10 Extensor Indicis Proprius Tendon Transfer for Rupture of the Extensor Pollicis Longus Tendon
Abstract
Transfer of the extensor indicis proprius (EIP) to extensor pollicis longus (EPL) tendon is a reliable procedure to restore thumb extension for a ruptured or otherwise irreparable EPL tendon. The EPL can rupture from attritional wear after distal radius fracture or due to osteophytes and chronic inflammation from wrist arthritis. Tendon transfer principles that are applied include an expendable donor (EIP), synergistic function, similar excursion and power, straight line of pull, and one transfer for one function—thumb extension. The procedure can be performed under wide-awake local anesthesia with no tourniquet (WALANT) to ensure proper tendon tension, glide, and repair strength. Proper tensioning of the transfer is critical, with slight over-tensioning preferable to provide optimal motion and strength. A Pulvertaft or similar tendon weave should provide adequate repair strength to start therapy early in the postoperative period. As with all tendon transfers, some loss of thumb extension strength is expected but otherwise a good range of motion, coordination, and function are the norm. There usually is a loss of independent index finger extension, and diminished index finger extension strength is expected, which is well tolerated from a functional standpoint.
10.1 Description
Tendon transfer of extensor indicis proprius (EIP) to extensor pollicis longus (EPL) for ruptured or lacerated and irreparable EPL tendon at the wrist level.
10.2 Key Principles
Tendon transfer basic principles, as applied to EIP to EPL transfer:
EIP is an expendable donor of similar excursion and power
This transfer performs only one function: thumb extension
Synergistic transfer
Though a straight line of pull is recommended, this procedure (as described later) provides a similar line of pull to the EPL tendon that changes course at Lister tubercle
Expect one MRC grade of motor strength loss
Proper tensioning of the tendon transfer is critical for an optimally functioning thumb
A strong repair allows immediate initiation of therapy to accelerate rehabilitation and decrease risk of tendon adhesions (Giessler et al; Germann et al 2008).
Occupations therapy is helpful for muscle re-education/cortical remapping.
10.3 Expectations
The surgery should recreate the ability to extend the thumb out of the palm and posterior to the plane of the hand, to facilitate pinch and grasp. As with any tendon transfer, a slight decrease in strength (four out of five MRC grade) is expected, but otherwise, a good range of motion, coordination, and function are the norm (Lemmen et al 1999; Meads and Bogoch 2004). Additionally, there will be loss of index finger independent extension and some loss of index finger extension strength, which are well tolerated (Magnussen et al 1990).
10.4 Indications
EPL tendon rupture is typically a consequence of distal radius fracture or wrist arthritis that places the rupture site at the level of the carpus. Ruptures or lacerations distal to this level may not leave enough EPL tendon to connect the EIP transfer. In general, EIP to EPL tendon transfer is indicated if EPL primary repair is not possible due to attritional rupture (poor tendon quality), segmental tendon loss (unable to bridge gap), or an old injury where the EPL muscle and tendon unit have irreversibly retracted.
10.5 Contraindications
Absent or non-function EIP or extensor digitorum communis tendon to index finger (EDCI)
Poor soft tissue coverage
Very distal EPL rupture such that EIP is not long enough for transfer
Joint contracture that would limit motion
10.6 Special Considerations
Assure that the patient has full passive thumb range of motion and functioning EDCI and EIP tendons to permit the sacrifice of the EIP tendon. To verify EIP function, the patient should demonstrate independent index finger extension with the other fingers clenched in a tight fist. The EDCI tendon will visibly buckle with this maneuver.
10.7 Special Instructions, Positioning, Anesthesia
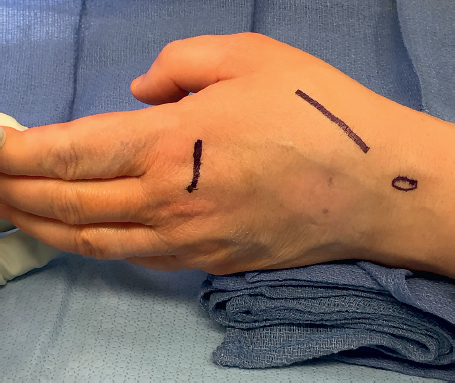
The procedure is best performed with the patient awake to assure proper tendon tensioning, repair strength, and tendon glide. Wide-awake local anesthesia with no tourniquet (WA-LANT) is preferred to avoid the influence of ischemia and muscle constriction from the tourniquet on the patient’s ability to move the thumb. The patient is positioned supine with their arm on a hand table. A tendon passer can simplify subcutaneous passage of the tendon and a “pig sticker” is used to perform the tendon weave.
10.8 Tips, Pearls, and Lessons Learned
The EIP and the other accessory extensor tendon, the small finger extensor digiti quinti (EDQ) are always more ulnar at the metacarpophalangeal (MP) joint. An easy way to remember this fact is that with the index and small fingers only extended, the hand forms the shape of a “U” for ulnar.
It is helpful to thoroughly release any EIP soft tissue attachments over the dorsum of the hand before dividing it distally.
It is important to assure that the EIP tendon has a clear line of pull from the exit of the fourth dorsal extensor compartment to the EPL without intervening soft tissue which could bind tendon glide.
Setting the proper transfer tension is critical. A good rule of thumb (literally) is to tension the tendons so that the thumb interphalangeal (IP) joint sits in full extension with the wrist in neutral (Low et al 2001). However, the final decision on proper tension should be based on the patient’s active range of motion at surgery. With the wrist in the functional position of 30 degrees of extension, the patient should be able to actively fully extend the thumb and oppose to at least the mid-portion of the small finger (Lalonde 2014).
You will have to ask the patient to extend the index finger (EIP), not the thumb, to test thumb extension.
In general, it is better to err on the side of overtightening the transfer since the tension tends to lessen slightly over the first few months after surgery as the patient “works out the slack in the system” (Lee et al 2015; Jung et al 2014).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








