Wound Care
Donald W. Buck
Robert D. Galiano
INTRODUCTION
The wound is a microcosm of the patient. While most wounds heal without intervention in healthy individuals, patients with systemic diseases or acute illnesses can develop non-healing wounds that require evaluation by a plastic surgeon. In general, the plastic surgeon is consulted to evaluate three types of wounds: (1) the acute wound where the final appearance may be the principal concern, (2) the wound in a patient whose medical status and/or mode of injury predisposes him or her to wound healing difficulties and the threat of a problem wound, or (3) the chronic wound refractory to past interventions.
In recent years, significant strides have been made in our overall understanding of problem wound physiology. This has led directly to clinical advances that have resulted in better treatments and overall wound care. With the staggering prevalence of chronic wounds and an ever-increasing armamentarium of wound care tools, it is imperative that the plastic surgeon maintain an updated understanding of wound healing biology and the principles of wound care. In this chapter we will focus on the basics of wound care and highlight some of the recent advances in this dynamic and expanding field.
FUNDAMENTALS
All wounds, whether acute or chronic, should be evaluated by a physician to determine their mechanism and to outline an approach to treatment. Tetanus prophylaxis is administered when prior immunity is unknown or the most recent booster vaccine is over 5 years old. A thorough history and physical examination should be performed, with particular emphasis on any aspect that relates to the wound cause and/or persistence (e.g., comorbidities, systemic diseases, and medications). The term wound encompasses a broad range of lesions without consideration to etiology, and the list of possible etiologies is vast. Table 3.1 lists some of the major factors, both systemic and local, that can have profound effects on wound healing.
Adjunctive diagnostic tests are guided by history and physical examination of the wound. Some useful studies include laboratory tests that reflect nutritional status (albumin, prealbumin, and transferrin levels), the level of physiologic inflammation (C-reactive protein and erythrocyte sedimentation rate), and the degree of diabetes control (plasma glucose and hemoglobin A1c). In addition, patients should have a recent complete blood count and basic chemistry panel to assess for leukocytosis, anemia, and renal disease. Other useful laboratory tools include transcutaneous oxygen pressure (tcPo2) measurements, toe pressures, neurofilament testing, and ankle-brachial index (ABI) (Chapter 95). Results of these tests may direct the need for procedures such as surgical revascularization. Wound parameter documentation is also useful to monitor the progression of wound healing in an objective manner.
The main fundamentals of wound care are summarized in Table 3.2. To attain these goals, it is useful to emphasize the common causative factors that are shared by problem wounds, as opposed to isolating the differences between diverse types of wounds. With this more simplistic view, it is possible to link the majority of problem wounds to a combination of three factors: age, ischemia (including repeated episodes of ischemia-reperfusion injury), and bacterial infection. By understanding and addressing these factors, the surgeon will be able to manage most wounds.
Age and Wound Healing
Although most wounds heal without incident in aged patients, there is a slight, but consistent, decline in wound healing rates in the elderly. This decline is exacerbated when ischemia and infection are superimposed. Laboratory studies reveal a functional decline in aged fibroblasts and endothelial cells that leads to accelerated senescence, diminished growth factor production, decreased stress response to hypoxia and toxins, and a reduction in collagen and matrix production. Interestingly, aged cells share many of the same molecular derangements as those seen in diabetic patients and irradiated wound beds. Obviously age cannot be reversed; however, it should be considered an important component of wound pathology and prompt the surgeon to aggressively optimize appropriate systemic parameters in these patients (nutrition, infection, ischemia, etc.). The use of growth factors or advanced wound protocols should be considered earlier in the elderly patient.
Ischemia and Wound Healing
The role of hypoxia in wound healing is well established. In fact, local tissue hypoxia is a common characteristic of most chronic wounds. The diffusion of oxygen and nutrients from capillaries to cells is limited to a distance of 60 to 70 µm in a person breathing room air. Therefore, anything that increases tissue diffusion requirements or limits available capillary delivery systems will establish a hypoxic environment. For example, oxygen tension in wound tissues is reduced an average of 15 to 20 mm Hg (25 vs. 40 mm Hg) as a result of the damage to small vessels in periwound areas. Likewise, the tissue fibrosis commonly encountered in chronic wounds can create a significant barrier to oxygen diffusion that subsequently produces persistent tissue hypoxia and further fibrosis.
TABLE 3.1 FACTORS THAT CONTRIBUTE TO WOUND HEALING IMPAIRMENTS | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
TABLE 3.2 BASIC FUNDAMENTALS OF WOUND CARE | ||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
While hypoxia alone is an important component of chronic wounds, most problem wounds are characterized by repeated episodes of ischemia followed by reperfusion. The detrimental effects of ischemia-reperfusion injury have been well established in cardiac pathology and organ transplantation, but are underappreciated in cutaneous wound healing. Reperfusion injury is particularly important in lower extremity wounds, where walking and standing can lead to localized ischemia in pressure-bearing areas, or through increased edema in patients with venous stasis. Pressure relief, through sitting, rest, and foot elevation, leads to resumption of adequate tissue perfusion and a vicious cycle ensues. Repeated episodes, sometimes multiple per day, result in gradual cellular damage and a chronic milieu of persistent inflammation. Similar cycles of ischemia-reperfusion may also occur in patients with pressure sores as they shift about in bed or wheelchairs.
Surgical and nonsurgical interventions can be undertaken to maximize oxygen delivery to tissues. Examples include elevation of edematous extremities, off-loading pressure points, debridement of necrotic tissue or foreign bodies that act as a physical barrier to diffusion, pain control that reduces sympathetic constriction of peripheral vasculature associated with the “fight-or-flight” response, heating that will result in vasodilatation of cutaneous vasculature, and smoking cessation and hydration that increase oxygen delivery at the cellular level. Recent research indicates that the benefits of ensuring adequate oxygen delivery to a wound not only are restricted to established wounds but may also be useful in preventing wound complications.
Bacteria and Wound Healing
All wounds are contaminated, but excessive numbers of bacteria will interfere with wound healing. A quantitative culture of 105 bacteria per gram of tissue is usually diagnostic of infection. However, this tool is rarely used because few microbiology laboratories perform the test reliably. Furthermore, the value of 105 is relative and not universally applicable. In fact, more virulent strains of bacteria can establish systemic infections at much lower densities. The presence of diabetes, ischemia, or other comorbidities will also lower the threshold needed to establish a true infection to an unknown extent. Likewise, as more research on the physiology of bacterial biofilms is introduced, it is likely that only a fraction of the 105 bacterial count is actually necessary to establish a biofilm and create a significant barrier to wound healing.
An important mechanism by which tissue hypoxia predisposes wounds to infection is by impairing the “oxidative burst” essential to microorganismal killing by leukocytes. This enormously elevated production of oxygen-derived radicals is a self-regulated process that is important in clearing the wound off bacteria. Notably, this process of radical production, which is normally limited to the early stages of wound repair, can be aberrantly prolonged in the setting of persistent infection or inflammation (Figure 3.1). This can result in bystander damage to the body’s normal cells and in many cases characterizes the microenvironment of the indolent wound. This explains the benefit of dressings and the avoidance of foreign debris (and highlights the importance of delicate tissue handling and the proper choice of suture material) in expediting healing.
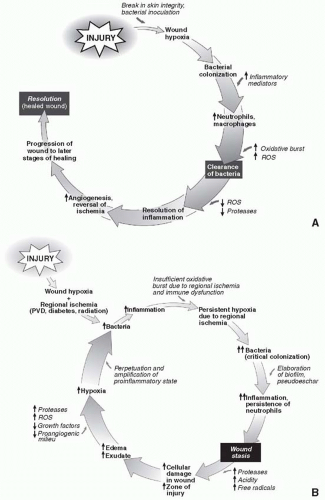 FIGURE 3.1. The normal healing milieu. A. Normal response to injury. B. Response to injury in the problem wound. ROS, reactive oxygen species; PVD, peripheral vascular disease. |
Bacteria exert adverse effects on wound healing in several ways. As mentioned above, through a persistent inflammatory response, they establish an environment of free radicals, secreted toxins, and proteases that act to degrade growth factors, prevent ordered assembly of matrix proteins, and result in the creation of proteinaceous debris that constitutes a pseudoeschar. In addition, they place a significant metabolic strain (bioburden) on the wound that the host may not be able to overcome. Importantly, wound bioburden is often stratified as a prognostic indicator and to assist in management decisions. Wounds may be considered contaminated (bacteria present without proliferation), colonized (bacteria present and multiplying without overt host reaction), critically colonized (the tipping point where host response is overcome by bacterial proliferation), or infected (expanding bacterial quantity with ongoing host reaction). Critical colonization of a wound or infection is often heralded by stasis in the progression of a wound that was previously healing. In fact, if the rate of healing decreases in any wound, it should be considered infected until proven otherwise. Other signs of bioburden progression and/or overt wound infection include increasing pain in the periwound area, increased wound edema, malodorous discharge, increased drainage, or purulence.
Systemic antibiotics are unnecessary for most wounds. By definition, most wounds are open and thus adequately managed through “drainage” and proper debridements. In addition, systemic antibiotics are only delivered to adequately perfused tissues; therefore, in the setting of most problem wounds, they are ineffective. However, there are settings where systemic antibiotics are important. In general, any wound that is complicated by surrounding cellulitis should be treated with adjunctive antibiotics. As mentioned, any wound where the rate of healing decreases is considered infected. Increased pain is another indication of a worsening infection. Another sign of infection is the appearance of straw-colored “oozing” from the skin; this is actually likely evidence of an underlying Staphylococcus cellulitis or lymphangitis. Antibiotics should also be considered in wounds contaminated by oral flora or animal bites, as well as in patients with mechanical implants. In general, surface irrigation and lavage with saline may be all that is necessary for truly contaminated wounds, whereas topical antibiotics and surgical debridement are often essential management tools for overtly infected wounds.
ADJUNCTS TO WOUND CARE
Debridement
Debridement is the single most important wound care tool to reduce bioburden and promote healing. Without adequate debridement, a wound is persistently exposed to cytotoxic stressors and competes with bacteria for scarce resources such as oxygen and nutrients. Many surgeons underappreciate the importance of adequate debridement in the management of both acute and chronic wounds. While most surgeons recognize the importance of debridement of grossly necrotic or foreign material, many still allow wounds to “heal” under a “biologic dressing” or eschar.
An eschar begins as a pseudoeschar, which is a provisional matrix of exudated serum components at the wound-air interface. If allowed to dry, the gelatinous pseudoeschar will harden to form a true eschar, or scab. Pseudoeschars and eschars may play a role in prolonging the inflammatory stage of wound healing, and hence establish an environment ripe for bacterial colonization in the compromised patient or susceptible wound bed. Likewise, the proteinaceous components of the eschar are appetizing nutrients for most bacteria. Therefore, any pseudoeschar or eschar should be debrided as it accumulates. An effective way to do this is through the proper use of dressing and debriding agents, as detailed below and in Table 3.3.
Debridement is typically considered a surgical tool, but it may also be accomplished through the use of enzymatic, mechanical, or autolytic (through host leukocyte action) means. Wound care manufacturers have produced numerous enzymatic and pro-autolytic agents. While they have been proven effective in mildly debriding wounds, their use should not supplant sharp surgical debridement as the method of choice for more heavily contaminated wounds or wounds with thicker levels of slough or eschar. Enzymatic and pro-autolytic agents work through preventing the cross-linking of exudated components and impede the bacteria-sequestering pseudoeschar and biofilms from forming. Mechanical debridement can be achieved through dressings, or newer pressurized water devices, such as the VersaJet (Smith & Nephew, Largo, FL), Waterpik (Waterpik Technologies, Fort Collins, CO), pulselavage, or shower spray devices. Mechanical debridement is effective at reducing bacterial counts and should be considered adjuncts to surgical debridement. Similarly, a syringe with a 20-gauge needle will generate the 15 psi necessary to lower bacterial counts in tissue.
For historical purposes, another effective means of achieving wound debridement is through the use of maggot therapy. Maggots preferentially feed on devitalized tissue and spare viable, well-perfused tissue; their secretions also target bacterial biofilms. Although they are used sparingly throughout most parts of the country, some centers utilize maggot therapy extensively.
Negative-Pressure Wound Therapy
Negative-pressure wound therapy (NPWT) has been a significant advance for the wound care practitioner. It consists of the use of a porous sponge within the wound, covered by an airtight occlusive dressing, to which a vacuum is applied. This modality has many uses and has found its way into the armamentarium of a wide array of surgical and nonsurgical specialties. It should best be thought of as an adjunct to assist in surgical closure of a problem wound. It can and has been used to completely heal a wound, but use in this manner is timeconsuming, expensive, labor-intensive, and not always effective. A more practical indication is to expeditiously prepare a wound bed for surgical closure by tertiary intent.
NPWT works through multiple important mechanisms including reduction of edema and removal of wound fluid rich in deleterious enzymes, both patient and bacteria derived. In addition, the cyclic compression and relaxation of the wound tissue likely stimulates mechanotransduction pathways that result in increased growth factor release, matrix production, and cellular proliferation.
Common clinical scenarios amenable to NPWT include lymphatic leaks, venous stasis wounds, diabetic wounds, wounds with fistulae, sternal wounds, orthopedic wounds, and abdominal wounds. Likewise, NPWT is used frequently as an alternative to bolster dressings for split thickness skin grafts. Notably, by reliably encouraging granulation tissue formation and reducing wound edema, NPWT has permitted normally emergent wounds to be managed in a nonemergent fashion, allowing for medical stabilization and optimization prior to advanced reconstructive procedures. In some instances, it has even enabled avoidance of free tissue transfer.
There are several contraindications to the use of NPWT, and these include the presence of a malignancy, use on wounds characterized by ischemia, as well as inadequately debrided or badly infected wounds. There have been reports of extension of the zone of necrosis when used on ischemic wounds; for this reason, these patients should be revascularized prior to application of NPWT.
TABLE 3.3 COMMON DRESSINGS IN WOUND CARE
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|
|---|





