* R. Hansen, personal communication.
Pathogenesis.
The aetiology of CEVD has not been established. The presence of this finding in one of identical twins and the absence of other affected individuals in the families suggests that a non-hereditary intrauterine event is responsible. Amniotic bands or other localized defects associated with the development of fetal skin can be readily excluded. The amniogenic theory that was proposed to explain the pathogenesis of congenital absence of the skin may be operative [5]. According to the theory, amniotic adhesions resulting from an unknown inflammatory process place traction on the developing fetal skin. Tearing of these adhesions in the perinatal period might produce cutaneous ulcerations in the newborn. However, the extent of the ulcerations, the associated vesicles, the reticulated pattern of scarring and oral involvement would be difficult to explain on that basis. Furthermore, placentas and membranes were noted to be normal in a number of the patients.
Several findings suggest a vascular cause. In case 2, placental infarcts were found at delivery, and hepatomegaly and bony changes on radiographic films were noted in the neonatal period [1]. Patient 3 had hepatomegaly associated with intra-abdominal calcifications and mild right cerebral atrophy that was discovered on a computed tomography (CT) scan at 2 years of age [1]. In case 6, a gangrenous area was noted on the right index finger at birth [2]. Multiple infarcts, or perhaps an associated vasospastic phenomenon, might have produced necrosis in a reticulated pattern and visceral defects.
Pathology.
The skin biopsy findings from affected children after the neonatal period demonstrated changes consistent with scarring [1–4]. Although the overlying epidermis was normal, the dermis showed a variable increase in collagen and decreased or absent adnexal structures. Several children have also been reported to develop recurrent blisters in areas of old scarring. The histological findings in the recurrent vesicles in case 8 showed a non-specific spongiotic dermatitis and probably represent recurrent blistering in fragile atrophic scars. Direct immunofluorescence was non-specific and electron microscopy was normal.
Three children were biopsied during the first few days of life. Histological findings in case 7 [3] showed a diffuse neutrophilic infiltrate with a few eosinophils and histiocytes [4]. In case 8, a distinct subepidermal blister was noted, with a mixed inflammatory dermal infiltrate composed primarily of eosinophils (R. Hansen, personal communication, 1997). Eosinophilic spongiosis was seen in one area that was not contiguous with a vesicle. In both cases, direct immunofluorescence was negative or non-specific. In the most recent case, epidermal necrosis and mixed dermal inflammation were noted [6] (R. Hansen, personal communication, 1997).
Electron microscopy of the scarred lesions from case 12 demonstrated granular deposits in keratinocytes but was normal in similar lesions from case 14 [7,12].
Clinical Features.
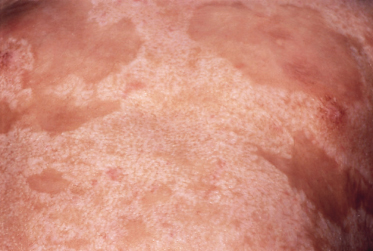
The early clinical course in these patients was remarkably similar. All but two of these children were born prematurely, and an extensive cutaneous eruption was noted at birth (Fig. 16.1). Large areas were covered with reticulated crusts, ulcerations, scattered intact vesicles and haemorrhagic patches. Lesions healed quickly during the first few months of life, leaving widespread supple reticulated scars (Fig. 16.2). With the exception of three patients, no new lesions appeared after the neonatal period, and the reticulated scars have gradually flattened and became less noticeable. Even in children in whom involvement of the scalp was severe, there has been some improvement. In three patients, occasional recurrent blistering has been described in areas of previous involvement [6] (R. Hansen, personal communication, 1997). These recurrences probably result from mechanical trauma to areas of increased skin fragility from atrophy and fibrosis. Skin biopsies from recurrent blisters have shown non-specific dermatitic changes [6] (R. Hansen, personal communication, 1997).
Fig. 16.1 At birth, case 8 demonstrated widespread erosions and crusting involving (a) the trunk and (b) the extremities and face.
Courtesy of R. Hansen.

These patients were from varying ethnic backgrounds and different parts of the world. There was no history of consanguinity in any of the families and, with the exception of the mother of patient 3, there was no history of increased fetal wastage. With the exception of case 4, parents denied a family history of cutaneous, skeletal, ophthalmological or neurological defects.
The physical findings were also similar in these children (Fig. 16.3). Symmetrical reticulated scarring involved at least 75% of the skin surface. Elevated bands were normally coloured to minimally hyperpigmented. Scars on the trunk and forehead were cobblestone-like and, in some areas, orientated along skin cleavage lines. On the limbs, the reticulated pattern followed the long axes of the extremities.
Fig. 16.3 At 5 years of age, case 2 (a) shows widespread supple and reticulated scars on the back and case 3 (b) shows them on the upper arm.
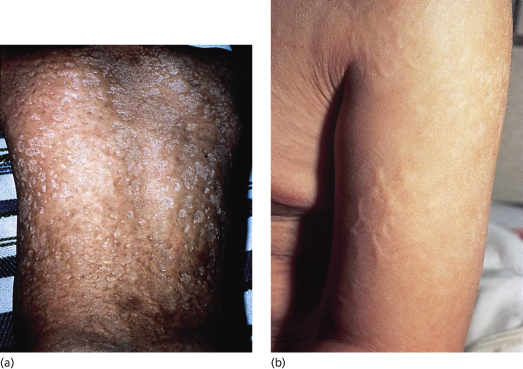
Although all parts of the skin surface were involved, in most cases there was relative sparing of the face, palms and soles. Despite the scarring, all joints were mobile and functionally unimpaired. Although alopecia in patients with scalp involvement tended to improve with increasing age, permanent hair loss was noted in areas with scarring.
Eyebrows and cilia were normal in all patients except one who had recurrent bilateral conjunctival injection and crusting associated with partial absence of eyelashes (case 8) and one who had scarring of the eyelids (case 6). Seven children had nail involvement with partial loss of nails and nail dystrophy. Five patients had scarring of the dorsal aspect of the tongue, and one had scarring of the buccal mucosa. All of the older children experienced hyperthermia, especially during hot weather. All patients adapted by avoiding intense sun exposure and taking rest breaks during active play.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree