Dermal Hypertrophies and Benign Fibroblastic/Myofibroblastic Tumors: Introduction
|
Dermal hypertrophies and benign fibrous tumors are quite common. Some of the entities described have characteristic clinical presentations and histopathologic features. Many primarily present in infancy and childhood (Table 66-1). A unifying histologic feature of hypertrophic scars and most of the rarer entities described is the presence of myofibroblasts, contractile spindle cells that express smooth muscle actin but not desmin (Table 66-2). Malignant fibrous tumors of the dermis are discussed in Chapter 125.
Skin Involvement | Entity | Typical Site(s) |
|---|---|---|
Often solitary | Infantile digital fibromatosis Myofibroma Calcifying aponeurotic fibroma Plantar fibromatosis Infantile fibromatosis Fibrous hamartoma of infancy Fibromatosis colli Cranial fasciitis | Digits Head/neck Palms/soles Soles None Upper arm/trunk Clavicle area Head/neck |
Often multiple | Juvenile hyaline fibromatosis | Ears/face and other sites |
Often multiple with visceral involvement | Infantile systemic hyalinosis Infantile myofibromatosis | Ears/face and other sites None |
Fibroblast | Myofibroblast | Smooth Muscle Cell | |
|---|---|---|---|
Nucleus | Tapered | Tapered to cigar-shaped | Cigar-shaped |
Positive immunohistochemical stains | Vimentin CD34 (sometimes) | Vimentin Smooth muscle actin Muscle specific actin | Vimentin Smooth muscle actin Muscle specific actin Desmin |
Negative immunohistochemical stains | Smooth muscle actin Muscle specific actin Desmin | Desmin |
Hypertrophic Scars and Keloids
Keloids and hypertrophic scars are related clinical lesions.1 These lesions present at sites of prior dermal injury and wound repair. They often occur after local skin trauma (e.g. laceration, tattoo, burn, injection, ear piercing, vaccination, or surgery) or inflammatory skin disorders (e.g. acne, bites, or infections). There may be growth of keloids during pregnancy.2 The predisposition to keloids in darker skin3 and reports of a familial, autosomal dominant inheritance4 suggest genetic influences. Hypertrophic scars and keloids show differences morphologically and histologically (Table 66-3),5,6 suggesting differences in pathogenesis. There also is an apparent association with melanin pigment, as albino and vitiliginous skin do not form keloids.7 Multiple keloids may also be associated with a genetic syndrome (Table 66-4).
Keloid | Hypertrophic Scar | |
|---|---|---|
Age | Especially third decade | Any |
Onset after injury | Delayeda | Immediate |
Growth beyond border of original wound | Yes | No |
Spontaneous regression | Rare | Occasional |
Recurrence | Common | Rare |
Distorted shape | Common | Rare |
Histopathology | Thick, hyalinized collagen | Fascicles of myofibroblasts arranged haphazardly |
Treatment response | Poor | Good |
Associated Genetic Syndrome | |
|---|---|
Keloids | Rubinstein–Taybi Goeminne |
Acrochordon-like lesions | Birt–Hogg–Dubéa Gorlin (Nevoid basal cell carcinoma)b |
Fibrous papules/angiofibromas | Tuberous sclerosisc Multiple endocrine neoplasia type I Birt–Hogg–Dubé |
Fibrofolliculomas/trichodiscomas | Birt–Hogg–Dubé |
Connective tissue nevus | Tuberous sclerosisd Buschke–Ollendorfe Familial cutaneous collagenoma Multiple endocrine neoplasia type I Birt–Hogg–Dubé Ehlers–Danlos (hypermobile, type III) Hunter/Hurler |
Sclerotic fibroma (circumscribed storiform collagenoma, plywood fibroma) | Cowden |
Desmoid tumor | Gardner/Familial adenomatous polyposisf Familial infiltrative fibromatosis/Hereditary desmoid disease |
Cutis verticis gyrata | Turner Noonan Fragile X Klinefelter Tuberous sclerosis Beare–Stevenson Ehlers–Danlos Apert |
Knuckle pads | Bart–Pumphrey |
Cerebriform fibrous proliferation | Proteus |
Gardner fibroma | Gardner/Familial adenomatous polyposis |
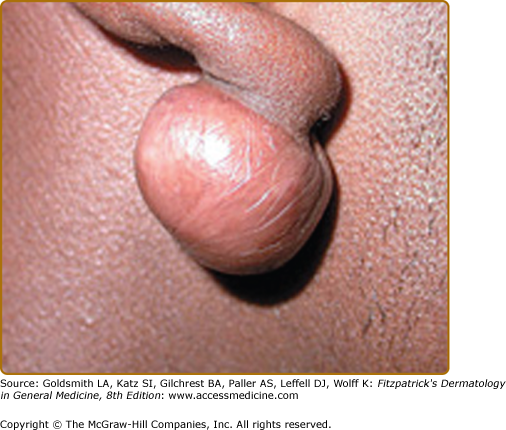
Keloids appear as well-circumscribed pink to purple or hyperpigmented firm nodules (Fig. 66-1) or plaques. The surface of keloids is usually smooth, but can be nodular and borders are often smooth, but can be irregular (Table 66-3). The surface and borders of hypertrophic scars are always smooth and regular. There is a predilection for developing keloids at sites of increased tension, such as the shoulders, sternum, mandible, and arms. Keloids also commonly affect the earlobes. Keloids and hypertrophic scars are often painful, hyperesthetic, or pruritic. Ulceration can occur. Multiple keloids are common, but several rare entities may be considered in the clinical differential diagnosis (see Box 66-1).8–11 Histopathologically, keloids are composed of thick, haphazard, eosinophilic, collagen bundles. Hypertrophic scars are more cellular with myofibroblasts either in disorganized whorls or sometimes oriented parallel to the epidermis.
Although the exact mechanism of keloid formation is still unclear,12–19 TGF-beta and its signaling pathway are important (see Table 66-5).12 Hypertrophic scars are associated with HLA-DRB16.20 In most studies, keloids and scars show the same biochemical and pathologic abnormalities. Keloids express increased levels of the gli-1 protein, an oncogene product also present in neoplasms such as basal cell carcinoma.21 Collagen synthesis and collagenase activity are increased in both keloids and hypertrophic scars. α1-Globulin (a collagenase inhibitor usually not present in normal scars) may contribute to increased collagen deposits. Hypertrophic scars have decreased levels of the profibrotic agent tumor necrosis factor.22 Keloids contain tenascin C, a protein associated with inflammation and wound healing.23 Fibroblasts from keloid-prone patients have altered cytokine patterns24 and increased sensitivity to transforming growth factor- β1 (TGF- β1),25 TGF-β2,26 platelet-derived growth factor, and epidermal growth factor.27 Carbon dioxide laser treatment reduces TGF- β1 levels in keloids.28 At least, part of the fibroblast stimulation may be secondary to infiltration of the scar by activated T cells.29 Also, there seem to be decreased levels of apoptosis, as shown by terminal transferase dUTP nick end labeling (TUNEL) assays and increased Bcl-2 and p53 expression in keloid-associated fibroblasts.30
Increased | Decreased |
|---|---|
Transforming growth factor-β Platelet-derived growth factor Vascular endothelial growth factor Collagen Cytokines (e.g., IL-1, IL-6) Cyclooxygenase 2 Plasminogen activator inhibitor-1 Matrix metalloproteinase-2 | SMAD proteins (e.g., SMAD7) Apoptosis |
The treatment of hypertrophic scars and keloids differs slightly.7,31 Hypertrophic scars tend to be more responsive than keloids and generally flatten with time. Although injection of hypertrophic scars and keloids with intralesional steroids is a first-line treatment in many cases, depending on the situation (e.g. a wound previously infected, a wound across lines of tension or a joint), hypertrophic scars may respond quite well to surgery as an initial treatment. Surgery alone is generally not recommended for keloids, as they often recur as larger lesions. An exception to this may be keloids on the earlobes.32 An algorithm for treatment is outlined in Treatment Box 66-2.
Hypertrophic Scars | Keloids | |
|---|---|---|
First-line | Intralesional steroids or sometimes surgical excision/revision | Intralesional steroids |
Potential modalities for use in combination with first-line or second-line treatment | Often not necessary | Cryotherapy Pressure Silicone gel sheeting |
Second-line | Often not necessary | Laser therapy Intralesional 5-fluorouracil Surgerya Radiation Bleomycin |
Dermatofibroma (Fibrous Histiocytoma, Sclerosing Hemangioma)
Dermatofibroma is a common, benign tumor that has a predilection for the lower legs of women. Any age may be affected, but typically dermatofibromas appear in the 20s and 30s. Dermatofibromas may be solitary or multiple and eruptive (see Box 66-3).33 Trauma, such as secondary to insect bites, has been thought to induce some lesions, suggesting a reactive/reparative process. The recent demonstration of clonal X-inactivation in some cases of dermatofibroma supports a neoplastic nature.34,35
Systemic lupus erythematosus Human immunodeficiency virus infection Immunosuppression of other cause (e.g., immunosuppressive drugs, especially in the setting of patients with autoimmune disease, lymphoma/leukemia, organ transplant) Case reports of atopic dermatitis, pulmonary hypertension, hydronephrosis, myasthenia gravis, pemphigus, pregnancy, sarcoidosis, hyperlipidemia |
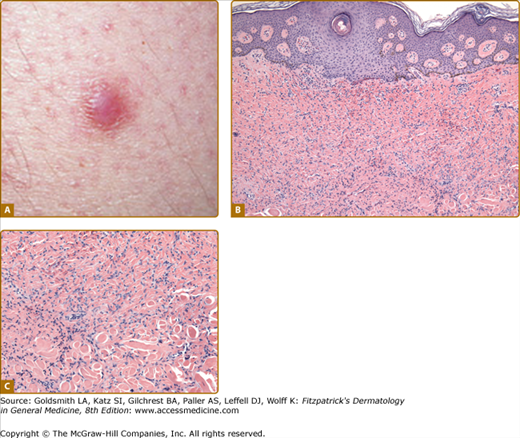
Usually asymptomatic, they occasionally are pruritic or painful. Some tumors grow very rapidly, whereas others remain static for many years. Characteristically, a dermatofibroma is firm, measuring from 0.5 mm to 1 cm in diameter, and lateral compression produces a dimple-like depression in the skin. The surface may be shiny or keratotic, and the color is variable, often brown but sometimes pink, red, tan, or flesh colored (Fig. 66-2A).
Histologically, the epidermis is usually hyperplastic and hyperpigmented. There may be follicular or sebaceous induction. The dermis has fascicles or haphazardly arranged collections of spindle cells that lack atypia in most cases (see Figs. 66-2B and 66-2C). The edges of the lesion are poorly defined with individual cells hugging collagen bundles (“collagen entrapment”). Mitotic figures may be present, but atypical forms are not a feature. Dermatofibromas are generally factor XIIIa-positive36 and CD34−.37 There are many histologic variants of dermatofibroma, most without clinical significance. Exceptions are in Box 66-4.
Clinical Features
Histologic Features
|
No treatment is necessary unless symptomatic. A common reason for removal is repeated trauma to the dermatofibroma, often secondary to shaving the lower legs. Cryosurgery may be helpful in flattening out the dermatofibroma but usually is not curative. Lesions termed “atypical,” “cellular,” “deep,” and/or “indeterminate” are generally best treated with complete excision, particularly if clinical size is >2 cm (see Box 66-4).38–44
Acrochordon (Fibroepithelial Polyp, Skin Tag, Soft Fibroma)
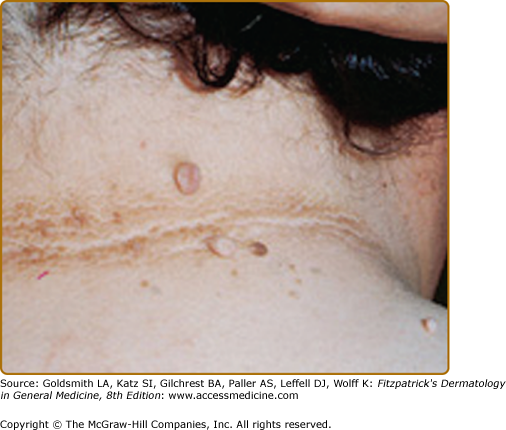
Acrochordons are pedunculated papules or tumors that are most commonly located on the eyelids, neck, axillae, and groin. There is a familial disposition, and acrochordons are more commonly seen in obese individuals, sometimes overlying acanthosis nigricans (Fig. 66-3). Acrochordon-like clinical lesions may be a feature of a genetic syndrome, although histologically there are differences (see Table 66-4).45,46 Histologically, an acrochordon is a polypoid lesion with a central collagenous core. Adnexal structures are generally absent. Although usually asymptomatic, lesions can become irritated or necrotic. Patients often request removal for cosmetic reasons.
Fibrous Papule (Angiofibroma)
A fibrous papule is a common papule on the lower portion of the nose or the central face. It usually presents in adulthood. Multiple lesions are a feature of certain genetic syndromes (see Table 66-4),47–51 but occasionally may be seen in patients with no other stigmata of a genetic disorder.52 The fibrous papule is small (2–5 mm), nontender, flesh colored (sometimes pink or slightly hyperpigmented), firm, and dome shaped. It must be differentiated from an early, nodular, basal cell carcinoma, and biopsy may be necessary. Unlike a basal cell carcinoma, it rarely bleeds and stays relatively stable in its smaller size. Histologically, the dermis shows fibrosis with stellate fibroblasts and dilated vessels. Identical histology is seen in pearly penile papules and periungual fibromas (Koenen’s tumors) (see Chapter 140). No treatment is necessary, and a simple shave or punch excision is usually curative.
Fibrofolliculoma/Trichodiscoma
Fibrofolliculomas/trichodiscomas are 2- to 4-mm, dome-shaped, yellowish to skin-colored papules located on the head, neck, and upper trunk; multiple lesions may be associated with Birt–Hogg–Dubé syndrome (see Table 66-4).45
Connective Tissue Nevus/Collagenoma/Elastoma
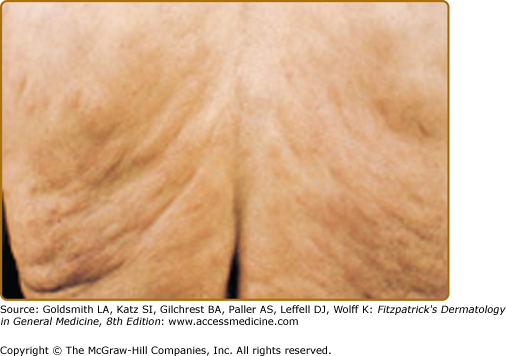
These hamartomas can be divided into familial, those associated with genetic disease (see Table 66-4),47,50,53–57 and other isolated variants. Connective tissue nevi present as asymptomatic, flesh-colored to yellow–brown papules or plaques that may be solitary or grouped, linear, or irregular in distribution (Fig. 66-4).58 The overlying epidermis is usually smooth. Histologically, connective tissue nevi show a normal epidermis overlying collagen in the lower dermis. The collagen may be subtly increased, thickened, or oriented vertically to the epidermis, and muscin may be increased. Elastic fibers may also be increased (elastoma).
Desmoid Tumor (Aggressive Fibromatosis)
Desmoid tumors, also known as deep or aggressive fibromatoses, are a type of fibromatosis. All types (extra-abdominal, abdominal wall, intra-abdominal) may be induced by trauma (Fig. 66-5). Mutations have been found in the adenomatous polyposis coli (APC) gene (5q21).61 Hormonal influences (e.g., pregnancy) are implicated in abdominal wall tumors.62 Tumors associated with Gardner/Familial adenomatous polyposis (FAP) (see Table 66-4)63 are often intra-abdominal,64 may be more aggressive and surgically unresectable, and are associated with a 10% mortality.65 Extra-abdominal tumors are deep-seated, often located in the area of the shoulder and pelvic girdle, chest wall, or head and neck.66 Although surgery is widely accepted as first-line treatment,67
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree