Aetiology and Pathogenesis.
In vitiligo there is a variable pattern of loss of melanocytes from the epidermis and follicular reservoir; this is most usually chronic and progressive, with periods of spontaneous remission. However, the mechanism of melanocyte loss has never been clearly understood, and vitiligo is probably a multifactorial disorder. Also, the pathogenesis differs between segmental and non-segmental vitiligo (NSV).
Genetic Susceptibility
Most cases occur sporadically but about 15–20% of patients have one or more affected first-degree relatives. Familial aggregation of NSV follows a non-Mendelian pattern suggesting complex polygenic multifactorial inheritance. The link of non-segmental vitiligo with various genes already associated with autoimmune disease has been reported, including CTLA4, PTPN22, MBL2 and IL10 [2,3], and also recently tyrosinase (TYR) [4]. Other candidate genes have been reported but need to be confirmed (GCH1, CAT, COMT, ACE, GPX1, AIRE). Targeted family-based association analysis recently proposed NALP1 as a susceptibility gene for vitiligo associated with other autoimmune diseases [5].
Similar to other common chronic disorders, vitiligo may represent an interaction between inherited and environmental factors [6].
Melanocyte Loss
Melanocyte loss could result from a cell-mediated immune response (cellular immunity), abnormal humoral response (autoantibodies), apoptosis [7] or detachment [8]. Nevertheless, the initiating events and the melanocytic targets are still unknown. A link between oxidative stress and immune system activation is possible. The production and release of hsp70 by melanocytes may activate an immune response [9].
Other Involved Cells
Keratinocytes appear to be involved in vitiligo and have defective intracellular signal transduction of the tumour necrosis factor-α (TNF-α)-activated pathway leading to limited survival and subsequent loss of production of specific melanocyte growth factors. The stem-cell factor, c-Kit axis, is most important in this setting [10]. A more generalized biochemical or biological defect could be responsible for vitiligo as illustrated by abnormalities of peripheral blood mononuclear cells (metabolic deregulations and oxidative stress) [11].
Segmental Vitiligo
The pathophysiology is presumed to be different for segmental vitiligo. The distribution of segmental vitiligo in at least a subset of patients suggests a pattern usually associated with cutaneous mosaicism.
Segmental vitiligo can be associated with non-segmental vitiligo. It indicates a continuum between the two forms with shared predisposing genetic factors, including genes operating specifically in the skin. It also suggests a mechanism of loss of heterozygosity for a dominant gene controlling part of the cutaneous phenotype [12].
Pathology.
The diagnosis of vitiligo is usually a straightforward clinical diagnosis and a skin biopsy is not required. Histologically, melanocytes are completely absent in established lesions of vitiligo [13–15]. Histological stains can be used to confirm the diagnosis, such as dopa stain for tyrosinase (a specific enzyme of melanocytes) or the Fontana–Masson silver stain for melanin. If necessary, immunohistochemical stains using antibodies to antigens on cells of neural crest derivation, or specific melanocyte antibodies such as anti-tyrosinase can also confirm the absence of melanocytes [16].
In contrast, melanocytes are not absent in the sections from early lesions, but exhibit various cellular abnormalities including vacuolization, presence of dilated endoplasmic reticulum and granular deposits [17].
Others abnormalities have also been described in vitiligo lesions such as alterations in keratinocytes and Langerhans cells, epidermal vacuolization, thickening of the basement membrane, macrophages in the dermis and neural alteration [18,19].
During repigmentation, especially when UV-induced, there is an influx of cells from the follicular reservoir, where melanocytes reside [20,21]. This is confirmed by response to treatment: repigmentation is first visible principally around follicular orifices, and depigmented lesions without hair follicules (glabrous skin) do not respond to treatment [22].
Clinical Features.
Clinical features are documented in several series on childhood vitiligo [23–30].
Prevalence and Age of Onset
Many studies report that most cases of vitiligo are acquired early in life, but the exact prevalence in the paediatric age group is unknown. Howitz et al. in Denmark found that approximately 25% of patients noted the onset of vitiligo before the age of 10 years [31]. The mean age of onset varied among different studies from 4 to 8 years. Vitiligo can occur in infants as young as 3 months. There are reports of congenital vitiligo, although whether these reports truly illustrate piebaldism or ‘congenital vitiligo’ is unclear [32]. In Caucasians, often the vitiligo only becomes evident after a holiday, when exposure of the skin to the sun reveals the depigmented areas of skin, highlighted by the unaffected skin, which tans normally.
Gender
In most reported paediatric series the majority of cases were in girls, but this finding differs from population-based studies, which do not confirm a female sex predominance.
Race
All races can be affected. The prevalence probably varies according to geographic origin and seems to be higher in India than in other countries.
Morphology
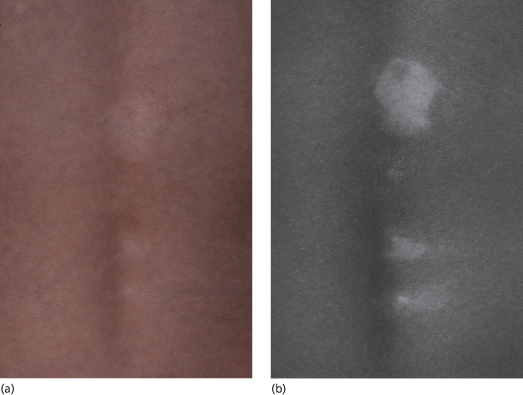
The depigmented lesions are, as the name suggests, completely devoid of pigment and appear as ivory white areas of skin (Figs 105.2 to 105.4). Patches of vitiligo are made more visible by tanning of the surrounding skin or in dark skin. The use of the Wood’s lamp is useful to delineate areas of involvement in fair-skinned children (Fig. 105.5).
Fig. 105.3 Vitiligo on the lower legs and feet: ivory white symmetrical areas on the knees, ankles and feet.
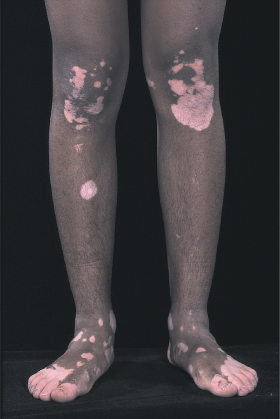
Early or advancing lesions of vitiligo may be partially depigmented and have a freckled appearance or multishaded hue. In dark-skinned individuals this is termed trichrome vitiligo. Typical lesions are several millimetres to many centimetres in diameter with an oval or geographic pattern. A hyperpigmented border may be seen surrounding the depigmented lesions. In a few patients, an inflammatory border (oedematous, pruritic and erythematous) may be visible.
Psychological Effects of Vitiligo
There is a lack of specific studies on the psychological effects of vitiligo. Nevertheless, although vitiligo is not a life-threatening disease, it can be a life-altering disease. Children are probably affected differently, depending on the location, extent and course of the disease, their age, the colour of their skin, their individual capacities and their social environment.
Classification and Distribution.
Depigmented patches of vitiligo can occur anywhere on the body and no area is necessarily spared. The most common involved site of vitiligo is the head.
In non-segmental vitiligo, lesions are characteristically distributed in a remarkably symmetrical pattern involving both sides of the body. The most common location is the face, especially around the eyes, and neck, followed by the lower limbs, trunk and upper limbs. Involvement of the perineum and in particular the perianal skin, is common in children and can herald the onset of vitiligo (Fig. 105.6). Examination of the hands and feet with a Wood’s lamp confirms that these areas are commonly involved, even in those with type 1 or 2 skin.
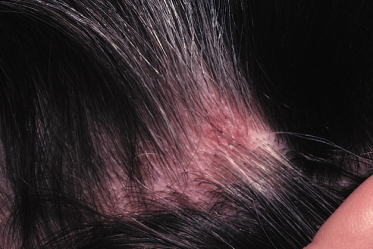
The skin and hair follicles on the scalp can also be involved, leading to poliosis (Fig. 105.7). In the literature, the prevalence was found to be between 12.3% and 19.3%. Premature greying of the hair is sometimes observed; Jaisankar et al. noted this finding in 4.4% of children [29]. There are a few individuals who develop totally white hair of the scalp, eyebrows and eyelashes.
The area rarely recognized to be affected by vitiligo is the oral cavity. The lips, buccal mucosa and gingiva can be involved but the incidence of involvement seems to be lower in children than in adults. In the literature, the involvement of the mucosa varies from 0% to 13.3%.
Extension
The extent of involvement varies among patients. Handa and Dogra demonstrated that 96.4% of children have less than 20% of the body involved, and 89.7% have less than 5% of the body area involved [27].
Koebner Phenomenon
In clinical pratice, we often observe that knees, elbows, shins, arms and hands are often the sites of initial involvement in children. Children are known to suffer from numerous scrapes and scratches as they play or explore their environment. Only a few studies have recorded the presence of the Koebner phenomenon in children with vitiligo. Handa and Dogra found evidence of koebnerization in 11.3% of children [27].
Associated Skin Conditions
Vitiligo can affect children with a history of atopic dermatitis, but no study has clearly demonstrated this association. In this situation, it is necessary to distinguish the depigmented areas of vitiligo from postinflammatory hypopigmentation or depigmentation, secondary to eczema.
Halo naevi can be observed in children with vitiligo and can precede the onset of generalized vitiligo. Nevertheless, in clinical practice, we often see children with halo naevi who do not go on to develop vitiligo. A precise comparison with the general paediatric population is impossible since the prevalence of halo naevi is not well known. Nevertheless, Prcic et al. [26] found that there are more halo naevi in children with vitiligo, compared to children without vitiligo (34% vs 3.3%). In the literature, the prevalence of halo naevi in children with vitiligo has varied among published studies (2.5–34%). It is also not entirely clear if the prevalence of halo naevi in childhood vitiligo is different from that in adult vitiligo. Prcic et al. reported in two series [25,26] that halo naevi were more frequent in childhood vitiligo compared to adult vitiligo. In contrast, Cho [24] found more halo naevi in a group of adult vitiligo cases compared to childhood vitiligo.
Associated Autoimmune Diseases
Children suffering from vitiligo are generally healthy, but other autoimmune diseases can be associated. The most common reported autoimmune disease is thyroiditis. The prevalence of thyroid dysfunction in childhood vitiligo was found to vary among different studies (0% to 25%) [26,30,33–36]. Some authors have suggested that thyroid dysfunction increases with age. Nevertheless, Kakourou et al. found no association between thyroid dysfunction and the following parameters: chronological age, age of onset, mean duration, clinical type of vitiligo, family history of autoimmunity/thyroid disorder or sex [34]. In the series by Mazerrreuw-Hautier et al., of the 10 affected children, all but one patient were girls [30]. Depending on the study, it seems now established that thyroid anomalies are more frequent or only observed in non-segmental vitiligo.
The other autoimmune diseases reported in children with vitiligo include: alopecia areata, diabetes mellitus, Addison’s disease and autoimmune polyglandular syndrome. The prevalence of these other diseases seems to be very low (1.3 to 7.6%) [24,27,28].
Antinuclear antibodies can be found in children with vitiligo. This probably represents the general autoimmune status of the child with vitiligo. Halder [23] found them in 4.8% of children, whereas Cho [24] and Prcic [26] did not find any positive children.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree