11 Facial paralysis
Synopsis
 Assess clinical problem: functional, psychosocial, and aesthetic.
Assess clinical problem: functional, psychosocial, and aesthetic.
 Understand the etiology and natural history of disease processes associated with facial paralysis.
Understand the etiology and natural history of disease processes associated with facial paralysis.
 Knowledge of anatomy is imperative for optimizing results.
Knowledge of anatomy is imperative for optimizing results.
 Formulate realistic, attainable, and practical management plan.
Formulate realistic, attainable, and practical management plan.
 Surgical management is multifocal and must be individualized for each patient.
Surgical management is multifocal and must be individualized for each patient.
Basic science
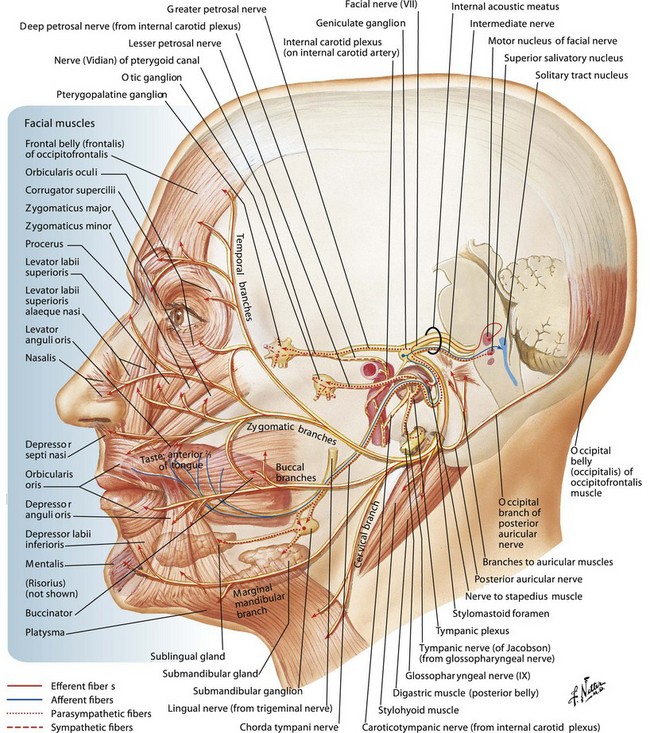
The facial nerve
The extratemporal portion of the seventh cranial nerve begins at the stylomastoid foramen. It is in a deep position below the earlobe but becomes more superficial before it passes between the superficial and deep portions of the parotid gland. Here it divides into two main trunks which then further divide within the substance of the gland. In a series of anatomic dissections, Davis et al.1 demonstrated several branching patterns of the facial nerve. Traditionally, it is taught that this results in five divisions of the facial nerve: frontotemporal, zygomatic, buccal, marginal mandibular, and cervical. In practice, however, there is no distinct separation between the zygomatic and buccal branches either in their location or in the muscles they innervate.
On leaving the parotid, the facial nerve may have 8–15 branches making up the five divisions. Distally, there is further arborization and interconnection of these branches (Fig. 11.1). The net effect is a great deal of functional overlap between the branches. For example, a single zygomaticobuccal branch may supply innervation to the orbicularis oculi as well as to the orbicularis oris.
The temporal division consists of three or four branches2 that run obliquely along the undersurface of the temporoparietal fascia after crossing the zygomatriarch in a location 3–5 cm from the lateral orbital margin. The lower branches run along the undersurface of the superior portion of the orbicularis oculi for 3–4 mm before entering the muscle to innervate it.3 According to Ishikawa,2 the upper two branches entering the frontalis muscle at the level of the supraorbital ridge are usually located up to 3 cm above the lateral canthus. The nerves usually lie approximately 1.6 cm inferior to the frontal branch of the superficial temporal artery. Because there is relatively little adipose tissue at the lateral border of the frontalis, those nerves are virtually subcutaneous and susceptible to injury.
The marginal mandibular division consists of one to three branches4 whose course begins up to 2 cm below the ramus of the mandible and arcs upward to cross the mandible halfway between the angle and mental protuberance. It has been well documented2,3,5 that these branches lie on the deep surface of the platysma and cross superficial to the facial vessels approximately 3.5 cm from the parotid edge. Nelson and Gingrass5 described separate branches to the depressor angularis, depressor labii inferioris, and mentalis, and a variable superior ramus supplying the upper platysma and lower orbicularis oris.
The cervical division consists of one branch that leaves the parotid well below the angle of the mandible and runs on the deep surface of the platysma, which it innervates by entering the muscle at the junction of its cranial and middle thirds. This point of entry is 2 or 3 cm caudal to the platysma muscle branch of the facial vessel.6
Facial musculature
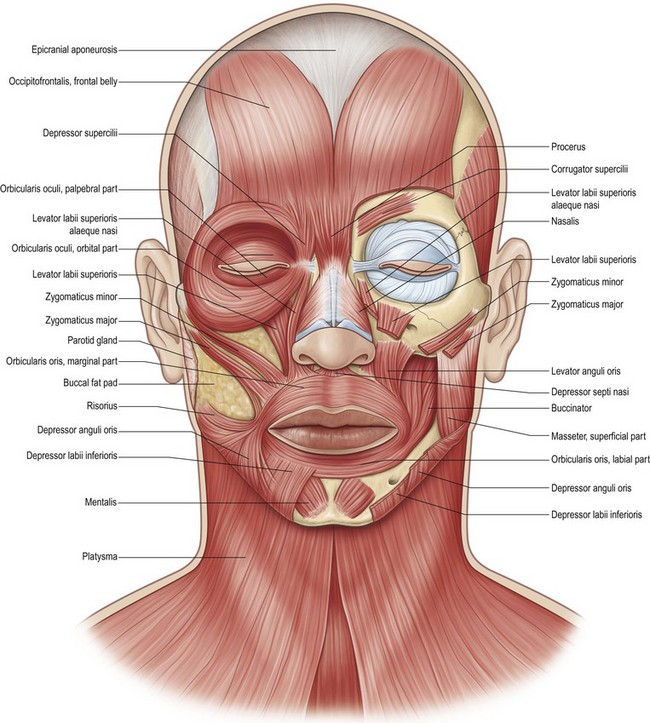
Facial musculature consists of 17 paired muscles and one unpaired sphincter muscle, the orbicularis oris (Fig. 11.2). The subtle movements that convey facial expression require coordination between all of these muscles.
Freilinger et al.3 have demonstrated that the mimetic muscles are arranged in four layers. The depressor anguli oris, part of the zygomaticus minor, and the orbicularis oculi are the most superficial, whereas the buccinators, mentalis, and levator anguli oris make up the deepest layer. Except for the three deep muscles, all other facial muscles receive innervation from nerves entering their deep surfaces.
The frontalis muscle is a bilateral broad sheet-like muscle 5–6 cm in width and 1 mm thick.4 The muscle takes origin from the galea aponeurotica at various levels near the coronal suture and inserts on to the superciliary ridge of the frontal bone and into fibers of the orbicularis oculi, procerus, and corrugators supercilii. It is firmly adherent to the skin through multiple fibrous septa but glides over the underlying periosteum. The two muscles fuse in the midline caudally; however, this is often a fibrous junction. Not only is the frontalis essential to elevate the brow, but also its tone at rest keeps the brow from descending. This tone is lost in the patient with facial paralysis, which allows the brow to fall and potentially obscure upward gaze.
The orbicularis oculi muscle acts as a sphincter to close the eyelids. Upper eyelid opening is performed by the levator palpebrae superioris muscle innervated by the third cranial nerve and the Müller muscle, which is a smooth fiber muscle innervated by the sympathetic nervous system. The orbicularis oculi muscle is one continuous muscle but has three subdivisions: pretarsal, covering the tarsal plate; preseptal portions, overlying the orbital septum; and the orbital, forming a ring over the orbital margin. The pretarsal and preseptal portions function together when a patient blinks, whereas the orbital portion is recruited during forceful eye closure and to lower the eyebrows. According to Jelks and Jelks,7 the preseptal portion of the orbicularis oculi is under voluntary control, whereas the pretarsal provides reflex movement.
The pretarsal orbicularis oculi overlies the tarsal plate of the upper and lower eyelids. The tarsal plates are thin, elongated plates of connective tissue that support the eyelids. The superior tarsal plate is 8–10 mm in vertical height at its center but tapers medially and laterally, whereas the inferior tarsal plate is 3.8–4.5 mm in vertical height. The skin overlying the pretarsal orbicularis is the thinnest in the body and is adherent to the muscle over the tarsal plate. The skin is more lax and mobile over the preseptal and orbital regions. The eyelid skin also becomes thicker over the orbital part of the muscle. The preseptal orbicularis provides support to the orbital septa and is more mobile except at the medial and lateral canthi, where the muscle is firmly attached to the skin. The orbital portion of the orbicularis oculi extends in a wide circular fashion around the orbit. It originates medially from the superomedial orbital margin, the maxillary process of the frontal bone, the medial canthal tendon, the frontal process of the maxilla, and the inferomedial margin of the orbit. In the upper eyelid, the fibers sweep upward into the forehead and cover the frontalis and corrugators supercilii muscles; the fibers continue laterally to be superficial to the temporalis fascia.8,9 Because this muscle is one of the superficial group of mimetic muscles,10 in the lower eyelid the orbital portion lies over the origins of the zygomaticus major, levator labii superioris, levator labii superioris alaeque nasi, and part of the origin of the masseter muscle. There are multiple motor nerve branches that supply the upper and lower portions of the orbicularis oculi, and these enter the muscle just medial to its lateral edge.
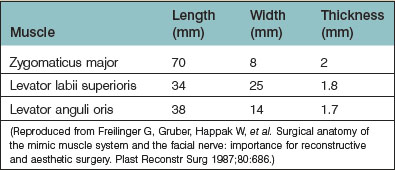
Freilinger et al.3 extensively studied the three major lip elevators, zygomaticus major, levator labii superioris, and levator anguli oris, and provided data on their length, width, and thickness (Table 11.1).
The orbicularis oris is a complex muscle that functions as far more than a sphincter of the mouth; it serves to pucker and purse the lips. It makes up the bulk of the lip, as skin overlies it superficially and mucous membrane is attached on its deep surface. Philtral columns are formed by the insertion of the orbicularis, and a portion of levator labii superioris, into the skin.11 The levator labii superioris fibers reach the philtral columns by coursing above the surface of the orbicularis oris to insert into the lower philtral columns and vermilion border as far medially as the peak of Cupid’s bow. Anatomically and functionally, the orbicularis oris muscle consists of two parts, superficial and deep. The deep layers of the muscle encircle the orifice of the mouth and function as a constrictor. The superficial component also brings the lips together, but its fibers can contract independently to provide expression.12
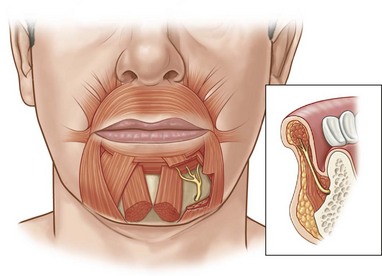
The lower lip depressors consist of the depressor labii inferioris, also known as the quadratus labii inferioris, and the depressor anguli oris, also known as the triangularis (Fig. 11.3). The mentalis, however, is not a lip depressor. Its indirect action on the lip is to elevate it.8 The depressor labii inferioris arises from the lateral surface of the mandible, which is inferior and lateral to the mental foramen. It runs medially and superiorly to insert into the lower border of the orbicularis oris and its surface. Through fibrous septa, it attaches to the vermilion and the skin of the middle third of one side of the lip.9 Its action is to draw the lower lip downward and laterally and to evert the vermilion (e.g., as in showing the lower teeth). The depressor anguli oris arises from the mandible laterally and is superficial to the depressor labii inferioris. The medial fibers insert directly into the skin at the labiomandibular crease; the remainder blend into the modiolus.13 It depresses the angle of the mouth (e.g., in frowning).
Diagnosis and patient presentation
Facial paralysis is a complex clinical problem with numerous consequences affecting the function, self-image, and social interactions of those afflicted and their families (Fig 11.4). Function of the muscles vital for the protection of the eye, maintenance of the nasal airway, oral continence, and clear speech may be lost. These muscles support the face at rest and enable an individual to wink, pucker the lips, and express emotions of surprise, joy, anger, and sorrow.
The emotional effects of facial paralysis cannot be underestimated. The unilaterally paralyzed face presents obvious asymmetry at rest, exacerbated by an attempt to smile (Fig. 11.5). As a result, these patients avoid situations in which they are required to smile. They become characterized as serious and unhappy, and their psychosocial functioning is frequently poor. A patient with bilateral facial paralysis has severe disability because his or her face cannot convey emotion.
Classification
In the formulation of a treatment plan, it is helpful to have a practical and clinically oriented classification. This will facilitate sound decision making and realistic surgical planning. Facial paralysis can take many forms. It can be classified anatomically and as congenital or acquired, and it can be broken down further into unilateral or bilateral categories.14 In addition, the degree of muscle involvement varies from total to partial paralysis. More than 50% of patients with facial paralysis suffer from Bell’s palsy and often recover fully.
It is estimated that facial paralysis occurs in 2.0% of live births.15 In the majority of patients, it is believed to be the result of intrauterine pressure on the developing fetus from the sacral prominence. The facial nerve is superficial and easily compressed. This leads to the panfacial type and buccal branch variety of congenital facial paralysis. It is believed, however, that the mandibular branch component and syndromic forms of facial paralysis may have a different etiology. In the authors’ experience, the cause of unilateral facial paralysis was congenital in two-thirds of patients encountered and acquired in one-third of patients. Acquired facial paralysis resulted from intracranial tumors in 50% of patients; and acquired facial paralysis from extracranial trauma. The majority of traumas were related to surgical procedures, most commonly cystic hygroma excision. In infants, the nerve is superficial at birth and can easily be traumatized through external compression or surgical misadventure. In contrast, the cause of facial paralysis for the majority of adults is acquired, from either intracranial lesions or inflammatory processes, such as Bell’s palsy.
Throughout all of these areas, however, facial paralysis constitutes a spectrum of involvement. It may be complete or incomplete to varying degrees, obvious in some patients, and subtle in others (Table 11.2).
Table 11.2 Classification of facial paralysis
| Extracranial |
| Traumatic |
| Neoplastic |
| Congenital absence of facial musculature |
| Intratemporal |
| Traumatic |
| Neoplastic |
| Infectious |
| Idiopathic |
| Congenital: osteopertosis |
| Intracranial |
| Iatrogenic injury |
| Neoplastic – benign, malignant, primary, metastatic |
| Congenital |
| Absence of motor units |
| Syndromic |
Patient selection
The presence of synkinesis, the simultaneous contraction of two or more groups of muscles that normally do not contract together,16 should be documented. Synkinesis is thought to occur from a misdirected sprouting of axons. The most common types of synkinesis are eye closure with smiling,17 brow wrinkling when the mouth is moved,18 and mouth grimacing when the eyes are closed.
Treatment: nonsurgical and surgical
Nonsurgical management
Nonsurgical management of the patient with facial paralysis applies primarily to the eye and can frequently make the difference between a comfortable eye and a painful one. Nonsurgical maneuvers can protect the eye while surgery is being planned and are regularly used in concert with the surgical management of the eye. In some instances, surgery may be avoided. Nonsurgical management of the eye consists of protecting the eye and maintaining eye lubrication (Table 11.3).
Table 11.3 Nonsurgical maneuvers to protect the eye
Eye lubrication can be provided by a number of commercially available preparations. This includes clear watery drops containing either hydroxypropyl methylcellulose or polyvinyl alcohol along with other agents including preservatives. These drops function by absorbing into the cornea and lubricating it. Although the duration of action will vary, most are retained on the surface of the eye between 45 and 120 minutes.19 Thus, to be most effective, they should be instilled frequently during the day. Thicker ointments containing petrolatum, mineral water, or lanolin alcohol are retained longer and can be used at night to protect and “seal” the eyelids during sleep. The patient who presents with excessive tearing may in fact have a dry eye and may benefit from the use of artificial tears. Corneal ulceration should be managed with prompt referral for ophthalmologic assessment.
In patients in whom there is incomplete facial nerve paralysis or recovering muscle activity after nerve injury, function may be improved with neuromuscular retraining supervised by an experienced therapist. This consists of various treatment modalities such as biofeedback, electromyography, and self-directed mirror exercises using slow, small, and symmetric movements.20 Patients can often relearn some facial movements or strengthen movements that are weak.
Surgical management
Deciding on a surgical procedure can initially seem daunting. There are a number to choose from, and selecting the most appropriate reconstruction may be confusing. It is important to listen to each patient carefully to identify which aspects of the paralysis are most troublesome and to treat each region of the face separately. The age of the patient, duration of the facial paralysis, condition of the facial musculature and soft tissues, and status of the potential donor nerves and muscles will all influence treatment options. One must consider the patient’s needs carefully and match the needs of the patient with the skill of the surgeon (Table 11.4).
Table 11.4 Most common surgical options for each region of the face
| Brow (brow ptosis) |
| Upper eyelid (lagophthalmos) |
| Lower eyelid (ectropion) |
| Nasal airway |
| Commissure and upper lip |
Nerve transfer either directly or via nerve graft to reinnervate recently paralyzed muscles Microneurovascular muscle transplantation with the use of ipsilateral seventh nerve, cross-facial nerve graft, or other cranial nerve for motor innervation Temporalis transposition with or without masseter transposition Soft-tissue balancing procedures (rhytidectomy, mucosal excision or advancement) |
| Lower lip |
Brow
There are at least three approaches to a brow lift: direct excision of the tissue above the brow (direct brow lift), open brow lift performed through a coronal incision, and endoscopic brow lift. Unilateral frontalis paralysis may cause a difference in brow heights of up to 12 mm. A direct brow lift is best able to correct such a large discrepancy. Direct brow lift involves excision of a segment of skin and frontalis muscle just above and parallel to the eyebrow. If the incision is placed just along the first line of hair follicles, the resulting scar is usually less noticeable. Frontalis shortening by excision and repair provides a reliable correction, which minimally relaxes over time. However, overcorrection is still required. Slight overcorrection is particularly beneficial if the person’s normal side of the forehead is quite active during facial expression. Branches of the supraorbital nerve should be identified and preserved because they lie deep to the muscle (Fig. 11.6).
Upper eyelid
Several techniques are available for the management of lagophthalmos. These are all directed at overcoming the unopposed action of the levator palpebrae superioris. Because of its relative technical ease and reversibility, lid loading with gold prosthesis is the most popular technique. The patient’s eyelid configuration is important in determining whether the bulge of the gold weight will be visible when the eye is open. If the amount of exposed eyelid skin above the lashes is more than 5 mm when the eye is open, the gold weight is likely to be noticeable to the patient. If the distance is less than 5 mm, the gold weight will roll back and be covered by the supratarsal skinfold (Fig. 11.7).
Because of its inertness, 24-carat gold is used; allergic reactions are rare, but if they occur, platinum weights are also available. Prostheses are available in weights ranging from 0.8 to 1.8 g. Adequate improvement in eye closure can be obtained with a weight of 0.8–1.2 g, giving the patient a comfortable eye without weight-related problems.21
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree