1540 nm Er:glass, pulsed dye, and 532 nm lasers, and also Intense Pulsed Light (IPL) and the 1450 nm diode. 4
Laser Biophysics
The word laser began as an acronym for light amplication by stimulation emission of radiation. The coherent light emitted is at a single wavelength. This contrasts with IPL devices that produce a spectrum of light wavelengths. 5 The property of selective photothermolysis allows the surgeon to select a laser wavelength that is maximally absorbed by the targeted tissue component, the tissue chromophore. In the skin, there are three main chromophores: water, hemoglobin, and melanin. The primary chromophore for the CO2 lasers and Er:YAG lasers is water. Whenever using a laser, consideration should be given to other competitive chromophores that may absorb the wavelength. These competing chromophores may give additional benefit or create additional risks associated with using a particular laser wavelength.
For example, at a wavelength of 532 nm, there is absorption of laser energy by both oxyhemoglobin and melanin. Thus, this type of laser can affect both vascular and pigmented lesions. Therefore, in patients with higher Fitzpatrick skin types there is an increased risk of developing hypopigmentation if treated with this laser wavelength.
The possibility of competing chromophores should be considered whenever a laser is being selected. This should also be considered whenever using an IPL device, which can produce a spectrum of wavelengths. The spectrum of emitted wavelengths will depend on the light source as well as any associated filters.
Examples in which competing chromophores can be advantageous are the current hair reduction lasers, which are designed to exert their effect on melanin, the target chromophore. These lasers may also be absorbed by hemoglobin, which is a competing chromophore. This absorption by hemoglobin, the competing chromophore, can also result in injury to the blood vessels supplying the hair follicle, which is desirable.
Ninety percent of the epidermis is water. Consequently, water is the primary chromophore for the current resurfacing lasers, including the Er:YAG and CO2. During resurfacing treatments, the intercellular water absorbs laser energy and instantly boils or vaporizes. The amount of energy that a laser delivers to the tissue and the time over which it is delivered determines the amount of tissue vaporized. For skin resurfacing, the objective is to vaporize the primary chromophore, water, while transferring a limited amount of heat to the surrounding collagen and other structures. This is because type I collagen is extremely heat-sensitive and becomes denatured at 60°C to 70°C. These lasers are designed to avoid excessive thermal injury to the collagen as this can produce scarring.
The fluence of a laser represents the amount of energy (joules) that is applied to the surface area of tissue (centimeter squared). Therefore, fluence is expressed as J/cm2. For CO2 lasers, 0.04 J/mm2 is the critical energy needed to overcome the tissue ablation threshold. For skin resurfacing, this is can be accomplished with 250 mJ per laser pulse using a 3-mm spot size. After each pulse, the tissue is allowed to cool before the delivery of the next pulse. The tissue thermal relaxation time is the amount of time necessary between pulses for complete cooling to occur. The pulse duration is the time the tissue is actually lasered. One way to minimize nonselective thermal injury is to keep the pulse duration equal to or less than the thermal relaxation time. Spot size is the diameter of the laser beam. For a given wavelength and fluence, smaller spot sizes have less depth of penetration due to increased effects of scatter. Depth of penetration also varies with wavelength, fluence, and laser pulse duration. If all other parameters are held constant, the longer the wavelength the greater the depth of penetration. 5
With laser resurfacing, a very high fluence is selected to vaporize target tissue almost instantly. This high fluence allows very short pulse durations (1 millisecond) to be used. Consequently, unwanted heat conduction to adjacent tissue is minimized. Power density, usually measured in watts, takes fluence, pulse duration, and treatment area into account (i.e., 60 W). A common misconception is that lower fluences or lower power densities will reduce the risk of scarring, when in reality if the energy is too low it boils intracellular water more slowly rather than vaporizing it and causes greater nonspecific thermal injury.
The water absorption coefficient is higher for the erbium laser. It ablates tissue with less adjacent thermal injury. Therefore, healing is faster than after resurfacing using a CO2 laser. This makes superficial resurfacing with an erbium laser more acceptable to patients as there is a significantly shorter recovery time for an equal depth of resurfacing with the CO2 laser. However, if it is used to produce less adjacent thermal injury there is also less neocollagen production. This relates to production of heat shock proteins. One manufacturer has an erbium laser with a slightly increased pulse duration to increase the adjacent thermal injury and increase neocollagen production.
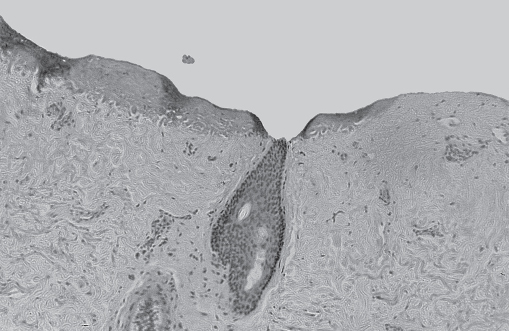
Histologic studies of biopsies taken immediately after laser resurfacing demonstrate a zone of tissue vaporization and ablation beneath which lies a basophilic zone of thermal necrosis ( Fig. 20.1 ).

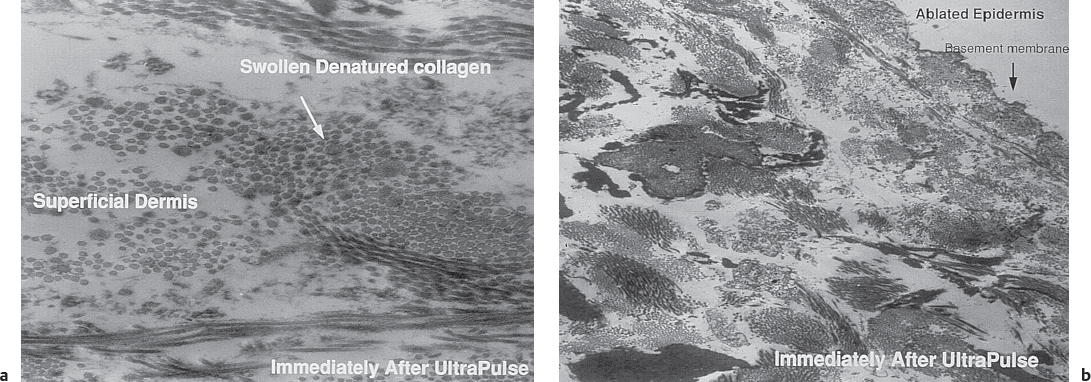
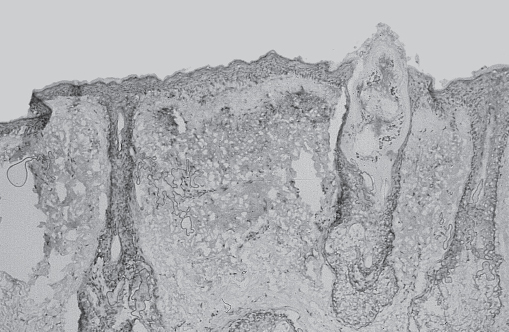
The energy of the initial laser pass is absorbed by the water within the epidermis. Once the dermis has been entered, there is less water to absorb laser energy, and heat transfer contributes to more thermal injury with each successive pass ( Fig. 20.2 ). So ideally, for the CO2 laser, a greater depth of ablation with a smaller number of passes and less thermal injury offers the least risk of scarring. Ultrastructural studies demonstrate smaller collagen fibers within larger collagen bundles in the papillary dermis ( Fig. 20.3 ). After laser resurfacing, wound-healing molecules, such as the glycoprotein tenascin, are expressed as new collagen that is produced in the papillary dermis ( Fig. 20.4 ).
Laser Safety
The importance of proper laser safety cannot be overemphasized. Laser safety includes, but should not be limited to, the current American National Standards Institute standards. It is important that each laser surgeon understands the principles of laser safety.
When using general anesthesia, there is a greater risk of laser fire associated with the use of oxygen and an endotracheal tube. There are now metal endotracheal tubes, foil wrappings for plastic endotracheal tubes, and endotracheal tubes that are designed specifically to be used with lasers. This is important to prevent endotracheal tube ignition and a possible airway fire.
Protective Eyewear
The first safety issue with any laser is avoidance of eye injury. Injury can occur with visible and invisible laser wavelengths. The eyes of the patient, laser room staff, and surgeon must be protected from inadvertent injury with appropriate eye protection. The protective eyewear must be designed for the particular laser wavelength. The optical density and wavelength for which the eyewear is protective should be printed on the eyewear frame. In general, laser protective glasses or goggles should have an optical density (ocular density) of at least 5. The optical density scale is exponential. Thus, an optical density of 5 means that for the specified wavelength noted on the side of the glasses or goggles, only one 10,000th of the laser energy will get through the lenses.
Skin Preparation
It is imperative that all makeup and moisturizers be removed before treatment is initiated. Alcohol-based skin preparations should be avoided, as these can create a fire hazard. It is safer to use aqueous-based solutions. Proper precautions must be taken for all skin cleansers.
Smoke Evacuator
For devices that produce a significant plume, smoke evacuators with specifically designed laser filters to trap laser plume contents should be used.
Laser Masks
When performing a resurfacing procedure which produces a significant plume, each person in the operating room should use a laser mask, which effectively filters infectious particles in the laser plume. These masks have a 0.1-mm filter pore size.
Skin Type Classification
It is important to consider skin type classification whenever considering laser or IPL therapy. The classification system is based on the response to ultraviolet light. In general, it also varies directly with the amount of melanin in the skin.
After laser resurfacing, possible problems with dyschromia depend on several factors, which include the Fitzpatrick skin type classification, depth of resurfacing, type of laser used for resurfacing which affects the amount of adjacent thermal injury, and any possible healing problems.
The Fitzpatrick skin classification system can be described as follows:
Class I: Very fair skinned, always burns, never tans
Class II: Fair skin, burns, possible mild tan
Class III: Medium skin tone, sometimes burns, tans
Class IV: Darker medium skin tone, rarely burns, tans readily
Class V: Darker skin tone, rarely burns, intensely tans
Class VI: Darker skin tone, never burns, intensely tans
Due to potential problems with dyschromia, with current technology the first author (P.J.C.) does not routinely perform CO2 laser resurfacing on patients with skin types IV, V, and VI.
Ablative Resurfacing Lasers
Carbon Dioxide Laser Resurfacing
The CO2 laser was invented in 1964 by Patel. 6 In the mid-1980s, CO2 lasers were used by some physicians for the removal of exophytic skin lesions and limited cutaneous skin resurfacing. The usefulness of the continuouswave CO2 laser (10,600 nm) was limited by its long pulse duration, which had the potential to produce unwanted adjacent thermal damage and scarring. 7 , 8 , 9 , 10 As laser technology improved, higher energy laser systems were developed that offered much shorter pulse durations more suitable for resurfacing. One of the first reported resurfacing treatments with a pulsed CO2 laser was performed by Larry David. 11 In 1993, Fitzpatrick reported use of the Ultrapulse CO2 (Coherent Medical Products), which produced relatively high fluence and much shorter pulse duration (1 millisecond) than earlier pulsed or superpulsed CO2 lasers. This combination provided relatively clean vaporization with a limited zone of adjacent thermal injury. This was the first CO2 laser that could be predictably used for the removal of superficial skin tumors and for cutaneous resurfacing. 12
Initially, in describing CO2 laser resurfacing, it was recommended that resurfacing be performed until a “chamois” appearance of the tissues was achieved. In 1995, Carniol recommended the first modification of this technique to decrease postresurfacing complications and facilitate healing. 13 Other pulsed and scanned lasers, such as Silktouch and Feathertouch (Sharplan Lasers) and Paragon (Lasersonics), were also developed for facial resurfacing. Most of these lasers utilize a 900- to 1,000-µs pulse duration or a rapid scan that created a relatively similar fluence and energy exposure duration. Many laser systems employ a computerized scanner which allows larger surface areas to be treated in a very systematic predictable fashion. 14
Light energy from the CO2 laser is absorbed by intracellular and extracellular water, resulting in coagulative necrosis and skin vaporization. As the epidermis is ablated and dermal temperatures exceed 55 to 62°C, collagen denaturation occurs. 15 This is followed by neocollagenesis and skin reepithelization, with subsequent skin tightening seen with the CO2 laser. A single pulse of the CO2 laser with a fluence of 5 to 19 J/cm2 and a pulse duration less than 1 ms can ablate 20 to 40 µm of tissue. 16 A single pass at these fluence settings can cause epidermal ablation. Ablation plateaus after the third laser pass when the depth has reached 200 µm, with additional passes causing thermal injury and scarring. 17 While the boiling point of water at 1 atmosphere is 100°C, ablation at these parameters can heat tissue to 120 to 200°C. 18
The skin tightening seen clinically with ablative CO2 lasers has been correlated histologically. Thirty-three patients were treated with either the pulsed CO2 laser or the continuouswave CO2 laser in the forehead, glabella, periorbital, or perioral regions. 19 Biopsy specimens of seven patients taken 1 year posttreatment noted subepidermal neocollagenesis measuring 100 to 350 µm in depth.
Patient Selection
Ablative laser resurfacing is indicated for rhytids, dyschromias, scars, and photoaging. An ideal candidate for ablative skin resurfacing is a Fitzpatrick skin type I to IV and has reasonable expectations for outcome ( Fig. 20.5 ). Great results have been achieved on periorbital/perioral fine rhytides, which are areas less amenable to surgical improvement. Ablative lasers are ideal for fine to moderate rhytides and static wrinkles, and less predictable for deep dynamic rhytides. Relative contraindications to ablative resurfacing include pregnancy, dermatologic conditions, history of radiation, keloid formers, Fitzpatrick V and VI, and recent isotretinoin usage. Patients with adnexal disease (such as scleroderma) will have poor healing since reepithelialization relies on stem cells in skin appendages.

Preoperative Patient Care
Patients who undergo deep resurfacing require intensive management. There is still controversy over whether skin preparation is needed for resurfacing. Some surgeons advocate pretreatment with hydroquinone, tretinoin, or glycolic acids. 20 , 21 , 22 Other physicians do not use any formal preparation before the procedure. Most surgeons agree that avoidance of sun before resurfacing is important. Exposure to the sun before resurfacing can activate the melanocytes and predispose the patient to hyperpigmentation. Isotretinoin use is typically avoided 12 months prior to ablative resurfacing. The importance of prophylactic antivirals for patients with a history of orofacial herpes undergoing deep resurfacing has been well documented. 23 Treatment is initiated 2 days prior to resurfacing for those with a history of herpetic outbreak and 1 day prior for all other patients. This antiviral therapy should be continued for 10 to 14 days until all reepithelialization is complete. Each physician has to make his or her own management decisions, but in general the authors treat all of their patients with prophylactic antiviral therapy.
The use of prophylactic antibiotics is much less universal. Many surgeons give antibiotics before and after the procedure to diminish the incidence of bacterial infection with prolonged or closed-mask dressings. Some physicians believe that prophylactic antibiotics do not diminish the chance of postresurfacing infection. 24 Physicians who use prophylactic antibiotics frequently give prophylactic antifungal medication to prevent yeast infections underneath the dressings.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








