Serial injections are started 7–10 days post insertion provided the skin flaps are in excellent condition and continue on a weekly basis for about 10–12 weeks. Most pediatric patients go on a home expansion protocol with injections performed by the parents under the direction of our nursing staff and surgeons. If another set of expanders is needed to fully excise the lesion (serial expansion) we usually wait 4–6 months.
A broad-spectrum antibiotic is started upon surgery and is continued until the drains are removed. By maintaining a low threshold for placing the patient back on antibiotic in the presence of suspected incipient infection, most infections can be controlled before loss of the expander.
The design of an expanded flap is of major importance. While the early dogma of tissue expansion emphasized designing advancement flaps only, experience over more than two decades has demonstrated that expanded transposition and rotation flaps may frequently be preferable. It provides greater versatility in flap design and range [1,2].
References
1 Bauer BS, Margulis A. The expanded transposition flap: shifting paradigms based on experience gained from two decades of pediatric tissue expansion. Plast Reconstr Surg 2004;114:98–106.
2 Joss GS, Zoltie N, Chapman P. Tissue expansion technique and the transposition flap. Br J Plast Surg 1990;43:328–33.
Regional Consideration in Paediatric Tissue Expansion
The optimal choice of treatment still varies by body region and we discuss the most pertinent issues and considerations necessary for successful tissue expansion in each body region.
Scalp
The expander is placed in a pocket dissected subgaleal but staying above the periosteum. Flaps are designed with consideration of the major blood supplies to the scalp (superficial temporal, postauricular, occipital vessels and contribution from supraorbital vessels). Port placement in the preauricular area has produced the least migration. The expanders used in scalp reconstruction are usually of 250 or 500 mL volume. Giant naevi might require serial expansion with a larger expander placed after each stage to distribute expansile forces evenly over the hair follicles. As previous studies have shown, tissue expansion itself does not induce proliferation of hair follicles but can more than double the size of the scalp without visible decrease in hair density [1]. Despite former thoughts that expansion may affect cranial vault morphology, it usually self-corrects within 3–4 months [2,3].
The use of expanded transposition flaps versus simple advancement flap design has greatly reduced the number of serial expansion required and has resulted in improved reconstruction of hair direction and hairline (Fig. 191.2).
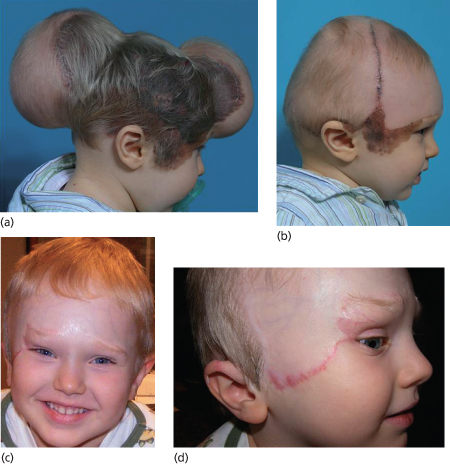
Fig. 191.2 (a) Giant congenital naevus covering the right scalp, upper ear, forehead and cheek. Expanded flaps are used to reconstruct the forehead and scalp. The surgeon must not overextend the flap but rather repeat expansion if needed. (b) Three months after one set of expansion. Increasing use of transposition flaps allows for better reconstruction of temporal hairline. (c,d) Final result 8 months after additional serial excision of the naevus in the right temple and cheek. The upper ear was reconstructed with postauricular flap and full thickness skin grafting of the upper periauricular surface was performed to avoid hair growth in this non-hair-bearing area. The patient may need some minor scar revision in the future.
Face and Neck
Large and giant naevi of the face are the most visible of these lesions and also represent the area where unsightly scarring is most readily visible; consequently, the planning and execution of the reconstructive plan must be very detailed. A description of all the nuances of treatment of facial naevi is beyond the scope of this chapter. What follows is the summary of the highlights.
To achieve an optimal aesthetic and functional result in the facial and cervical regions, one must adhere to the subunit principle. This dictates incision placement so the final result has the scar hidden in a natural crease (e.g. nasolabial fold). Undue tension on facial structures (brow, eyelid, mouth) can cause disfigurement such as brow asymmetry or ptosis, anterior hairline asymmetry, lower lid and oral drooping, especially when using cervical skin flaps cephalad to the cervicomandibular angle.
Neale et al. [4] report 10% lower eyelid ectropion rate and >10% lower lip deformity in this context. Judicious flap design and the use of expanded transposition and rotation flaps, use of multiple expanders and overexpansion are recommended to further minimize these complications (Fig. 191.3).









