Full-thickness skin removal is particularly appropriate if the lesion might involve the entire skin thickness (skin tumours, contracting scars) and enables pathological anatomical assessment. If the scar is placed within a wrinkle, the result is often better than after removal of partial thickness of the skin and epithelialization.
Subcutaneous Tissue Removal
If the lesion is located subcutaneously, surgical excision is usually indicated. Depending on its quality, the overlying skin will be incised or excised. The skin will be incised in full thickness, with consequent induction of a scar. In vascular deformities, laser ablation coagulates small vessels (especially capillaries) without damaging the skin and consequently without leaving a visible scar. Sometimes the scar is placed at a less obvious site (e.g. facelift incision for facial tumours or in hair-bearing skin for a subcutaneous forehead tumour). Using endoscopically assisted techniques results in smaller scars.
Wound Closure
Primary Versus Secondary Wound Healing
Wound closure occurs by primary (surgical) wound healing or by secondary (natural) wound healing.
- When a wound is closed surgically, primary wound healing occurs: wounds heal faster and more optimally. It is essential that the margins of the defect are apposed properly so that the wound edges are exactly sutured to each other in the same level. Dissolvable suture material is preferable in children, thereby minimizing the need for later removal of sutures.
- Secondary wound closure is the natural way of wound healing: an open wound closes by contraction and epithelialization from the wound margins. This will generally create more obvious scars. Only for small lesions (several millimetres) should secondary wound healing be considered.
The normal healing process should be explained to children and parents. Scars develop to varying degrees; there is typically a phase of redness and thickening, with potentially lasting broad scars.
Surgical Wound Closure
Surgical wound closure can be divided into three groups:
- primary wound closure;
- wound closure with autologous non-vascularized tissue;
- wound closure with autologous vascularized tissue.
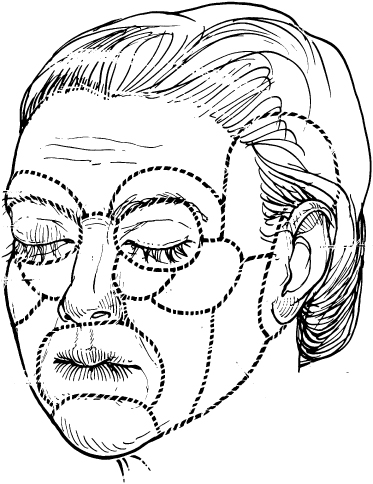
Preferably the scars are placed within the wrinkle lines of the skin or at the margins of anatomical units. Then they will be less obvious (Fig. 186.3).
Fig. 186.3 (a) Incisions are placed at the anatomical margins of the facial units. (b) Inconspicuous scars in the same patient 2 years after surgery.

Primary Wound Closure
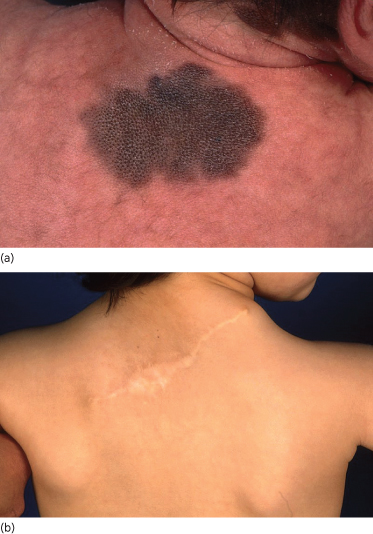
A wound can be closed primarily if the surrounding skin possesses enough elasticity to allow exact approximation of the vital wound margins with limited residual tension on the sutures. Children have relatively more excess skin, allowing primary closure in most cases (Fig. 186.4). Advantages of the (young) age of children include the relative excess of skin and its increased regenerative capacity, allowing larger resections of lesions than in adults. The increased regenerative capacity allows staged removal of larger lesions. In this way, especially small to moderately large skin lesions or even local alopecia can be treated. Ideal indications are patients with excess of skin (e.g. cutis laxa or Ehlers–Danlos).
Fig. 186.4 (a) Large congenital naevus. (b) Scar 3 years after complete excision and primary closure of the wound.
Wound Closure with Autologous Non-Vascularized Tissue
If direct skin closure is impossible, the wound can heal quickly by application of skin grafts, which provide a new epithelium. A full-thickness skin graft (FTG) contains the entire dermis with the hair follicles, sebaceous glands and sweat glands. A partial-thickness or split-thickness skin graft (SSG) contains only partial dermis without the complete array of skin appendages (Fig. 186.5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree