Vesicular Palmoplantar Eczema: Introduction
|
Vesicular palmoplantar eczema is a dermatitis of the hands and feet characterized by small to large blisters clinically and spongiotic vesicles histologically. It can manifest as either an acute or a chronic dermatitis, or both. Because clinical and histologic presentations of the variants of hand dermatitis, including vesicular palmoplantar eczema, often overlap, making a precise diagnosis can be difficult. For example, patients with pompholyx, the most acute form of vesicular palmoplantar eczema, have been noted to have higher incidence rates of both atopy and contact dermatitis than controls.
With the preceding caveat in mind, vesicular palmoplantar eczema can be divided into four categories: (1) pompholyx, (2) chronic vesiculobullous hand dermatitis, (3) hyperkeratotic hand dermatitis, and (4) id reactions (see Chapter 17). These conditions can be grouped under the category of endogenous hand dermatitis, in contrast to dermatitis clearly caused by exogenous factors such as contact allergy or irritation.
Pompholyx is a term best reserved for acute explosive outbreaks of small to large vesicles and bullae on the palms and soles. It tends to occur more often in the spring and fall, and may be associated with stress. Other etiologic factors are less well established. Cheiropompholyx and podopompholyx are terms occasionally used to describe cases affecting the palms or soles, respectively. Chronic vesiculobullous hand dermatitis, also known as dyshidrotic hand eczema or dyshidrotic hand dermatitis, is usually characterized by small vesicles on the lateral aspects of the fingers. “Dyshidrosis,” a dysfunction of the sweat gland, was long postulated to be a cause, but its role has been subsequently disproved. However, the terminology persists and is commonly used. A third category is chronic hyperkeratotic hand dermatitis, an entity that generally occurs on the central palms. Unlike the other classifications of vesicular palmoplantar eczema, vesicles do not dominate the clinical presentation. However, the spongiosis observed histologically is indistinguishable from the other categories. An id reaction is a vesiculobullous dermatitis, generally appearing on the lateral aspects of the fingers, elicited by an infection elsewhere in the body. The most common cause is a fungal infection. Treatment of the underlying causative factor usually leads to resolution. Endogenous hand dermatitis can be exacerbated by exogenous factors, most notably irritant dermatitis and allergic contact dermatitis. In addition, atopy may in some cases predispose to the development of vesicular palmoplantar eczema.
Epidemiology
Differences in classification and definition have made it difficult to assess the true incidence of the endogenous hand disorders. Most studies have focused on the prevalence of exogenous hand disorders as seen in occupational settings. Pompholyx is the least common presentation of hand dermatitis; in one population study, the 1-year prevalence of pompholyx was estimated to be 0.5%.1 In the same study, hyperkeratotic hand dermatitis represented 2% of all hand dermatoses.1 Other studies have noted prevalence rates ranging from 1% to 5%, with the variation in the frequency of vesicular hand eczema attributable in part to the lack of a common condition.2,3,4
Etiology and Pathogenesis
With the exception of the id reaction, a direct cause of vesicular palmoplantar eczema is rarely identified. A number of etiologic factors have been associated with pompholyx, including atopy (see Chapter 14), contact allergy (see Chapter 13), psychological stress, and hot weather.1 Pompholyx has also been reported after ingestion of piroxicam,5 after ingestion of certain metals in predisposed or sensitized patients most commonly nickel, cobalt, and chromate5 and after intravenous immunoglobulin therapy, with 39 cases reported to date.6,7 There has also been a report of five cases of photo-induced pompholyx in patients with a reported history of photo-induced disease that was reproduced when the patients were phototested with an ultraviolet A (UVA) source.5 Histologic evaluation confirmed the diagnosis of pompholyx and a true photosensitivity rather than photoaggravation. Additionally, there has been evidence of association of vesicular hand eczema following dermatophytid from tinea pedis.8 In a study of 398 patients with hand eczema, those with culture positive tinea pedis were found to have an increased relative risk of 3.58 (p < 0.05) for vesicular hand eczema.9
Exacerbating Factors
Contact allergy is common in patients affected with vesicular palmoplantar eczema, especially the chronic type, but the causal relationship is not always clear. There are cases in which contact allergy has exacerbated preexisting hand dermatitis and also reports that ingestion of certain metals, including nickel, cobalt, and chromium, have caused flares. However, in other cases, the causal relationship may be the reverse. The skin’s impaired barrier function in vesiculobullous hand dermatitis (see Chapter 47) may in some cases lead to sensitization and a higher prevalence of contact dermatitis in the affected population. Investigations into the role of atopy (see Chapter 14) have yielded mixed results. Some studies have shown levels of personal or familial atopy as high as 50% in affected subjects, compared to 11.5% of controls, but other studies have demonstrated no difference in the prevalence in people with vesiculobullous hand dermatitis versus controls.10
Clinical Findings
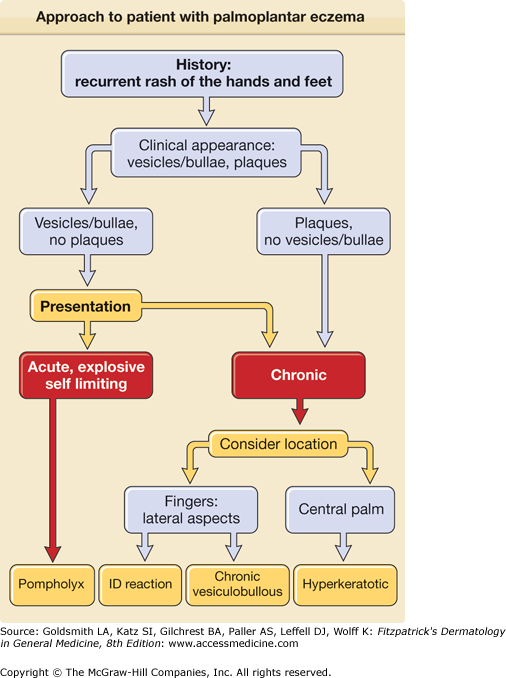
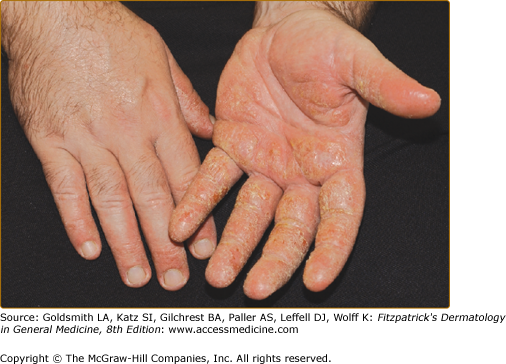
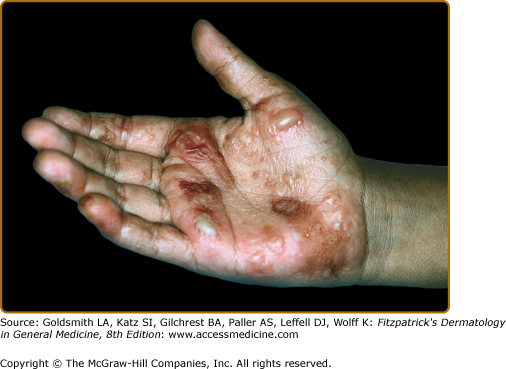
Figure 16-1 is an algorithm showing the approach to the patient with vesicular palmoplantar eczema. Pompholyx can even be severe enough to necessitate hospitalization. In true acute pompholyx, there is an explosive outbreak of deep-seated vesicles on the palms, the lateral aspects of the fingers (Fig. 16-2), and sometimes the soles, usually in a symmetric pattern. Discomfort and itching usually precede the development of the blisters, which have been described as having a “tapioca” appearance (see Fig. 16-3). Blisters may coalesce then desiccate and resolve without rupture (Fig. 16-4). Intact, large blisters can be drained, but should not be unroofed. However, large blisters may rupture spontaneously, leaving oozing or dried up erosions (Fig. 16-5).
This acute phase is generally followed by desquamation of the affected areas. Individual outbreaks are usually self-limited over 2–3 weeks, although they may recur. Secondary bacterial infection is common, often resulting in a local cellulitis, and can sometimes potentiate the development of lymphatic damage, resulting in lymphedema. Attacks are most common among adolescents and young adults and seem to be more common in the spring and summer months. Outbreaks have been shown to be associated with dermatophyte infection, contact dermatitis, in particular cosmetic and hygiene products, metals and internal reactivation from drugs, foods, or metals.
Chronic vesiculobullous hand dermatitis is more common than pompholyx and more difficult to manage because of its relapsing course. The clinical presentation includes small 1- to 2-mm vesicles filled with clear fluid localizing to the lateral aspects of the fingers, palms, and soles as in pompholyx (see Fig. 16-3). As the condition becomes more chronic, the clinical appearance may evolve and subsequently appear more fissured and hyperkeratotic (as in Figs. 16-2 and 16-6). A clear history of vesicles or exacerbations characterized by blistering may help to narrow the classification of a given presentation of hand dermatitis.
Patients with hyperkeratotic hand dermatitis are usually male and generally present with chronic keratotic pruritic plaques, sometimes with fissures on the central palm (see Fig. 16-6). This condition may be the end result of contact allergy, excoriation, and irritation, but generally the cause is not identifiable, and contact allergy does not seem to play an important role. This hand dermatitis commonly occurs in middle-aged to elderly men and is often very refractory to treatment. Friction in lichen simplex chronicus may be an important factor in some cases. Plantar involvement is present in a minority of cases.
(See Chapter 17)
In an id reaction, erythematous vesicles usually are seen on the lateral aspects of the fingers and the palms and are typically pruritic (Fig. 16-7). This eruption of vesicles is usually sudden and classically occurs in response to an intense inflammatory process, especially fungal infections, taking place somewhere else on the body. The id reaction is thought to be an allergic reaction to fungi or to some antigen created during inflammation. Treatment of the underlying infection results in resolution.
Laboratory Findings
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree