Abstract
Anatomic considerations are a critical aspect of preoperative planning for all surgical procedures; however, nowhere is it more important than in the hand, wrist, and forearm. The relatively superficial location of critical structures including tendons, nerves, and vessels cannot be underestimated or overlooked. This chapter will review anatomy, incisional considerations, and specific approaches for the hand, wrist, and forearm.
1 Anatomy and Approaches
I. Hand
A. Anatomic Compartments
Thenar: Median, recurrent motor branch nerve
Abductor pollicis brevis
Flexor pollicis brevis (deep fibers innervated by deep branch of ulnar nerve)
Opponens pollicis
Adductor: Ulnar nerve
Adductor pollicis
Hypothenar: Ulnar nerve
Abductor digiti minimi
Flexor digiti minimi
Opponens digiti minimi
Interosseous: Ulnar nerve
Dorsal interossei (four)
Volar interossei (three)
Lumbricals: 1st and 2nd median nerves, 3rd and 4th deep branch of ulnar nerve
1st and 2nd are unipennate
3rd and 4th are bipennate
These muscles originate on the flexor digitorum profundus (FDP) tendons
B. Nerves
Median
Recurrent motor branch
Palmar cutaneous branch (branches off the main trunk of the nerve proximal to the carpal tunnel but innervates the palm)
Ulnar
Ulnar motor and ulnar sensory split within Guyon’s canal
C. Vasculature
Superficial palmar arch—continuation of ulnar artery
Common digital arteries to index, middle, ring, and small fingers arise from superficial arch
Split into proper palmar digital arteries, supplying ulnar side of index finger as well as ulnar and radial arteries to middle, ring, and small fingers
Deep palmar arch—continuation of radial artery
Princeps pollicis branch supplying thumb
Radial-side digital artery of index finger
D. Incisional Considerations
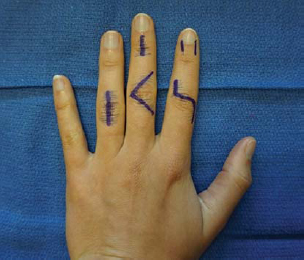
Volar: Avoid deep creases on digits, cross creases at approximately 90-degree angle (Bruner) with the incision running diagonally across the skin in between creases to avoid contracture.
Incisions less than 90 degrees may cause skin necrosis of the corner.
Avoid travelling too dorsal/lateral while creating the angle to avoid crossing the neurovascular bundles that could be damaged when elevating the flap.
Dorsal: Often can use smaller incisions due to mobile nature of skin, can be vertical, horizontal, or curved with appropriate skin bridges.
Fingers can be approached dorsally, volarly, or midaxially.
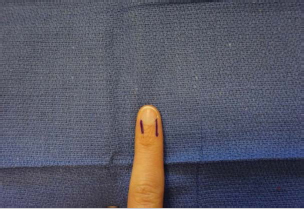
If midaxial, it is best to place the incision at the junction of the glabrous and non-glabrous skin.
E. Approaches
1. Nail Bed
The nail bed is exposed by bluntly removing the nail plate from the underlying sterile matrix with a noncutting instrument such as a freer.
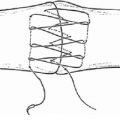
Longitudinal incisions in the eponychial fold can be made at the proximal corners radially or ulnarly to expose the proximal nail bed and germinal matrix (► Fig. 1.1).
2. Interphalangeal Joints
Dorsal: A variety of incisions can be used, including straight, curved, S-type, H-type, and chevron (► Fig. 1.2).
At the distal interphalangeal joint, the germinal matrix is 1 mm distal to the insertion of the extensor tendon, and both are relatively superficial under the skin.
The extensor mechanism dictates the approach at the proximal interphalangeal joint. Care should be taken to protect the central slip as it inserts onto the middle phalanx, and the lateral bands.
Dorsal approach between the central slip and the lateral bands.
Lateral exposure to the joint achieved by freeing the lateral bands and retracting them dorsally.
Extensile approach by incising the lateral bands with subsequent repair.
The entire extensor mechanism can be removed via the Chamay approach of a distally based V-shaped flap.
Volar: Zig-zag (aka Bruner) incision through skin to expose the flexor tendon sheath (► Fig. 1.3).
The pulley overlying the joint is incised longitudinally.
Do not incise A2 or A4 pulley whenever possible.
The flexor tendons are retracted radially or ulnarly.
For more exposure, the split in the superficialis tendon may be carried proximally to allow for more retraction of the profundus tendon.
The collateral ligament attachments to the volar plate are incised and the volar plate is mobilized to expose bone.
Joint hyperextension exposes articular surfaces.
Midlateral: Longitudinal incision along midlateral aspect of finger (use the most dorsal aspect of the proximal or distal phalangeal creases as landmarks).
The fat overlying the interphalangeal joints is thin; use superficial dissection to avoid incising the joint itself unintentionally.
Dissection is carried down the midline of the finger with a slight volar angle.
Neurovascular bundle is contained in the volar flap.
The flaps can be elevated to expose volarly or dorsally.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree