15 Endoscopic Forehead and Midface Lift
Introduction
Facial harmony, which is an essential component of an aesthetically pleasing face, is gradually lost as a result of aging. This is often dramatically reflected in the upper twothirds of the face with the development of lateral sagging of the eyebrows and hooding of the upper eyelids. The concomitant vertical elongation of the lower eyelids, cheek descent, and loss of volume with exposure of the infraorbital rim creates the double convexity deformity of the lower lid.
The concept of elevation of the eyebrow has been around for nearly a century since its first description. 1 Almost 50 years later, descriptions of forehead lift with temporal incisions 2 and subperiosteal release of the orbital ligament started to appear in the literature. 3 , 4 , 5 Building on these concepts, surgeons started to use endoscopes to assist in the subperiosteal elevation of the forehead performed through a transtemporal approach. 6 , 7 , 8 , 9 Around the same time, with the introduction of the deep-plane rhytidectomy, the midface started to receive a lot more attention. 10 Because the deep-plane rhytidectomy offered a suboptimal, more lateral, vector of pull for the midface, several other techniques were developed to address this anatomical region, such as the same transtemporal approach used for forehead dissection. 11 , 12 , 13 Since then, endoscopic forehead and midface lift gained wide popularity due to its reliable and reproducible results and limitation of the morbidity related to the open approaches. Patients also were understandably more attracted to an option with shorter scars and that was perceived as less risky in terms of an unnatural result or complications. Further experience expanded the confidence that this technique can be used for older patients with more advanced upper face aging and that scalp removal is not really necessary to produce a longlasting improvement in forehead appearance. Over the last two decades, a plethora of articles have been published describing modifications and refinements of the endoscopic forehead and midface lift. However, perhaps the biggest advancement in the rejuvenation of this anatomical region was a better understanding of the aging changes that occur in the area.
In order to achieve a successful outcome in brow and midface lifting surgery, the surgeon needs to have not only a thorough understanding of the anatomy and age-related changes but also a sharp aesthetic eye for the ideal brow and cheek position. Once these principles are well understood, the technical details and peculiarities of one or another particular technique will guide the surgeon on how to achieve a longlasting brow elevation, a natural look, and a pleased patient.
Surgical Anatomy for Endoscopic Forehead and Midface Lift
Surgeons often contrast “surgical anatomy” with anatomy to distinguish the unique perspective of the operative field from the gross anatomy lab. “Endoscopic anatomy” is an additional perspective that the facial plastic surgeon must master. Through the endoscope, familiar structures are viewed in an unfamiliar manner; therefore, a thorough knowledge of the anatomy of the forehead and midface musculature, the fascial planes, and nerves is indispensable.
Muscles
The forehead muscles have an important role in facial expression and are an important part of the rejuvenation process. There are five muscles that are divided into brow elevators and depressors. The only brow elevator muscle is the frontalis muscle. The brow depressors are the corrugator supercilii, procerus, depressor supercilii, and orbicularis oculi. The corrugator supercilii is the largest of the brow depressors and has two heads: a transverse and an oblique, which will produce the vertical and oblique glabellar lines. The procerus produces the horizontal glabellar lines. The medial portion of the orbicularis is a medial brow depressor and provides some contribution to the glabellar lines, whereas its lateral portion is a lateral brow depressor and will create the wrinkling pattern known as crow’s feet.
Fascial Layers and Fat Pads
The galea aponeurotica covers the upper part of the cranium. As the galea extends anteriorly into the forehead, it splits into superficial and deep layers enveloping the frontalis muscle. On its deep surface, the galea is attached to the pericranium by loose cellular tissue, creating a gliding plane, which allows the aponeurosis carrying the skin to move through a considerable distance. Lower in the forehead, the deep galea layer will further split. It will obliterate the subgaleal plane attaching to the pericranium and creating a fixation point at about 2 to 2.5 cm above the rim. Below this point, it will envelop the galeal fat pad, creating a separate glide space that will allow further brow mobility. 14 The galea fat pad extends transversely over the superior orbital rim for about 2.5 cm deep to the frontalis muscle and is suspended by the deep galea fusion with the periosteum of the orbital rim. It has been noticed that over the lateral rim, this fascial suspension is somewhat lower and sometimes absent, which would allow this fat pad to descent. 15 The more inferior portion of the galeal fat pad, underneath the preseptal and orbital portion of the orbicularis oculi, is called retro-orbicularis fat pad. 16 This fat pad extends from the supraorbital notch laterally, beyond the lateral orbital rim.
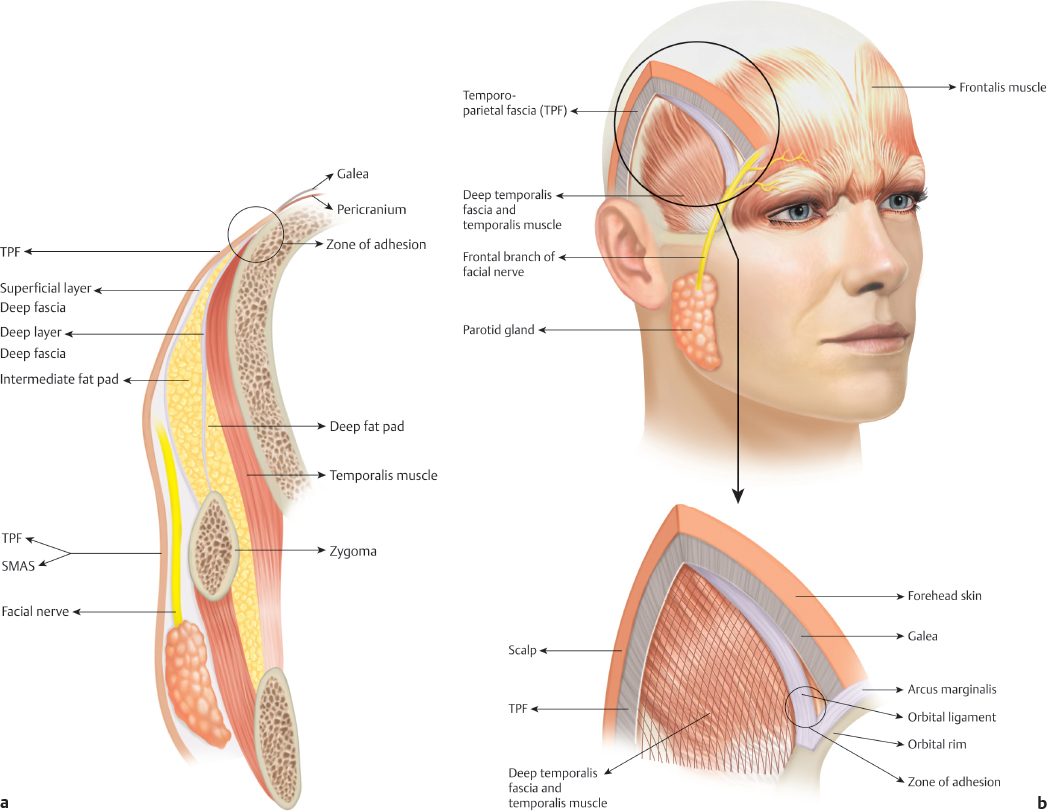
Laterally, the galea continues as the superficial temporal fascia (or temporoparietal fascia [TPF]). Inferiorly, this layer will be the direct extension of the superficial musculoaponeurotic system above the zygomatic arch. The TPF has surgical anatomical importance due to the fact that the frontal branch of the facial nerve, along with the superficial temporal vessels, course within this layer. Deep to this fascia lies the deep temporal fascia, which is divided into a superficial and a deep layer. The superficial layer attaches in the lateral aspect of the zygomatic arch while the deep layer attaches in the medial aspect. These two layers envelop the intermediate temporal fat pad. 17 Underneath the deep layer is the deep temporal fat pad. Overlying the temple and the lateral brow region, the superficial temporal fascia is firmly bonded to the overlying skin while it is loosely attached to the deep temporal fascia. The skin over the temple can move up to 2.5 cm. 15 The only area of sturdiness of this fascia is its insertion on the frontal bone along the rim of the temporal fossa. This structure is called zone of adhesion or fixation and is about 6 mm wide. 18 This is a confluence of the deep galea plane and pericranium on one side and all layers of the temporalis fascia on the other side, with a firm anchoring over the frontal bone. At its inferior end, the superficial temporal fascia forms a condensation creating a ligamentous structure that attaches the superficial fascia to the superolateral orbital rim called orbital ligament. This structure firmly attaches to the frontozygomatic suture and, because the TPF is firmly engaged to the skin of the temple, it will tether the skin and lateral eyebrow to the orbital rim ( Fig. 15.1 ). The medial extension of this ligament is the arcus marginalis, which is the fusion of the orbital septum with the periosteum overlying the orbital rim. The arcus marginalis will extend through the entire superior orbital rim providing a robust fixation to the eyebrow. It is extremely important that the surgeon be familiar with these fascial structures in order to perform an appropriate brow release.
The majority of the volume of the midface is provided by the malar fat pad. It lies superficial to the superficial musculoaponeurotic system and immediately below the lateral part of the infraorbital rim. It creates the convexity associated with a youthful midface. Deep to the orbicularis oculi muscle but superficial to the preperiosteal layer, inferiorly to the infraorbital rim, lies another important fat compartment—the suborbicularis oculi fat (SOOF). This adipose tissue is much smaller than the malar fat pad, but its elevation or increased volume can significantly improve results in midface rejuvenation. SOOF has been described as two distinct fat pads: a medial compartment that extends form the medial limbus to the lateral canthus and a lateral component that extends from the lateral canthus to the temporal fat pad. 19
Nerves
The facial nerve supplies all the muscles of facial expression. It travels deep to the musculature and innervates them from their undersurface. The brow elevators and depressors are all innervated by the frontal branch, with the exception of the procerus, which is innervated by the buccal branch. 20 In regard to surgical anatomy for brow and midface lifting procedures, the anatomy of the temporal branch becomes critical. This branch (or branches since there are usually more than one) exits the parotid gland and crosses the zygomatic arch approximately in its middle third, 21 and its insertion point is about 1 cm above the supraorbital rim. 22 The most commonly used surface landmark for the course of the facial nerve, known as Pitanguy’s line, 23 is a line that runs from 0.5 cm inferior to the tragus to 1.5 cm above the lateral eyebrow. However, because the eyebrow is a somewhat imprecise landmark in some patients, a more consistent approximation is the line that begins at the inferior aspect of the ear lobule and bisects another line connecting the superior border of the tragus to the lateral canthus. Nevertheless, a more accurate means to precisely identify the location of the temporal branch is to identify a series of bridging veins that travel from the TPF to the deep temporal fascia and can be seen during the endoscopic dissection. 24 One in particular, the zygomaticofacial (sentinel) vein, is larger than the others and was described as being within a 0- to 10-mm radius of the vein. 25 The senior author (VCQ) demonstrated this vein to be a perforator that corresponds to the course of the frontal branch. 24 It is usually located 1 cm from the frontozygomatic suture line 26 , 27 ( Fig. 15.2 ).

Sensory innervation of the forehead, temples, and anterior scalp is provided by the supraorbital and supratrochlear nerves, both branches of the ophthalmic division of the trigeminal nerve. The supraorbital nerve exits the skull through a notch or a foramen at the medial portion of the supraorbital rim. Generally, the notches are considered to be more frequent than the foramina. 28 , 29 Shortly after its exit, the supraorbital nerve trunk divides into a superficial (medial) and a deep (lateral) branch. The superficial division quickly splits into multiple smaller branches that pierce the frontalis muscle and run superiorly within the superficial galea. The deep division courses superolaterally between the deep galea and the periosteum, running along the temporal line. 30 The supratrochlear nerves exit the orbit medial to the supraorbital nerve through a notch above the trochlea. 31 This nerve is embedded within the medial portion of the corrugator muscle, which renders it at significant risk for injury during corrugator resection if not carefully dissected.
Aging of the Upper Two-Thirds of the Face
A lack of a better understanding of the effects of aging over the skin, subcutaneous fat, fascia, muscles of facial expression, and skeletal framework can be responsible for suboptimal outcomes of facial rejuvenation procedures. The youthful forehead is smooth, has a full eyebrow, concealing most of the upper eyelid, with only a couple of millimeters of lid show. The soft tissue pads the superior orbital rim preventing the bony orbit to be visible. The youthful midface varies in soft tissue volume but should have a triangular configuration with a gentle curved appearance overlying the zygomatic maxillary area. At the infraorbital lidcheek junction, there is a smooth transition from the thin eyelid skin to the thick cheek skin. The chronologic sequence of aging-related events starts in the third or fourth decade, when a gradual process of weakening of the structures of the face takes place resulting in the characteristics associated with the aging face syndrome.
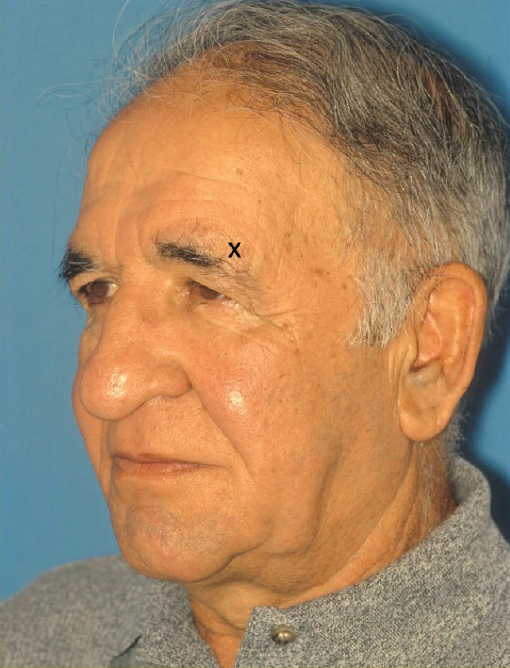
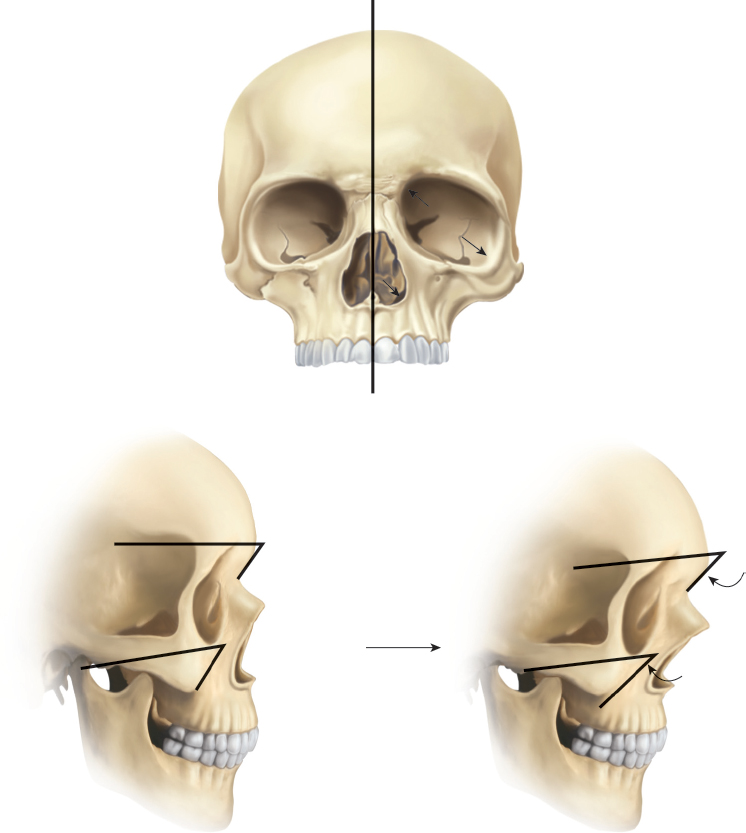
Eyebrow aging most commonly starts laterally. If this would be caused solely by the downward shifting of forehead soft tissues, one would expect the eyebrow to descend equally on the medial end. As described earlier, over the temple and the lateral brow region, the superficial temporal fascia has loose deep attachments with the only area of tenacity being its insertion on the zone of adhesion and on the orbital ligament. The unsupported lateral portion of the superficial fascia, overlying the temple, will slowly pivot on those anchor points and migrate inferomedially, contributing to lateral brow ptosis, hooding, and pseudoexcess of upper eyelid skin ( Fig. 15.3 ). There are three structures that have been implicated as facilitators of brow descent: the galeal fat pad, the preseptal fat pad, and the glide plane space. 15 , 32 The degree as to how much brow descent the patient will develop will be dictated by the muscular action on the fixation points and the facilitating structures. The lateral extension of the frontalis muscle does not surpass the zone of fixation, leaving the lateral brow unsupported.
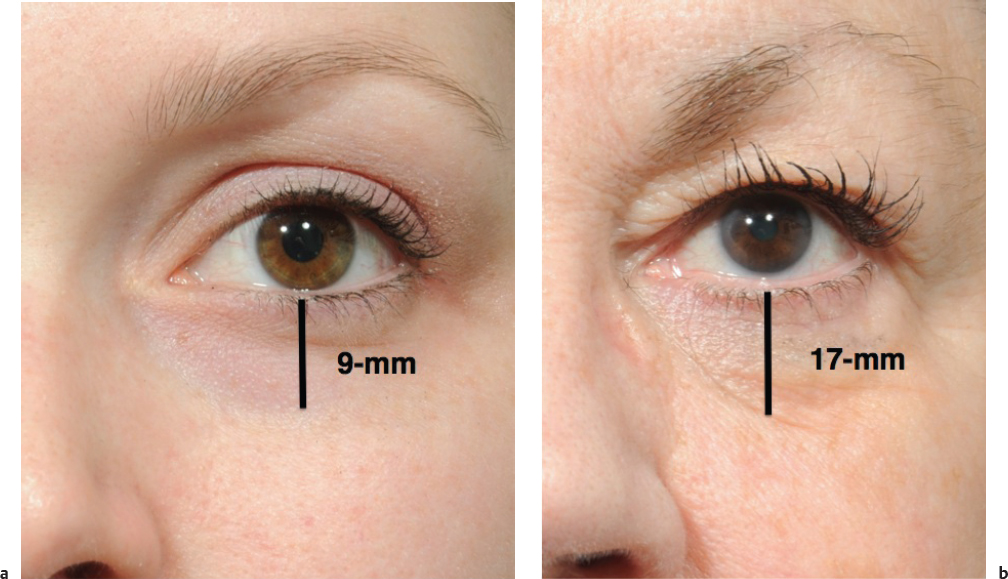
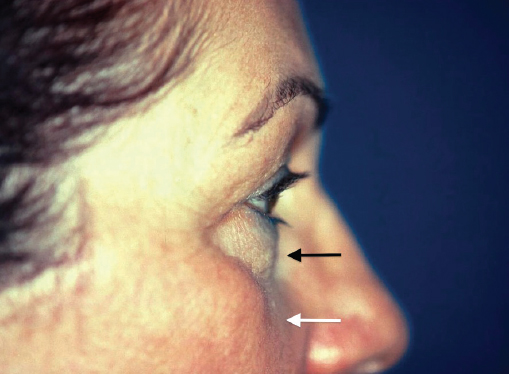
Midfacial age-related changes observed in soft tissue are perhaps the most controversial area when discussing the aging face. It has always been accepted that the aged face presented a sagging mostly secondary to gravity, but this hypothesis has been under severe scrutiny over the last decade. A compelling study by Lambros, 33 analyzing photographs from patients at different ages and superimposing those images, reported the lidcheek junction, the orbicularis wrinkles, and moles on the cheeks to be stable over time. He concluded that a vertical descent of skin was not a major component of aging in the midface and attributed the illusion of lower lid lengthening to lidcheek junction changes in shadows that are created by orbital fat protrusion with relative skin immobility. Even though most authors agree with the concept of changes in midface volume, the stability of the lidcheek junction has been contested. Clinical observations by several authors, including the senior author, document a lengthening of the lidcheek junction over time creating what has been described as “V” pattern of infraorbital aging 34 , 35 , 36 , 37 with deepening of the nasojugal groove ( Fig. 15.4 ). The protrusion of orbital fat through a weakened orbital septum will create a double convexity on this region ( Fig. 15.5 ). Aging changes in one anatomical region will have an impact on the neighboring areas. The midface ages together with the lower lid in the same manner that the upper eyelid ages with the brow. It has been described that, when comparing young and old pictures of the same person, one gets the impression of a “deflation wave” that runs perpendicular to the axis of the nasolabial fold. 33 In fact, studies have demonstrated that the aging process causes fat atrophy and fat hypertrophy in different areas. 38 Fat atrophy occurs creating depressions in the periorbital, perioral, temporal, and buccal spaces. 38 Fat hypertrophy, on the other hand, is seen mostly in the submental region, but also in the jowl and nasolabial and labiomental fold regions. The idea that the fat descends independently of skin is also very unlikely. These concepts imply that the face ages threedimensionally, with changes in position and volume. Fig. 15.6 illustrates a patient with midface aging.

The final piece to the forehead and midface aging puzzle comes from the changes seen in the craniofacial skeleton. The bony remodeling that occurs over the years has been increasingly recognized as one of the key contributors to facial aging. 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 There is a clockwise rotation of the maxilla in relation to the cranium along with a relative contraction of the bony skeleton and the changes in the glabella, orbit, pyriform, and maxilla seen with the passage of time, explain the loss of skeletal support and its effect on the overlying soft tissues. It was postulated that the decrease in the maxillary angle would create a lack of support for the malar fat pad, leading to its descent. 40 Another important area of consideration when studying forehead and midface aging is related to the changes that occur in the orbit. The lidcheek junction is a key portion on midface aging and rejuvenation strategies. The orbital width and area have been demonstrated to increase, 40 , 41 , 42 with the infraorbital rim having some degree of resorption, bowing preferentially inferolaterally in females, while in males, the entire inferior orbital rim recedes. This creates a negative vector, which explains the associated soft tissue changes in this area. The superior orbital rim has been demonstrated to have superomedial bone resorption in both males and females. 40 , 41 , 42 , 43 Fig. 15.7 illustrates the skeletal changes that occur with aging. Another skeletal change significant for midfacial aging is related to bone resorption in the pyriform aperture. Even though the pyriform aperture angle remains stable, there is a lateral resorption of bone, with widening of this area and subsequent loss of support for the soft tissues that will result in deepening of the nasolabial folds. 39 , 40
The changes in curvatures of the aged face are more likely to be caused by a combination of all these factors: changes in the volume of fat pads, increased laxity of retaining ligaments of the face, and change in the position of these ligaments secondary to skeletal changes. With that in mind, when rejuvenating the face, a simple elevation of the fat compartments through lifting procedures may not lead to an appealing result if the facial fat compartments are atrophic or if the bone structure is weak. In that perspective, volume replacement with soft tissue fillers or autologous fat to restore volume loss and create a more curvilinear contour to the face can complement lifting procedures ( Fig. 15.8 ). In addition, aging is not a linear and uniform process. Every patient will age differently, a point that can be well illustrated in the upper third of the face. Brow descent is not that significant in many cases, and certainly, in some patients, it does not descend as much as most forehead lift procedures tend to raise them. There are a few reports in the literature that contradict the belief that the eyebrows uniformly descend over time, demonstrating that they remain relatively stable or even rise with aging. 33 , 47 , 48 This data is by no means dogmatic; however, it suggests that aging is a heterogeneous process. It should make the surgeon aware of individual nuances, and he or she should avoid a cookie-cutter approach to brow and midface lifting procedures.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








