Modifying Technique by Age and Developmental Stage
It is important to recognize that some reconstructive options are more likely to be successful in children than in adults, and some less so. The developmental age and character of the child will often influence the best option for surgery. For instance, tissue expanders in the lower limb have a lower complication rate in children than in adults, but the child would need to be able to cope with the process of inflation of the expander over a period of time.
The key surgical advantages of younger patients are the better skin quality, particularly in terms of elasticity and vascularity, the lower likelihood of co-morbidities and the lower risk of joint stiffness if immobilization is required postoperatively. Conversely, the disadvantages include the risk of losing co-operation if the child becomes anxious, hence the need for skilled paediatric nurses and avoidance of painful or unpleasant procedures; greater requirement for general anaesthesia, rather than local or regional blockade; the need for skilled paediatric anaesthetists, particularly for younger children; and the requirement to consider the family situation as well as the child. A further crucial requirement is to take account of future growth, particularly where scars or grafts lie close to a joint
Simple technological advances can assist with some of these challenges. For instance, the appropriate use of fine resorbable sutures avoids the anxiety of suture removal and reduces unnecessary general anaesthesia. Similarly, use of non-adherent silicone dressings (Mepitel) can allow pain-free dressing changes, while modern burns dressings (Biobrane) for superficial partial-thickness burns can allow earlier discharge home with less discomfort (see below)
Challenges of More Complex Skin Surgery
Wound Healing
Wound healing has been studied extensively in skin, and there is a distinction between primary healing, which occurs in the incised wound and in which the skin edges are in close apposition, and secondary healing, in which the edges are far apart. During wound healing, there is interaction of cellular and extracellular events such as cell migration, proliferation and differentiation. There is also synthesis and remodelling of extracellular matrix, culminating finally in tissue repair with scar formation. Three phases of wound healing are recognized: (i) the period of haematoma formation, inflammation and removal of foreign material; (ii) the phase of granulation tissue growth and epithelial migration; and (iii) the phase of connective tissue remodelling, wound contraction and scar formation. These phases overlap and occur in both primary and secondary healing but to differing extents. In secondary healing the entire process is prolonged, particularly the second and third phases, and healing relies on the wound becoming smaller. This is due to both wound contraction, which is thought to be mediated by myofibroblasts, and cicatrization (or contracture), which is due to fibrosis. Although the processes causing the wound to shrink in size are useful to wounded animals, they can be disastrous in the case of surgical wounds because they may result in deformity. The surgeon aims to achieve primary healing and prevent secondary wound healing by direct suture of skin edges and also by use of skin flaps and grafts. It is worthwhile counselling parents that even in primary healing, the remodelling phase can be visible for up to 2 years.
The tensile strength of a wound is a measure of its load capacity per unit area. Collagen fibres are largely responsible for the tensile strength of wounds, and the rate of healing varies between species and individuals, as well as between different tissues in the same individual. All wounds gain strength at approximately the same rate during the first 14–21 days. Experiments in the rat have shown that the tensile strength of wounds is 32% at 7 days and 64% at 14 days, and does not reach a maximum until 10 months. Even so, wound tensile strength only reaches about 80% of that in normal skin [1].
Skin Closure and Suture Technique
The surgeon has a choice of methods of wound cover, but a successful outcome in terms of subsequent scarring and cosmetic result is dependent on adherence to basic plastic surgical principles. These are correct planning, accurate approximation of skin edges, measures to minimize wound haematoma, minimal handling of the skin edges, avoidance of excess tension on the skin edge and prevention of unnecessary wound contamination. Factors beyond the surgeon’s control that may cause a poor scar are the age of the patient and the site and also direction of the wound. In general, except for scars in infants (1–3 months), which often heal as fine lines, children’s scars remain erythematous and harder for longer.
The size of the anticipated skin defect influences the surgeon’s choice of wound cover. Small wounds can be closed directly. Conversely, larger defects will require skin flaps or skin grafts and for lesions that do not require immediate excision, techniques such as serial excision and tissue expansion may be employed.
Placement and Alignment of Scar
The vast majority of skin lesions are suitable for excision and direct closure. In general, lesions are excised as an ellipse. The skin of infants and smaller children is very elastic and padded by a type of adipose tissue commonly called ‘baby fat’, which maintains the skin at maximal distension. One consequence of this is that wounds that one may not expect to close directly in older children and adults can be approximated with comparative ease in infants.
When planning elliptical incisions, one is generally taught that the length of the ellipse will be equal to three times the diameter of the lesion, and this is a useful guide when explaining the procedure to patients. However, in reality, one can make the limbs of the ellipse shorter, thus decreasing the length of the final scar. The longitudinal axis of the ellipse should be designed to lie along or parallel to a line of skin tension.
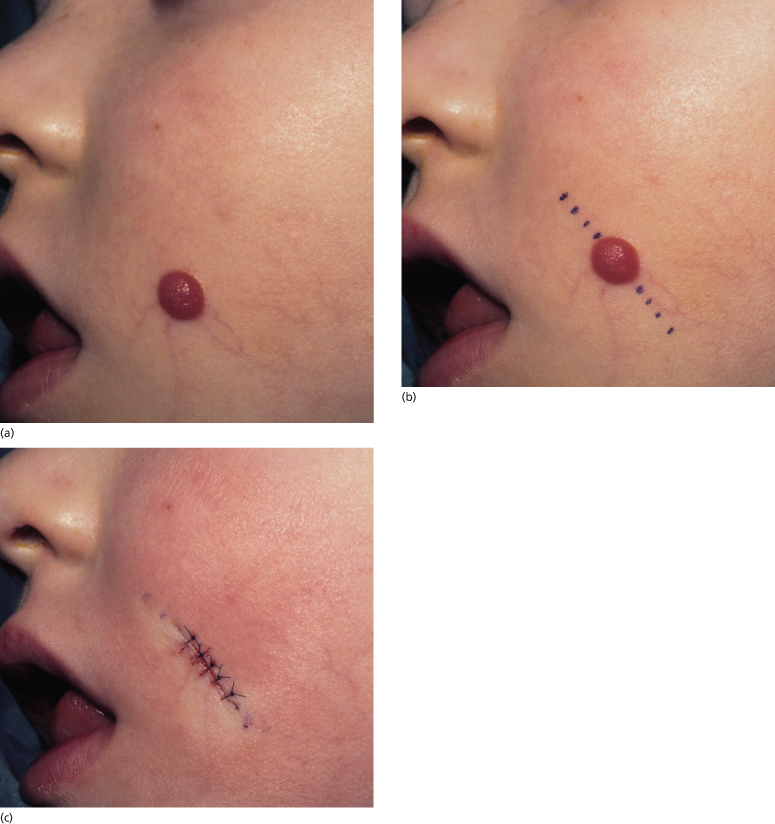
The existence of lines of tension in the skin was first noted by Dupuytren in 1832 [2] and subsequently investigated by Karl Langer [3], Professor of Anatomy at Joseph’s Academy in Vienna. The work was presented in the second of a series of four papers in 1861 [3]. Although some of Langer’s lines run across natural creases, they form the basis of our understanding of lines of skin tension, which have attracted numerous descriptive terms, as listed by Borges [4]. A scar is less conspicuous if it lies along or parallel to a line of skin tension. In the face, these lines correspond to wrinkle lines in elderly people, in whom they are also known as lines of facial expression. In the neck, these lines correspond to the lines of dependency, where the effects of gravity produce horizontal creases. Lines of skin tension also lie horizontally in flexion creases and in the limbs; where it is difficult to choose the correct line, it is preferable to follow the line that falls when the limb is in the relaxed position. In the case of facial surgery in a child, it is often difficult to plan the direction of excision because the skin is stretched and facial lines are absent (Fig. 187.2). In this instance, the excision should be planned so that the scar will eventually lie in a line of facial expression (Fig. 187.3).
Fig. 187.2 Position of skin tension lines corresponding to lines of facial expression in later life.

Fig. 187.3 Excision of a Spitz naevus on a 3-year-old girl. (a) The lines of skin tension are not obvious on the stretched skin of a child. (b) Therefore, the excision should be planned so that the scar falls in a future skin crease. (c) The sutured wound after excision of the naevus as a short ellipse.
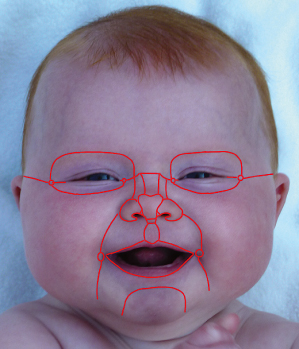
Another principle to follow when planning surgical wounds on the face is to appreciate facial aesthetic units. Figure 187.4 illustrates the position of aesthetic units in a child and to make the scar less conspicuous, whenever possible it is best to orientate the scar at the junction of these units [5,6].
Fig. 187.4 It is important to appreciate the cosmetic units of the face. Scars are less conspicuous if they lie along the border of adjacent cosmetic units.
In many instances the line of excision is dictated by the orientation of the lesion. Figure 187.5 shows a nasal residual haemangioma in which the scar is orientated vertically within the glabellar crease and along the junction of the nasal aesthetic units. Gentle handling of the tissues, minimal skin tension across the repair, meticulous haemostasis and the use of fine sutures will all contribute to the final quality of the scar.
Fig. 187.5 A 4-year-old girl with a large nasal haemangioma. (a) The haemangioma has predominantly regressed to leave fibro-fatty residual tissue amenable to surgical excision. (b) The excision is planned to orientate the subsequent scar at the junction of aesthetic units. (c) Two years following surgery, the scar is fully mature but made more obvious by areas of hyperpigmentation secondary to sun exposure.

To avoid placing an obvious scar on the nose, lesions on the nasal tip can be accessed utilizing plastic surgical techniques commonly used in the adult population. In a 4-year-old girl, an open tip rhinoplasty approach was used to correct a bulbous nasal tip caused by the fibro-fatty residual haemangioma (Fig. 187.6).
Fig. 187.6 A 4-year girl with a fibro-fatty residual haemangioma producing a bulbous nasal tip. (a) More complex plastic surgical techniques are required in this case to excise this lesion in order to maintain a good nasal tip shape. A columella V-shaped incision will provide good access to the lesion and alar cartilages whilst avoiding an obvious scar on the nasal tip. (b) To respect facial cosmetic (aesthetic) units, an open tip rhinoplasty approach is used, delicately elevating the columellar skin to expose the underlying lesion. (c) The fibro-fatty haemangioma can be mobilized from the displaced alar cartilages, which often need central support sutures to maintain the symmetrical nostril shape. (d) Although there is a scar in the collumella, this approach to the nasal tip will give the best aesthetic outcome in these difficult cases.

Common sites for lesion excision in the paediatric population include the scalp (e.g. sebaceous naevus) and eyebrow (e.g. dermoid cysts) in which case scars can be hidden in the hair-bearing skin. In this case, the skin should not be cut perpendicular to the surface, as is the normal teaching, but parallel to the direction of the hair follicles, to prevent their disruption and subsequent localized alopecia. The sex of the child is important when planning excisions within the hair scalp because of the likelihood of later balding in boys [7].
Scars and Problem Scars: Hypertrophic and Keloid Scars
Clinical Features.
Although one hopes that all scars will heal perfectly as thin lines, often this is not the case. In children in particular, there is a significant risk of hypertrophic and even keloid scar formation. There are many similarities between hypertrophic and keloid scars. In both, the pathology is within the dermis, where there is dense hyalinized fibrous tissue with excess collagen deposition that is organized as discrete nodules. Frequently, the rete pegs in the papillary dermis of the lesions are obliterated. Unlike normal dermis, in which collagen is arranged in discrete fascicles separated by interstitial space, the collagen nodules in keloids and hypertrophic scars appear avascular and are arranged in a haphazard manner. Keloid nodules are thought to have a glassy appearance compared with hypertrophic scars.
The distinction between keloid and hypertrophic scars is a clinical one, and it is incorrect to think of them as the same phenomenon that is qualitatively similar but quantitatively different. Keloid scars (Fig. 187.7) are most likely in patients of African origin but also in the Chinese and Celts. In addition, there may be a familial predilection. They can occur at any age but are most prevalent in patients between 10 and 30 years of age [8]. They are rare in very young children [9] and the elderly. Keloids develop a few months after the wound repair, and occur most commonly on the lower face, neck, earlobes, presternal area and back. Their characteristic feature is that they outgrow the boundaries of the original scar, invading surrounding normal tissue. They rarely subside and treatment is largely unsuccessful.
Fig. 187.7 A keloid scar on the ear of a 10-year-old boy after surgery for correction of prominent ears.

Hypertrophic scars are less associated with racial origin and have a lower familial tendency. They can occur at any age but are most frequent below the age of 20 years. Hypertrophic scars develop a few weeks after injury and are prevalent on scars across flexor surfaces (Fig. 187.8). Hypertrophic scars stay within the boundaries of the original scar and subside over a 2–3-year period. Patients are troubled by the appearance of the scar, persistent itching and contracture.
Fig. 187.8 Hypertrophic scars on the flexure aspect of a 12-year-old girl. She had hypertrophic burn scars that were revised when the scars were thought to be inactive, but the new wounds also became hypertrophic.

Aetiology.
Clues to the aetiology of both hypertrophic and keloid scars lie in some clinical observations. Both types of scars are common in some areas, such as the sternum and shoulders. Hypertrophic scars often occur where the axis of the wound crosses natural lines of skin tension rather than running parallel to them. This gave rise to the theory that abnormal mechanical stresses are an important trigger of hypertrophic scarring. Hypertrophic scars are very common following a burn injury, particularly in children (Fig. 187.9). Interestingly, they seldom occur in superficial burns that have healed in less than 2 weeks, but are likely to form at sites where the burn injury was deeper and the wound slow to heal [10]. Similarly, parts of wounds that dehisced and became infected are also more likely to become hypertrophic than areas of uneventful primary healing.
Fig. 187.9 Severe hypertrophic scars are common following burns, as on this 3-year-old boy who sustained deep partial-thickness burns. The scars can mimic keloids but do not extend beyond the boundary of the original wound.

Other theories for the aetiology of hypertrophic and keloid scars include the suggestion that there were abnormalities of the immune system, but Cohen et al. [11] were unable to show any derangement of local or systemic immune factors. Tissue culture and biochemical studies have confirmed the increased production of collagen in keloid scars. Furthermore, fibroblasts that have been isolated from keloid scars continue to overproduce collagen when in culture. Hence, it appears that once the fibroblasts have been stimulated to behave abnormally, they continue to do so even when removed from the abnormal environment [12]. Specific collagen studies have shown that the overproduction is mainly of collagen type I and not type III that is seen in wound healing. One popular concept is that hypoxia may stimulate or be responsible for the propagation of hypertrophic and keloid scars. Kischer et al. [13] observed increased occlusion of the microcirculation within lesions due to endothelial cell proliferation. It was hypothesized that perivascular myofibroblast contraction may contribute to microvascular occlusion. The resulting hypoxia could stimulate endothelial hyperplasia, causing further hypoxia, which would eventually lead to excess collagen production. Numerous dysregulated genes have been identified in cases of keloid scarring, with variable inheritance patterns [14].
The symptom of severe itching in hypertrophic scars has attracted some interest and a high concentration of neuropeptides has been shown in hypertrophic scars compared with normal skin [15]. These may be responsible for the itching but, as some neuropeptides are trophic agents, it has even been suggested that they may stimulate growth of the abnormal scars.
Treatment.
Hypertrophic scars by their nature will regress with time. However, at the earliest suggestion that a scar may become hypertrophic, it is advisable to institute preventive measures. The mainstay of management is the use of pressure garments [16]. Quinn [17] introduced the use of silicone gel for hypertrophic and keloid scars. To be effective, silicone gel needs to be applied for at least 12 h per day. As a practical guide, as soon as a wound is seen to be hypertrophic, and in all healed burn wounds, the authors would advocate the use of pressure garments (Fig. 187.10) in conjunction with silicone gel, which can be worn inside the garment, for a minimum period of 6 months. Children cope very well with this regime, but occasionally some develop an atopic sensitivity to silicone gel.
Fig. 187.10 Pressure garments, sometimes with silicone gel applied directly on the scar, form the mainstay of treating hypertrophic scars in burns. They need to be worn for at least 6 months and usually for 2–3 years.

Intralesional steroid injections can be used for hypertrophic scars, but surgery is not advised in the active phase when scars are red and itchy. Thereafter, options for surgical treatment include excision and direct closure, but this may result in scar recurrence. Alternatives are the use of Z-plasty techniques to realign the direction of the scars to lie parallel with the lines of skin tension or to introduce local unaffected flaps to relieve tension and break up the scar.
Treatment of keloid scars is frustrating. Surgical excision alone is unlikely to be successful, and the lesions are likely to recur and may be larger than their original size. Intralesional excision is thought to be less harmful as it does not damage normal tissue, although a recent retrospective study suggests that there is a lower rate of recurrence with complete excision [18]. Intralesional steroid injections can in many instances decrease the size of keloids. It is the authors’ practice to use intralesional injections of triamcinolone 10 mg/mL (maximum 1 mL) at 6-week intervals. A minimum of three injections is necessary before the benefit of the treatment can be assessed. In young children, the injections may need to be administered under general anaesthesia. If steroid injections are unsuccessful, the next option would be to combine intralesional surgical excision with postoperative steroid injections. Complications of steroid injections such as local fat atrophy and depigmentation are due to extravasation into normal tissue.
Many workers have used radiotherapy following excision of keloids, but the authors do not recommend its use in children owing to the risk of future malignancy. However, patients are often willing to take that risk, such is the social stigma from keloids.
It is remarkable how little has changed in the treatment of keloid scars over the last 20 years, and how little high-quality evidence is available to guide treatment choices [19]. A summary of various regimes of surgery, radiotherapy and steroids in the treatment of keloids was published by Lawrence [20]. Although quantitative comparison of published data is not possible owing to numerous variations in patient cohort and treatment protocols, the summary nevertheless provides an impression of treatment efficacy. Analysis showed that steroid injections alone had a mean success rate of 66%. Surgery alone had a mean success rate of 28%, which increased to 52% when combined with postoperative steroid injections and to 75% with radiotherapy.
Research into the reduction of scarring remains frustrating and often controversial in what would be a lucrative market. Renovo, a British company focusing on skin treatments, is planning phase III trials for its product, which is an intradermal injection of transforming growth factor β3 (TGFβ3) intended to reduce scarring and thus have applications in the treatment of hypertrophic and keloid scars. The results of three trials already completed were published in the Lancet, along with an editorial commentary [21], and the results of phase III are planned to be available in 2011.
Scar Revision
There should be little reason for scar revision following elective surgery. Local skin flaps may be bulky initially, but the vast majority settle down with time. The majority of patients who request scar revision are those with wounds that were the result of trauma or that have contracted unexpectedly or become hypertrophic. Scars are unsightly if they are tethered to the underlying muscle or fascia, contracted, raised or widened. Circular scars contract to produce a pin-cushion effect of the normal tissue within the scar.
It is essential to allow scars to mature before attempting revision, which means waiting for the itching and redness to resolve. It is the authors’ practice to wait for a minimum of 1 year in adults and 2 years in children before considering revision. In that time, scar remodelling and softening may be such that further surgery is unnecessary. If children are in their early teens, it may be worthwhile waiting until they are 17 or 18 to reduce the risk of hypertrophic scar formation. Prior to surgery, it must be stressed to the patient or parent that the original deformity may recur or even be worse. It is also important to pinpoint the exact feature of the scar that the patient dislikes and avoid excessive corrective surgery.
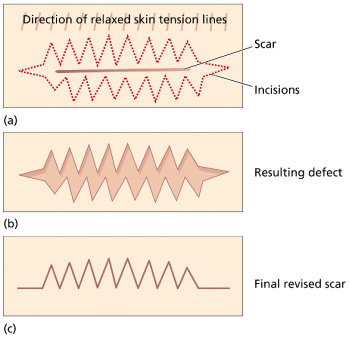
Surgery for scar revision is one of the most challenging in plastic surgery. Much scar revision involves excision of the scar with untethering of the local tissue, and then reapproximation of appropriate tissue layers. Sometimes, the scar can be de-epithelialized and buried subcutaneously to provide a firm anchor to the repair and correct a sunken contour deformity. If a scar is unsightly because it lies across a natural line of skin tension, then attempts can be made to realign the scar with the techniques of Z-plasty (Fig. 187.11) or W-plasty (Fig. 187.12). The details are quite complex and outside the limits of this text [7,22,23] but in principle, if a straight scar is up to 35° across a line of skin tension, a Z-plasty is chosen. If the angle is between 35° and 90°, a W-plasty is performed with multiple small flaps with acute angles.
Fig. 187.11 A Z-plasty can also be used to change the direction of a scar so that it falls into a line of natural skin tension. (a) The scar initially passes across the line of relaxed skin tension which is along the nasolabial groove. Thus, it would be very noticeable during normal facial expressions. (b) After excision of the scar and transposition of the flaps, the central limb of the scar is along the nasolabial groove. The price is two further scars from the lateral limbs of the Z-plasty. However, with good planning these will also fall in or close to lines of relaxed skin tension and the final scar will be less noticeable than the original.
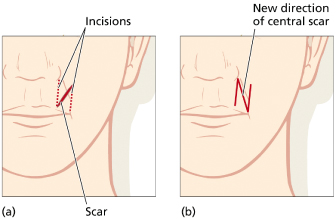
Fig. 187.12 A W-plasty is an alternative to a Z-plasty and is indicated when the angle between the scar and relaxed skin tension lines is between 35° and 90°. (a) The scar is excised with a running W incision. Closure of the resultant defect (b) produces a zig-zag scar where each limb of the scar is close in alignment with the skin tension lines.
References
1 Levenson SM, Geever EF, Crowley LV et al. The healing of rat skin wounds. Ann Surg 1965;161:293–308.
2 Dupuytren G. Leçons Orales de Clinique Chirurgicale Faites à l’Hôtel-Dieu de Paris. Paris: Baillière. 1832, p. 4.
3 Langer K. Zur Anatomie und Physiologie der Haut. [On the anatomy and physiology of the skin (translated by T. Gibson)]. Br J Plast Surg 1978;31:3–8, 93–106, 185–99, 273–8.
4 Borges AF. Elective Incisions and Scar Revision. Boston: Little, Brown, 1973.
5 Menick FJ. Nasal reconstruction. Plast Reconstr Surg 2010;125(4):138e–150e.
6 Roldan JC, Teschke M, Fritzer E et al. Reconstruction of the lower lip: rationale to preserve the aesthetic units of the face. Plast Reconstr Surg 2007;120(5):1231–9.
7 McGregor IA. Fundamental Techniques of Plastic Surgery, 8th edn. Edinburgh: Churchill Livingstone, 1989.
8 Ketchum LD, Cohen IK, Masters FW. Hypertrophic scars and keloids: a collective review. Plast Reconstr Surg 1974;53:140–54.
9 Moustafa MFH, Abdel-Fattah AFMA. Keloids of the earlobe in Egypt. Their rarity in childhood and their treatment. Br J Plast Surg 1976;29:59–60.
10 Egro FM, O’Neill JK, Briard R et al. Pediatric superficial scald burns – reassessment of our follow-up protocol. J Burn Care Res 2010;31(1):196–9.
11 Cohen IK, McCoy BJ, Mohanakumar T et al. Immunoglobulin, complement, and histocompatibility antigen studies in keloid patients. Plast Reconstr Surg 1979;63:689–95.
12 Cohen IK, Keiser HR. Collagen synthesis in keloid and hypertrophic scar following intralesional use of triamcinolone. Surg Forum 1972;23:509–10.
13 Kischer CW, Theis C, Chavapil M. Perivascular myofibroblasts and microvascular occlusion in hypertrophic scars and keloids. Hum Pathol 1982;13:819–24.
14 Shih B, Bayat A. Genetics of keloid scarring. Arch Dermat Res 2010;302(5):319–39
15 Crowe R, Parkhouse N, McGrouther DA et al. Neuropeptide containing nerves in painful hypertrophic scar tissue. Br J Dermatol 1994;130:444–52.
16 Larson DL. Contracture and scar formation in the burn patient. Clin Plast Surg 1974;1:653–6.
17 Quinn KJ. Silicone gel in scar treatment. Burns 1987;13:S33–40.
18 Tan KT, Shah N, Pritchard SA et al. The influence of surgical excision margins on keloid prognosis. Ann Plast Surg 2009;64(1):55–8.
19 Durani P, Bayat A. Levels of evidence for the treatment of keloid disease. J Plast Reconstr Aesth Surg 2008;6(1):4–17.
20 Lawrence WT. In search of the optimal treatment of keloids: report of a series and review of the literature. Ann Plast Surg 1991;27:164–78.
21 Ferguson M, Duncan J, Bond J et al. Prophylactic administration of avotermin for improvement of skin scarring: three double-blind, placebo-controlled, phase I/II studies. Lancet 2009;373:1264–74. Commentary 373:1226–8.
22 Borges AF. Improvement in anti-tension-line scars by the W-plasty operation. Br J Plast Surg 1959;12:29–33.
23 McGregor IA. The theoretical basis of the Z-plasty. Br J Plast Surg 1957;9:256.
Methods of Wound Cover
Primary, Delayed and Secondary Closure
Primary healing occurs when a wound is closed within hours of its creation, which is desirable especially in the paediatric population. Delayed primary healing occurs in contaminated or poorly delineated or dehisced wounds left open to prevent wound infection. The skin and subcutaneous tissues are left unopposed and closure is performed after the normal host defences are allowed to debride the wound. Collagen metabolism is undisturbed and the wound achieves strength as if it had been primarily closed.
Healing of partial-thickness wounds principally involves the epithelium and the superficial portion of the dermis and occurs by epithelialization. Epithelial cells within the dermal appendages, hair follicles and sebaceous glands replicate to cover the exposed dermis. There is minimal collagen deposition and an absence of wound contraction.
Secondary healing occurs when open full-thickness wounds are allowed to close by wound contraction secondary to the action of myofibroblasts and subsequent epithelialization. There is an increased risk in secondary healing for the subsequent scar to be wide, unsightly and with a tendency to become hypertrophic.
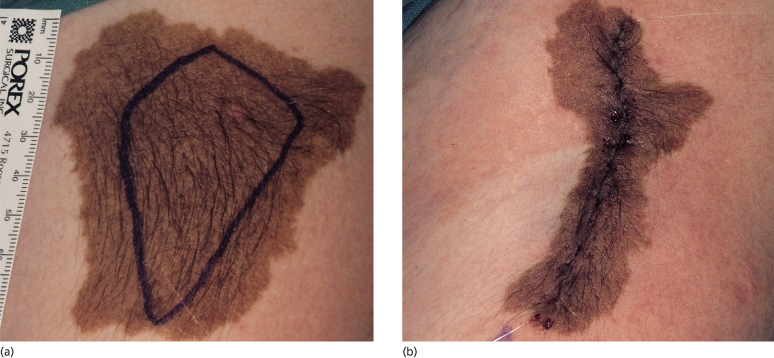
Serial Excision
On occasions when a large benign lesion has to be excised, it may be possible to excise it in two or more stages (Fig. 187.13). This technique utilizes the ability of the surrounding skin to ‘expand’ over time. At each stage of the serial excision, the amount of lesion that is excised is the maximum that will allow the wound to be closed comfortably without undue tension. If a wound is closed with excessive tension, the scar will stretch sometimes to a width resembling the size of the original lesion. These staged excisions are planned so that the vertical length of the scar barely exceeds the longest diameter of the lesion. In all but the final stage, the excisions are intralesional, as are the suture holes. Although individual patient variations exist, often it is possible to plan subsequent stages of excisions after a minimum of 3 months.
Fig. 187.13 First stage of serial excision of scar. (a) This 12-year-old girl had a large pigmented congenital naevus on her left arm. The planned area of excision is marked. (b) Following the first-stage excision, note that the suture marks are intralesional. A further stage of excision is planned to remove the remnant lesion.
Skin Graft
Skin grafts offer the simplest method of covering defects that are too large for direct closure. Skin grafts are sheets of skin that are completely detached from their source of origin, so rendering them avascular. Following transfer to a recipient site, their survival depends on acquiring a new blood supply from the wound bed.
Skin grafts contain epidermis and variable amounts of dermis. If the entire thickness of dermis is included, they are described as full-thickness grafts, whereas if there is a variable amount of dermis they are called split-thickness grafts (Fig. 187.14).









