54
Vitiligo and Other Disorders of Hypopigmentation
Introduction/Definitions
• Hypomelanosis: an absence or reduction of melanin in the skin that may be due to any one or a combination of the following:
1. A decrease in the number of melanocytes (e.g. vitiligo).
2. A decrease in melanin synthesis by a normal number of melanocytes (e.g. albinism).
3. A decrease in the transfer of melanin to keratinocytes (e.g. postinflammatory hypopigmentation).
• Amelanosis: total absence of melanin in the skin.
• Depigmentation: usually implies a total loss of skin color (e.g. as in vitiligo).
• Poliosis: a lock of scalp hair, eyebrows, or eyelashes that is white or lighter in color.
• Canities: generalized depigmentation of scalp hair.
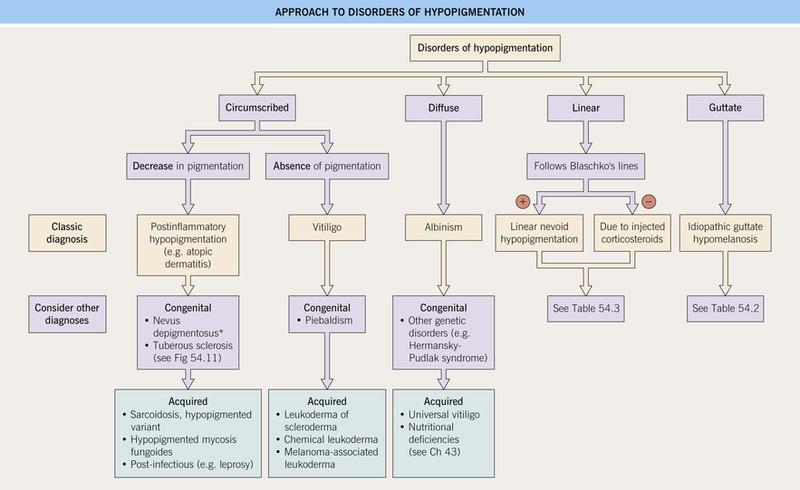
Approach to Disorders of Hypopigmentation
Vitiligo
• An acquired disease, due to autoimmune destruction of melanocytes, that is characterized by circumscribed, amelanotic macules or patches of the skin and mucous membranes (Fig. 54.2); hairs within involved areas may be depigmented or pigmented; the uveal tract and retinal pigmented epithelium can also be affected.


Fig. 54.2 Vitiligo. A Complete loss of pigment of the glans penis. Note the lack of any secondary changes. B Depigmentation of the volar wrists as well as the palmar surfaces; easily recognizable in darkly pigmented individuals. Courtesy, Jean L. Bolognia, MD.
• Two major subtypes of vitiligo: generalized (most common) and localized (Fig. 54.3).
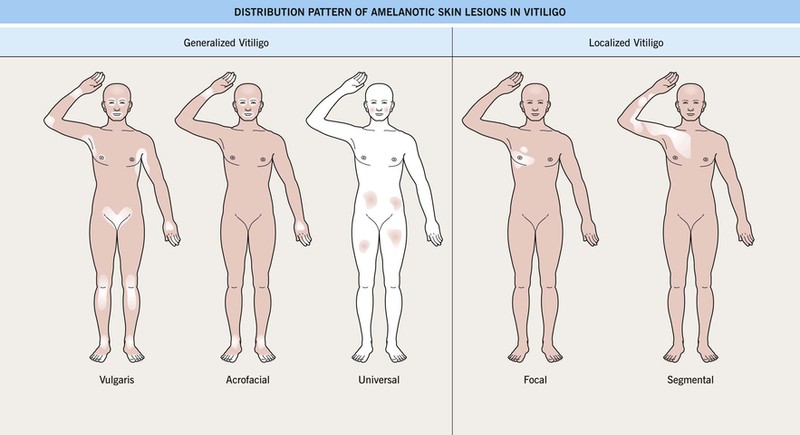
Fig. 54.3 Distribution of amelanotic skin lesions in vitiligo. Vitiligo is clinically divided into two broad categories: generalized and localized. The three distribution patterns in generalized vitiligo include vulgaris, acrofacial, and universal. In focal vitiligo, the amelanotic macules or patches are limited to one or only a few areas, but not necessarily in a segmental pattern, as in segmental vitiligo, which is also unilateral and respects the midline. Adapted with permission from Le Poole C, Boissy RE. Vitiligo. Semin. Cutan. Med. Surg. 1997;16:3–14.
• 10–15% of patients with generalized vitiligo have systemic autoimmune diseases, in particular thyroid disease (Hashimoto’s thyroiditis or Grave’s disease), pernicious anemia, Addison’s disease, and AI-CTD (e.g. SLE); associated cutaneous disorders include halo melanocytic nevi, alopecia areata, and lichen sclerosus.
– Includes acrofacial, vulgaris, and universal (see Fig. 54.3); occasionally an inflammatory edge is seen (Fig. 54.4).
– Usually begins in childhood; typically presents in a unilateral, segmental pattern that respects the midline and usually remains stable in size after 1–2 years (Fig. 54.5).


Fig. 54.5 Segmental vitiligo. A Unilateral band of depigmentation on the face, the most common location for segmental vitiligo. Note the pigmented and depigmented hairs within the affected area. B Under normal light, vitiligo can be subtle in lightly pigmented individuals. The clue to the diagnosis is the poliosis of the eyelashes. A, Courtesy, Kalman Watsky MD; B, Courtesy, Jean L. Bolognia, MD.
– DDx: nevus depigmentosus (decreased but not total loss of pigment).
• DDx of depigmented lesion(s).
• Vitiligo and ocular disease.
• Rx: primarily directed at repigmentation of patient-desired areas (Fig. 54.7).
– The efficacy of treatment depends on four variables.
1. Site: face, neck, mid extremities > acral, mucosal (i.e. sites without hairs).
4. Pigmented hairs within the vitiligo patch: presence > absence.
– Repigmentation usually appears in a perifollicular pattern (Fig. 54.6) and/or from the periphery of lesions.
– 10–20% monobenzyl ether of hydroquinone (MBEH) is sometimes used as depigmentation therapy for widespread or treatment-resistant vitiligo, but it can be permanent and lead to loss of pigment in areas distant to the sites of application.

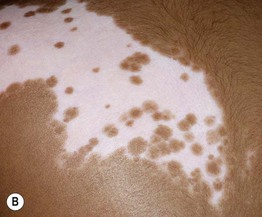
Fig. 54.6 Perifollicular repigmentation. Vitiligo on the elbow (A) and segmental vitiligo on the back (B) responding to PUVA and narrowband UVB therapy, respectively, with repigmentation in a prominent perifollicular pattern as well as from the periphery. The areas of repigmentation are darker in color than the uninvolved skin in (A). A, Courtesy, Jean L. Bolognia, MD; B, Courtesy, Julie V. Schaffer, MD.
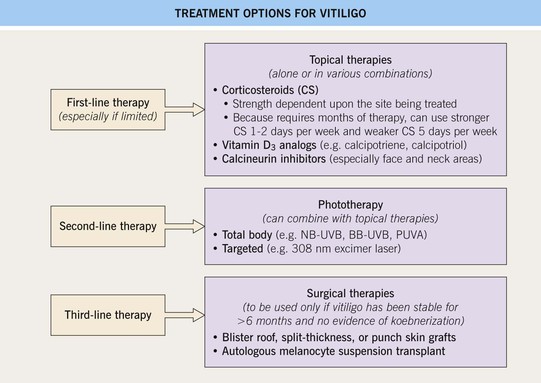
Fig. 54.7 Treatment options for vitiligo. Treatment of vitiligo is directed at repigmentation of patient-desired areas. Camouflage can be offered to all patients for temporary (e.g. makeup, self-tanners) or more permanent (e.g. tattoos) cosmetic relief. Referral to a support group [e.g. National Vitiligo Foundation (www.mynvfi.org)] may also be helpful. 10–20% monobenzyl ether of hydroquinone (MBEH) is sometimes used as depigmentation therapy for widespread or treatment-resistant vitiligo, but it can be permanent and lead to loss of pigment in areas distant to the sites of application. NB-UVB, narrowband ultraviolet B; BB-UVB, broadband UVB; PUVA, psoralens plus ultraviolet A.
Hereditary Hypomelanosis
Oculocutaneous Albinism (OCA)
• Estimated frequency is 1 : 20 000, but may be 1 : 1500 in areas of Africa.
• Four subtypes of OCA (Table 54.1) exist; nearly always inherited in an autosomal recessive manner; OCA1 and OCA2 constitute ~90% of all cases of OCA.
Table 54.1
Classification of oculocutaneous albinism (OCA).
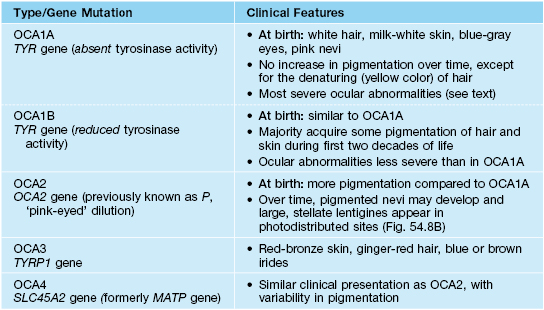
TYR, tyrosinase; OCA, oculocutaneous albinism; TYRP1, tyrosinase-related protein-1; SLC45A2, solute carrier family 45 member 2.
• Early ophthalmologic consultation and strict photoprotection are mandatory; the development of aggressive SCCs (Fig. 54.8A) is a significant cause of morbidity and mortality.