Veins at Other Sites
 GENERAL
GENERAL
As treatment of leg veins has become so successful and commonly performed, enlarged veins at sites other than the legs are becoming more of a concern for patients. Photoaged hands with ropey blue veins contrast with faces rejuvenated by lasers and injectables. Enlarged veins on the central chest are cosmetically disturbing.
Décolletage is the term used to describe the upper part of a woman’s torso the neck, shoulders, upper back, and chest. Revealing fashions motivate female patients to seek cosmetic improvement of enlarged veins, wrinkled skin, and blotchy pigmentation. After breast implants, veins can become enlarged on the central chest with obstruction of venous return from the skin due to physical pressure of the implants against skin and muscle. After medical etiologies such as portal vein hypertension or right-sided heart failure are not suspected, the cosmetic appearance may be treated. This chapter deals with the treatment of enlarged veins of the chest and hands.
Special Consent
Generally, non-leg sclerotherapy sites have a lower incidence of side effects, specially telangiectatic matting and hyperpigmentation. Some physicians may use a site-specific consent. Matting or hemosiderin staining may be more distressing to the patient when they occur at sites less covered than the legs; so, patients should be aware of the slight risks before such veins are treated. Care should be taken to ensure that the patient’s expectations are appropriate, and particular note should be made in the chart that the patient has been informed of the possibility of cosmetic complications. Patients should sign a consent form acknowledging this discussion before beginning the treatment. The sclerotherapy for leg veins consent can be used or modified for the specific area.
Limit Treatment to Cosmetic Regions
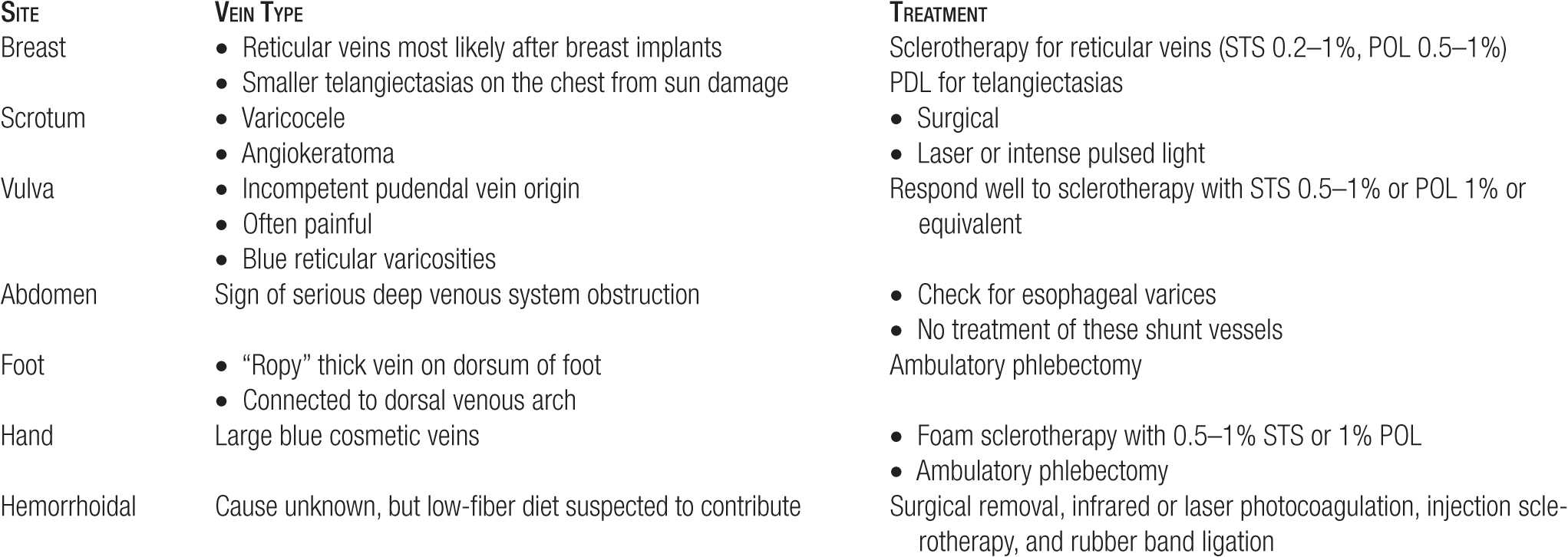
Because vessels in locations other than the lower extremities do not produce significant disturbance of venous circulation nor are they typically the result of reflux, treatment should be limited to the specific vessels that are of immediate cosmetic concern. Ideally, one can document the appearance of the vessels in pretreatment photographs. General principles are summarized in Table 16-1.
TABLE 16-1
Treatment Options for Veins Other than Face or Legs
Anti-inflammatories
A mild local inflammatory response after sclerotherapy is common. To reduce this response when visible or sensitive body areas are treated, a nonsteroidal anti-inflammatory agent can be prescribed for three days after each treatment session. In addition, the use of a medium-potency topical steroid may be applied twice a day for two to three days post-treatment including immediately after the treatment. This may also be used for the legs. The most effective way to reduce an inflammatory response is to reduce the concentration of sclerosing agents to the minimal concentration that will sclerose the targeted vessel. A detergent agent is preferred for nonfacial treatment. Avoidance of hypertonic saline is highly recommended.
 BREAST
BREAST
Evaluation
Most prominent veins on or around the breast are typically caused by breast implants. Other medical causes should be considered before treatment, such as right-sided heart failure. The history of breast implants particularly in thin, healthy women typically results in very little further medical evaluation. Rarely, posttraumatic vessels may appear on the breast shortly after an isolated incident of trauma. These vessels can be treated easily, provided that the trauma was remote and that the vessels have not been undergoing any recent change.
Some patients have familial (“essential”) telangiectasia that are present on many areas of the body, including the breasts. These vessels can be treated easily and present no special difficulty. These are usually exacerbated by sunlight exposure. Smaller telangiectasias on the chest may best be treated by lasers as discussed in another chapter. Sclerotherapy is the recommended treatment when reticular blue veins are targeted for cosmetic treatment.
As stated, postoperative dilated vessels are most often noticed after breast implants (Figure 16-1A). It is believed that these vessels occur centrally due to slightly blocked venous drainage on the lower half of the chest. Although these cosmetic vessels may be treated, treatment should not be undertaken for at least six months after the implants are in place as new vessels may appear. Special care is required to avoid puncturing an implant that may have migrated or extruded into an unexpectedly superficial location. Ultrasound may be used to confirm the position of the implant. The patient must also be warned that the vessels treated centrally may be replaced by veins on the lateral portions of the chest. New vessels will be less cosmetically visible when lateral to the décolletage area of the central chest.

![]() FIGURE 16-1 Reticular veins prominent on the chest after breast implants. A. Appearance before treatment. B. Appearance after one treatment with 0.2 percent STS—1 cc total.
FIGURE 16-1 Reticular veins prominent on the chest after breast implants. A. Appearance before treatment. B. Appearance after one treatment with 0.2 percent STS—1 cc total.
Bypass vessels may serve to direct venous outflow around an obstruction in the axilla or the neck. These are usually identified by their location and orientation, as they extend well away from the breast toward the neck, shoulder, or axilla. These vessels should not be treated, and patients in whom this bypass syndrome is suspected should be evaluated for prior upper extremity deep vein thrombosis (DVT), for other causes of outlet obstruction such as superior vena cava syndrome, and for hypercoagulable states.
Some patients are concerned about normal vessels that are particularly prominent because of variant anatomy or because of translucent skin. Prominent normal vessels should be treated only if there is a pressing reason, cosmetic or otherwise, for doing so. Patients must be specially warned of the risks of resistance to treatment in normal vessels. Also, patients with translucent skin will always be able to see superficial veins more easily as they become more apparent with age. Most Caucasian patients’ vessels become more visible as skin ages and becomes atrophic.
Treatment
At the initial treatment session, a test injection can be limited to one vein. Treatment may begin at the inferior inner quadrant of the breast and other areas normally covered by a brassiere so that if pigmentation occurs, it will be hidden. We recommend that the décolletage is treated only after good results have been seen in less visible areas.
Because breast veins often drain directly into small-caliber deep vessels, the concentration and volume of sclerosant should be kept to a minimum. Typically, the starting sclerosing concentration is 0.1–0.2 percent sodium tetradecyl sulfate (STS) foamed or 0.25-0.5 percent polidocanol (POL) foamed. A typical response is seen in Figure 16-1B. High grades of compression are not possible in the breast area, but a tight-fitting sport brassiere is recommended for the first 48 hr in order to minimize inflammation as much as possible. Patients are advised to sleep elevated with two pillows for several days. Bruising is common and will typically clear two to three times faster than on the legs, resolving in a matter of days.
 HANDS
HANDS
Evaluation
Bulging hand veins rarely represent true venous pathology. Abnormally large hand veins that develop suddenly can be a sign of upper extremity venous outflow obstruction, but in most cases, these large veins are merely a cosmetic nuisance. They may appear as age causes fat atrophy accompanied by loss of subcutaneous tissues around and below the veins (Figure 16-2A). In addition, apotosis or programmed cell death of smooth muscle cells in vein walls contributes to the stretching and enlargement as time progresses.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



