Chapter 14
Viral Infections
OVERVIEW
- Viruses are obligate parasites able to make important changes in cellular function and immune responses of the host.
- As well as modifying genetic material of the host cell, the viral genome itself undergoes changes—shift and drift.
- RNA viruses are unstable, undergoing multiple mutations and causing systemic disease (measles).
- DNA viruses are more stable and cause local infections (human papilloma virus warts, molluscum).
- Herpes simplex infections are acquired by local contact and reactivate at the inoculation site, usually mucosae (lips and genitals).
- Herpes zoster (shingles) is due to reactivation of previously acquired varicella zoster virus (chicken pox).
- Specific antiviral medications are few and therefore the current primary strategy for reducing viral infections is vaccination.
Introduction
The term virus comes from Latin, meaning poison or toxin. Most modern medical practitioners think of viruses as micro-organisms rather than toxins, but some experts argue that viruses are not living organisms as they do not fulfill all the necessary criteria. Viruses do not have cell structures and they require host cells to replicate and synthesise new products. This spontaneous self-assembly within the host cells has been likened to the autonomous growth of crystals. Viral self-assembly has also been used to strengthen the hypothesis that the ‘origins of life’ started from self-assembling organic molecules. Nonetheless, viruses do possess genes, cause disease, trigger immune responses and evolve through natural selection; so, from a practitioner’s point of view, living or otherwise, they have an enormous impact on human health.
The inability of viruses to grow or replicate outside the host cell means they have become masters at persistence within the host. Viruses persist within the host cell because they are often able to replicate without killing the host cells, their gene expression can be restricted, they can mimic host molecules, down-regulate host immunity and directly infect the host’s immune cells. Viruses continuously change, either gradually (called ‘drift’) where they accumulate minor mutations, or suddenly (called ‘shift’) following major changes during recombination of the viral genome.
RNA viruses such as measles and human immunodeficiency virus (HIV) are unstable, undergoing immense drift and shift with up to 2% of their genome altered each year through multiple mutations. These viruses tend to cause systemic disease in humans, leading to generalised cutaneous eruptions such as a ‘viral exanthem’. In contrast, DNA viruses such as human papillomavirus (HPV), molluscum contagiosum, herpes simplex virus (HSV), and varicella zoster virus (VZV) are more stable. They are frequently inoculated directly into the skin and replicate in epidermal cells.
Viruses can be transmitted by direct contact from skin to skin, through aerosols, transplacental spread, blood products, contaminated needles and via the faecal–oral route. Once inside the host, viruses can spread directly from cell to cell, via the blood, or central nervous system by axonal transport. Many viruses demonstrate tropism (in other words a predilection for a certain host cell) via virus attachment to protein-specific cell surface receptors. HPV, for example, has tropism for keratinocytes.
The behaviour of different viruses therefore determines the type of disease they cause with resultant localised or widespread reactive skin disorders. Common viral infections of the skin are usually easily identified by pattern recognition through the characteristic skin or mucous membrane site affected and/or typical lesions.
Herpes viruses
Herpes simplex
HSV is spread by direct contact—‘shedding’ from one host to another. Two viral subtypes exist: type I is associated mainly with facial lesions although the fingers (Figure 14.1) and genitals may be affected. Type II is associated almost entirely with genital infections. HSV remains within the host for life, remaining latent in the sensory nerve ganglia leading to recurrent reactivation.

Figure 14.1 Inoculation herpes.
Primary herpes simplex (type I) infection usually occurs in or around the mouth/nose, with variable involvement of the face (Figure 14.2). Lesions consist of small vesicles (Figure 14.3) which crust over and are associated with regional lymphadenopathy. HSV type II infects the external genitalia; the initial vesicle or vesicles rapidly break down into painful ulcers (Box 14.1).

Figure 14.2 Herpes ‘cold sore’.

Figure 14.3 Herpes simplex vesicles on posterior pinna.
Box 14.1 Herpes simplex—points to note
- Genital vesicles may not be visualised as they rapidly ulcerate.
- Prodrome symptoms consist of itching, tingling and tenderness.
- Rapid viral detection from scraping the vesicle/ulcer base using electron microscopy, immunofluorescence or PCR.
- Genital herpes in pregnancy carries a risk of ophthalmic infection of the infant. Caesarean section may be indicated.
- ‘Eczema herpeticum’ occurs in patients with atopic eczema where the HSV disseminates across abnormal skin (Figure 14.4).

Figure 14.4 Eczema herpeticum.
Episodes of reactivation of HSV may be triggered by the cold (‘cold sore’), bright sunlight, trauma, immunosuppression or intercurrent illnesses. There is frequently a prodrome of tingling or itching before the appearance of the vesicles, which occur in the distribution of a sensory nerve. Topical aciclovir/penciclovir/idoxuridine cream can be used to treat mild labial herpes. Severe infections should be treated with oral aciclovir 200–400 mg five times daily for 5 days. Secondary prophylaxis for frequent reactivation can be given as 400 mg once or twice daily. Higher doses are needed in immunocompromised patients. Valaciclovir (HSV 500 mg twice daily for 5 days, VZV 1 g three times daily for 7 days) and famciclovir (genital HSV 250 mg three times daily for 7 days, VZV 750 mg daily for 7 days) are alternatives that are taken less frequently. Brisk inflammatory responses to genital HSV can be seen in patients with HIV whose immune system is reconstituting once they start their HAART (highly active antiretroviral therapy)—the so-called immune reconstitution inflammatory syndrome (IRIS). Clinically, this is seen as deteriorating signs and symptoms of HSV disease and may warrant aggressive treatment of the HSV and occasionally a reduction in the HAART medication.
Varicella zoster virus
VZV is a herpes virus that causes chicken pox (the primary illness), which is characterised by a prodromal illness for about 2 days followed by crops of papular-vesicular lesions (Figure 14.5) that eventually crust over and heal. Subsequently shingles (reactivation) may occur as the virus remains latent in the sensory nerve ganglia (Box 14.2). The thoracic nerves are most commonly affected. In shingles, pain, fever and malaise may precede the rash which is characterised usually by its dermatomal distribution (Figure 14.6); however, adjacent dermatomes may be affected (Figure 14.7). Erythematous papules usually precede vesicles which develop over several days, crusting as they resolve, often with secondary bacterial colonisation. Occasionally, peripheral motor neuropathy can result and a proportion of patients develop severe chronic postherpetic neuralgia. Skin lesions of shingles and nasopharyngeal secretions can transmit chicken pox to susceptible individuals.
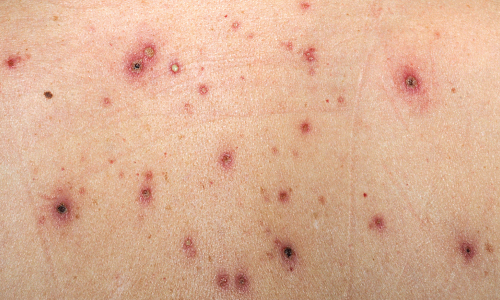
Figure 14.5 Varicella zoster virus chicken pox infection in an adult.

Figure 14.6 Herpes zoster in a dermatome (shingles).

Figure 14.7 Multidermatomal varicella zoster virus (shingles).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








