17 Brachioplasty with Interdigitation of the Posteromedial Scar

Abstract
As variable deformities of the upper extremity result after massive weight loss, a one-size-fits-all approach to brachioplasty is doomed to leave both patients and surgeons dissatisfied. The surgical strategy can be reasonably adjusted based on a systematic evaluation of an individual’s brachium, axilla, and upper-lateral chest wall. This chapter outlines the authors’ approach to the pre-operative analysis of the upper extremities, explains the rationale for selecting a surgical approach based on the extent and severity of a patient’s deformity, and details our technique of brachioplasty for patients who have marked brachial skin laxity. Our approach to brachial rejuvenation involves excision of excess skin along the posteromedial aspect of the arm using interdigitating incisions in conjunction with a Z-plasty of variable size and extent to restore normal contour to the axilla and upper-lateral chest wall.
Introduction
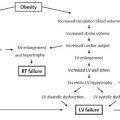
Upper extremity deformities of varying severity are seen with aging, normal weight loss, and massive weight loss such as occurs following bariatric surgical procedures. As a person loses weight, a variable amount of subcutaneous fat is lost from the upper extremity. Additionally, skin elasticity decreases with advancing age and can be markedly decreased after the dermis is stretched by massive weight gain. Several patterns of deformity arise, depending on the extent of fat deposition on the arm at the time of maximal body weight, the degree of weight loss, and the residual elasticity of the skin.1,2 The mildest cases of upper extremity contour deformity manifest as lipodystrophy without excess skin, whereas the most severe occur as a combination of both excess skin and fat extending from the elbow onto the lateral chest wall. The most severe deformities frequently occur after extreme weight loss, with the resultant deformity taking the form of what might appear to be a bat’s wing.3
Various techniques for surgical management of upper extremity contour deformities have been suggested since aesthetic brachioplasty was first described in the 1950s by Correa-Iturraspe and Fernandez.4 A large number of brachioplasty techniques have been reported in the literature, and many are based on elliptical incisions3,5–10 that produce a scar along the bicipital groove. Significant common problems have been reported from these techniques ( Table 17.1 ).6,11–18
Indications
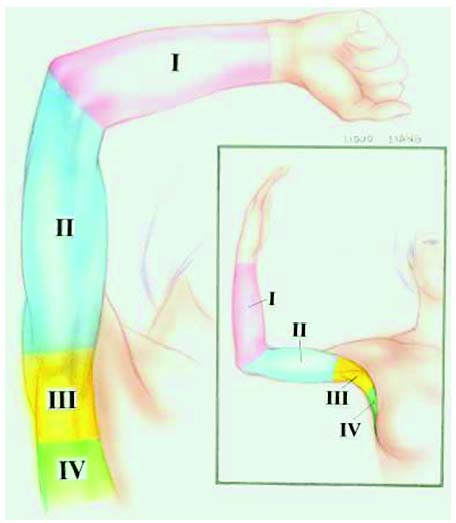
We have previously characterized deformities of the upper extremity using a four-zone system.3 A rational surgical plan can be developed based on analysis of a patient’s deformity using these zones. The upper extremity, axilla, and upper-lateral chest wall are divided into four zones: zone I extends from the wrist to the medial epicondyle, zone II extends from the medial epicondyle to the proximal axilla, zone III is the axilla itself, and zone IV starts at the inferior axilla and extends onto the chest wall ( Fig. 17.1 ).
Deformities limited to zone I generally result from an excess of fatty tissue without significant excess skin. Such deformity is generally amenable to treatment with liposuction.2 Zone II deformities present more variably. The extent of excess skin and its elasticity will dictate whether contour abnormalities of zone II can be effectively treated with liposuction alone, or liposuction in combination with limited excision, or whether extensive excision is required.1 In borderline cases, when liposuction may significantly, but not fully, correct a patient’s deformity, it is especially important to educate the patient about the differences in scarring and contour that can be expected from each of these different techniques. Only a well-informed patient can understand the trade-offs in scarring and contour that are the product of these different surgical approaches.
Combined zone deformities are almost always the result of significant skin excess with a variable amount of lipodys-trophy. Importantly, the proportion of excess skin for the massive weight loss patient is almost invariably, in our observations, greater than that of excess fatty tissue. The excess skin typically hangs from the posteromedial aspect of the arm. We believe that treatment of deformities of combined zones II and III, as well as combined zones II, III, and IV, is generally best achieved by brachioplasty with interdigitation of a posteromedial scar.
Technique
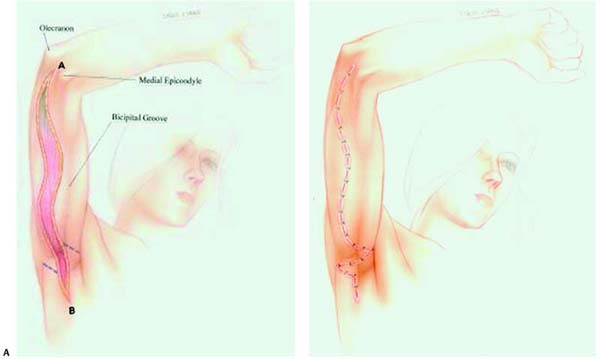
Prior to surgery, the patient is marked in the standing position with the arms abducted at the shoulder and flexed to approximately 90 degrees at the elbows. The surgeon then visualizes or marks a line along the long axis of the arm from a point midway between the olecranon and the me-dial epicondyle and the end of the excess tissue either in the axilla or on the chest wall, depending on the nature of the deformity. An undulating incision is planned on each side of this reference line; the incisions are planned so that they will interdigitate after the intervening tissue is resected. The incisions must converge at their terminal ends and should be marked so that, when the patient’s arms are resting at the sides in the anatomic position, the final scar lies on the posteromedial aspect of the arm posterior to the medial bicipital groove. Pinch-testing while marking will help the surgeon achieve the desired final scar position and avoid overresection.
Once the initial markings are completed, the patient receives a dose of preoperative antibiotics and prophylaxis for deep venous thrombosis (DVT). The patient is placed under general anesthesia, and, if necessary, the markings are refined. The skin and superficial subcutaneous tissue are next sharply incised along the sinuous markings down to the level of the underlying muscle fascia. The subcutaneous tissue between the incisions is elevated off the muscular aponeurosis. Injury to the ulnar nerve and superficial sensory nerves must be avoided at this stage.13 Minimizing undermining is important, as the incidence of seromas and lymphedema has been shown to be reduced when undermining is avoided.19–21 Laxity of the remaining skin should permit easy closure without the need for undermining. The surgeon inexperienced with brachioplasty may wish to initially make only one incision, elevate the tissue to be resected, confirm the position of the second incision, and tailor tack with towel clamps.18


A Z-plasty is planned within the axilla such that the final transverse limb will lie in the axilla’s apex. The parallel limbs of the Z are marked at approximately 60-degree angles to the central limb; the central limb is formed by the segments of the sinuous brachioplasty incisions that lie within the axilla. When necessary, the sinusoidal incisions are extended medial to the Z-plasty to facilitate resection of tissue in zone IV ( Fig. 17.2 ).
Closed suction drains are placed and are brought out through the medial aspect of the surgical site. Incisions are closed in three layers: the superficial fascial system, deep dermis, and subcuticular layer. The wounds are dressed with Xeroform, Telfa, and gauze; Kling and an Ace wrap are then applied to the upper extremity beginning at the wrist.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree