References
1 Einstein A. Letter to Michele Angelo Besso, November 1916.
2 Einstein A. Zur Quantentheorie der Strahlung (On the Quantum Theory of Radiation). Physica Zeitschrift 1917;18:121–8.
3 Anderson RR, Parrish JA. Microvasculature can be selectively damaged using dye lasers: a basic theory and experimental evidence in human skin. Lasers Surg Med 1981;1:263–76.
4 Lou WW, Geronemus RG. Treatment of port wine stains by variable pulse width pulsed dye laser with cryogen spray: brief communication. Dermatol Surg 2001;27:963–5.
Mechanism of Action of Vascular Lasers
Optical penetration into the skin is governed by a combination of absorption and scattering of light. A wavelength of 577 nm was initially employed for the process of selective photothermolysis [1] for preferential absorption by oxyhaemoglobin of red blood cells within the dilated superficial blood vessels. This produces selective thermal damage to the target blood vessels. Within biological systems each component, for example, a macromolecule such as haemoglobin will have its own specific absorption spectrum. If a wavelength is selected that corresponds to the absorption peak of one component but not to a peak for any of the others, that component can be specifically targeted. If the light is of high intensity then this enables a large quantity of energy to be deposited within that biological target. Provided that certain other parameters are satisfied, this creates the ability to selectively damage one tissue component while leaving the others relatively intact.
Thus, it is the wavelength of laser light that determines its penetration into tissue and the chromophore (e.g. haemoglobin) in the superficial capillaries of the skin. With the new modified PDLs the wavelength has been extended from 577 nm to a range of 585–600 nm [2,3], which has the advantage of deeper dermal penetration without significant loss of absorption for the treatment of vascular lesions. Pulse duration of 0.45 ms was included in the design of the original PDLs on the basis of a calculated thermal relaxation time. Any vessel diameter between 10 and 50 µm would require less than 1 ms of thermal relaxation time (TRT). The laser spot size is also relevant; the newer lasers have a larger spot size (7, 10 and 12 mm; 12 mm used for the Perfecta V beam laser) which enables treatment to cover a larger area more speedily [4–6].
Mathematical models disregard certain thermal and optical considerations pertaining to live human skin, and a subsequent in vivo study has measured the TRT as 1–10 ms for vessel diameters of 30–150 µm. This is therefore longer than the pulse duration of the short (0.45 ms) PDL and the newer lasers have pulse durations of up to 40 ms.
Selective photothermolysis is an important concept to understand as it uses the principle of coagulation by the appropriate selection of wavelength, pulse duration and laser fluency. A precise biological target can be selectively and thermally damaged by lasers within the vasculature while sparing the surrounding tissue. The pulse duration selected is matched to the thermal relaxation time of the target.
References
1 Anderson RR, Parish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed irradiation. Science 1983;220:524–7.
2 Tan OT, Morelli JG, Garden J et al. Tunable dye laser (577 nm) treatment of port wine stains. Lasers Surg Med 1986;6:94–9.
3 Tan OT, Sherwood K, Gilchrest BA. Treatment of children with port wine stains using the flashlamp pumped tunable dye laser. N Engl J Med 1989;320:416–21.
4 Tan OT, Motemedi M, Welch AJ et al. Spotsize effects in guinea pig skin following pulsed irradiation. J Invest Dermatol 1988;90:877–88.
5 Tan OT. Dye laser for benign cutaneous vascular lesions: clinical and technical development. Lasers Dermatol 1991:60–72.
6 Laube S, Taibjee S, Lanigan SW. Treatment of resistant port wine stains with the V Beam pulsed dye laser. Lasers Surg Med 2003;33:282–7.
Vascular Pulsed-Dye Lasers
These contain a rhodamine dye that is excited by a xenon flash lamp and produces a light at 585–600 nm in pulses of 0.45 ms (short-pulse PDL), 1.5 ms (long-pulse PDL) and 1.5–40 ms (very long PDL). Light penetrates the dermis to a maximum depth of 1.2–1.5 mm. The higher wavelength and longer exposure time enables deeper penetration. In order to prevent any risk of damage to the surrounding skin caused by the increase in thermal exposure time and increase in the dissipation of heat, cooling devices have been introduced. Some lasers have an attachment to provide a targeted cryogenic spray to freeze the uppermost part of the skin a fraction of a second before the laser beam is delivered. Other cooling devices blow cool air across the treatment site during and after laser. Some systems apply a cooling gel before laser treatment is delivered, for example, Laser Aid gel (Geistlich Pharma, Wolhusen, Switzerland).
Most children under the age of 5 years require general anaesthesia, especially for large lesions on the face. Older children are usually able to tolerate treatment using local anaesthesia (Fig. 188.2), either EMLA® (eutectic mixture of local anaesthetics, which is 2.5% lidocaine and 2.5% prilocaine in an oil-in-water emulsion) [1,2] or preferably Ametop® (3% amethocaine gel). EMLA causes vasoconstriction, whereas Ametop causes vasodilation and is therefore preferred for the treatment of vascular lesions, especially port wine stains. Local anaesthesia, including nerve blocks, is used on occasions in older children and lidocaine gel 2% can be used in very small babies for immediate anaesthesia when treating small lesions such as papules, pyogenic granulomas or ulcerated haemangiomas.
Fig. 188.2 Laser treatment under local anaesthesia for a port wine stain: administered by Dr Samira Syed, aided by Nurse Specialist Jane Linward, using the Candela SPTL-1b machine.

PDLs are a relatively safe and effective treatment for vascular anomalies of the skin. Adverse effects are minimal: post-inflammatory hyperpigmentation and/or hypopigmentation; immediate post-laser purpura, which subsides within 5–10 days; blistering and crusting occasionally and, rarely, scarring. It is important to be aware of secondary postoperative infection, which in our experience is rare, in particular Staphylococcus aureus or herpes simplex virus type 1.
Laser treatment for all vascular birthmarks is best performed at an early age so that most, if not all, of the treatment is completed before the child starts school. This may not always be possible, but there is a clear advantage in terms of minimizing the potential psychological problems and also younger children tend to be more compliant with the procedure.
The Newer Generation of Vascular Lasers
Table 188.1 details the parameters or the vascular lasers used by our department at Great Ormond Street Hospital, London, UK.
Table 188.1 Laser parameters for vascular lesions
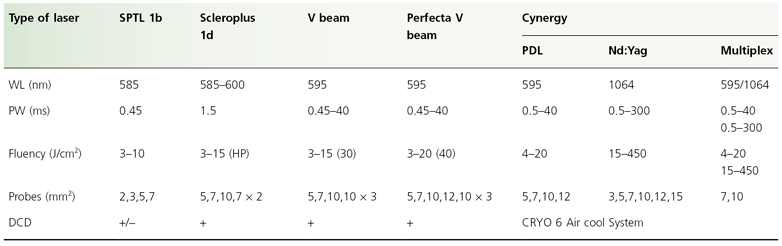
WL, wave length; PW, pulse width; DCD, dynamic cooling device; HP, high power.
V Beam Perfecta® (Candela Corporation, Wayland, MA, USA)
This PDL has a variety of different-sized probes and a higher fluency delivery.
Cynergy Multiplex Laser System® (Cynosure, Inc., Westford, MA, USA)
The Cynergy Multiplex laser system delivers the separate or sequential delivery of 595 and 1064 nm wavelengths at precisely timed intervals from the same delivery system for the treatment of vascular anomalies. It is useful for the treatment of refractory port wine stains, angiomas, venous malformations, difficult large thread veins, cutaneous small lymphatic lesions and other indications. Advantages are better clearance, fewer treatments, 2–3 days of bruising and minimal pain and discomfort. The mechanism, confirmed by several studies, demonstrates sub-therapeutic (PDL) light doses alter the absorption characteristics of blood, making it a better target for the 1064 nm Nd:Yag component [3–6]. PDL conversion of blood to a combination of methaemoglobin and thrombus temporarily increases the absorbance at 1064 nm by approximately 3–5 times that of normal blood [7,8]. This synergistic approach provides an enhanced effect on the vascular lesions. These higher powered lasers carry an increased risk of scarring and should be used with caution.
References
1 Sherwood KA. The use of topical anaesthesia in removal of port wine stain in children. J Pediatr 1993:122:536–41.
2 Tan OT, Stafford TJ. EMLA for laser treatment of port wine stain in children. Lasers Surg Med 1992;12:543–8.
3 Boixeda P et al. Advances in treatment of cutaneous and subcutaneous vascular anomalies by pulsed dual wavelengths 595 and 1094 nm. Medical Laser Application 2008;23(3):121–6.
4 Black JF, Barton JK. Time–domain optical and thermal analysis of blood undergoing laser photocoagulation. Proc SPIE 2001;4257:341–54.
5 Mordon S, Brisot D, Fournier N. Using a ‘non-uniform pulse sequence’ can improve selective coagulation with a Nd:YAG laser (1.06 µm) thanks to Met-hemoglobin absorption: a clinical study on blue leg veins. Lasers Surg Med 2003;32:160–70.
6 Tanghetti E. Controversies and Conversations in Cutaneous Laser and Cosmetic Surgery. Colorado Springs, CO, 2005.
7 Kuenstner JT, Norris KH. Spectrophotometry of human hemoglobin in the near infrared region from 1000 to 2500 nm. J Near Infrared Spectrosc 1994;2:59–65.
8 Heger M, Beek JF, Moldovan NI et al. Towards optimization of selective photothermolysis: prothromic pharmaceutical agents as potential adjuvants in laser treatment of port wine stains – a theoretical study. Thromb Haemost 2005;93:242–56.
Treatment of Port Wine Stains
Port wine stains (PWS) affect 3 in 1000 newborn infants [1,2]. A PWS is a capillary vascular malformation of developmental origin characterized pathologically by ectasia of superficial dermal capillaries [3] and clinically by permanent macular erythema.
Treatment with the PDL has revolutionized the treatment of PWS. Favourable factors for a good response to treatment are: younger age, a pink/red colour (compared with dark purple) and certain anatomical sites [4]. Lateral facial lesions, forehead and neck respond better than the centrofacial region. The most refractory area on the face is often the centre of the cheek. PWS on the lower limbs respond least favourably [5].
The timing of laser treatment depends on the age of patient at presentation to the specialist. Laser treatment is effective at any age but there are substantial benefits to early treatment and we are in favour of referring these children for assessment to a specialist unit soon after birth. This is also important if there is the possibility of any associated medical problem such as Sturge–Weber syndrome or glaucoma. It also allows the parents to be fully informed about what is involved in their child having laser treatment, discussing the possible outcome and the limitations of treatment, potential side-effects and planning a programme of treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








