2 Extensor Tendon Repair (Zones 2, 4, 6-9)
Abstract
This chapter focuses on extensor tendon injuries from zone 2 to 9 excluding zones 1, 3, and 5. Surgical repair is favored for complete injuries or partial ones which involve more than 50% of the width of the tendon. Various techniques have been described to lessen the chance of tendon shortening and gap formation and to improve the ease of the technique. Traditionally, the modified Becker technique is superior over the modified Kessler, figure of 8, or modified Bunnell suture technique. The RITM (running, interlocking, horizontal mattress) technique provides greater strength, less shortening, and faster operative time compared to the modified Becker stitch, especially for zone 2 to 4 repairs. Rehabilitation for zone 4 to 7 repairs can consist of the Wyndell Merritt protocol that allows for early active motion. Complications such as tendon adhesion, rupture, and limited flexion can be mitigated by optimal repair technique and appropriate rehabilitation.
2.1 Introduction
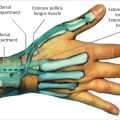
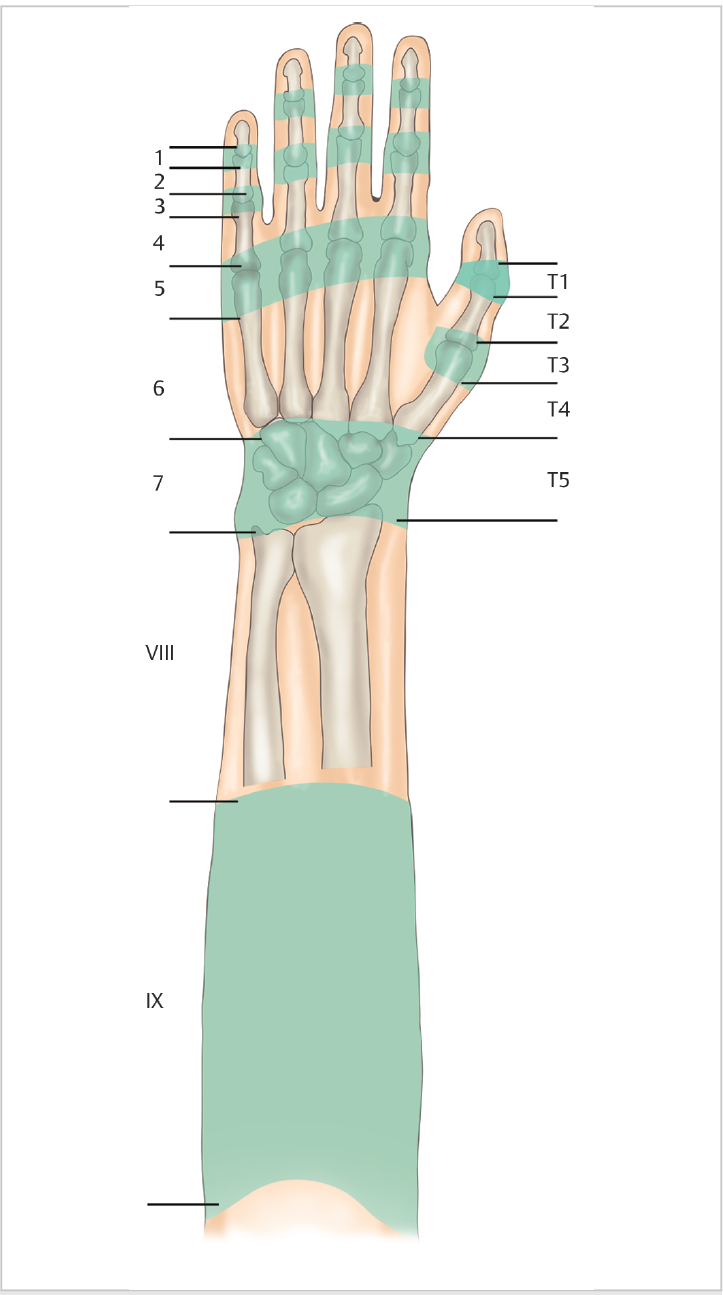
Extensor tendon injuries can be divided in to nine zones (► Fig. 2.1). Zone 1 includes the distal interphalangeal (DIP) joint, zone 2 the middle phalanx, zone 3 the proximal interphalangeal (PIP) joint, zone 4 the proximal phalanx, zone 5 the metacarpophalangeal (MCP) joint, zone 6 the metacarpals, zone 7 the carpus, zone 8 the musculotendinous junction, and zone 9 the muscles of the extensors. Thumb zone 1 is over the interphalangeal joint, zone 2 the proximal phalanx, zone 3 the MCP joint, zone 4 the thumb metacarpal, and zone 5 the thumb carpometacarpal (CMC) joint. This chapter will discuss initial evaluation, treatment, rehabilitation, and complications related to extensor tendon injuries in zones 2, 4, 6, 7, 8, and 9. Zones 1, 3, and 5 are described in Chapter 1.
2.2 Evaluation
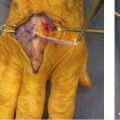
Examination starts with observing the normal cascade of the hand. The examiner needs to test each finger individually for extension lag or weakness to prevent the juncturae tendinum from masking a tendon injury. Associated bony and soft tissue injuries need to be addressed at the same time or in a staged fashion.
2.3 Treatment
2.3.1 General Treatment Guidelines
When examining a patient with an extensor tendon laceration, it is important to assess active and passive motion of the finger and wrist. Radiographs should be obtained to rule out bony injuries or radiopaque foreign bodies. Neurovascular status should be documented. With open fractures, appropriate washout, debridement, and antibiotics should be administered, and tetanus should be updated. It is also important to test each extensor compartment for zone 7 injuries. In grossly contaminated wounds, repair is delayed until the contamination is under control. Despite better repair techniques and rehabilitation, patients should be advised that some extensor lag may persist, and full flexion may not be possible despite successful treatment.
2.3.2 Repair Techniques
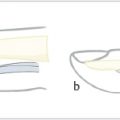
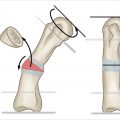
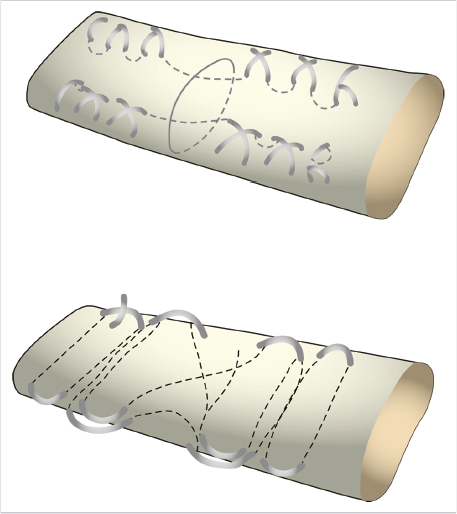
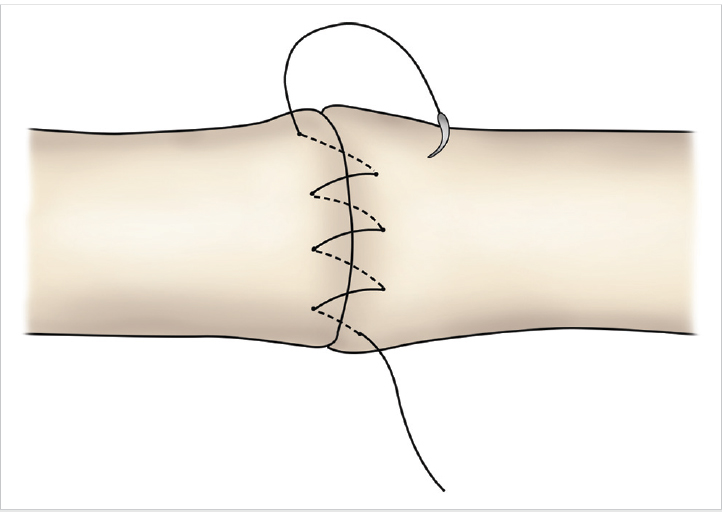
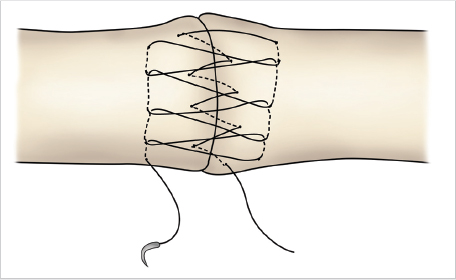
Repair techniques include modified Becker, modified Bunnell (► Fig. 2.2), modified Kessler, or running, interlocking, horizontal mattress (RITM) stitch as described by Lee et al 1 (► Fig. 2.3 and ► Fig. 2.4). The augmented or modified Becker suture method was performed with two rows of laterally placed crisscrossing sutures initiated 1 cm from the edge of the tendon with three crosses for each side of the tendon margin. The modified Bunnell suture method consists of four core sutures with the second core suture placed next to the first as described by Howard et al. 2 For the RITM suture configuration, a simple running suture is placed followed by a mattress configuration that is locked by passing the suture needle underneath the preceding crossing suture. Woo et al 3 reported four different extension repair techniques comparing modified Kessler, modified Becker, figure of 8, and double loop technique. They found that the modified Becker technique failed solely by suture breakage instead of pull out, with the highest resistance to gapping. They suggested that sutures applied to the lateral edge of the extensor tendon perpendicular to the orientation of the fibers provided the strongest repair, especially for zone 2 and 4 injuries. In addition, with the modified Becker technique the crisscross lattice creates a finger trap effect around the tendon to strengthen the repair. 3 Chung et al 4 performed a biomechanical study investigating the strength of 1, 2, or 3 cross-stitches using the modified Becker technique and found that a single cross-stitch had increased stiffness, yield load, and less gap formation than multiple cross-stitches. However, a single cross-stitch had a lower ultimate load to failure compared with three cross stitches. The tendon distal to the MCP joint (zones 2–4) are generally thinner and best repaired with RITM technique using 4–0 nonabsorbable braided sutures, whereas the tendon proximal to zone 5 can accommodate a core suture better and can be better secured with a modified Kessler or modified Becker stitch using 3–0 nonabsorbable braided sutures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree