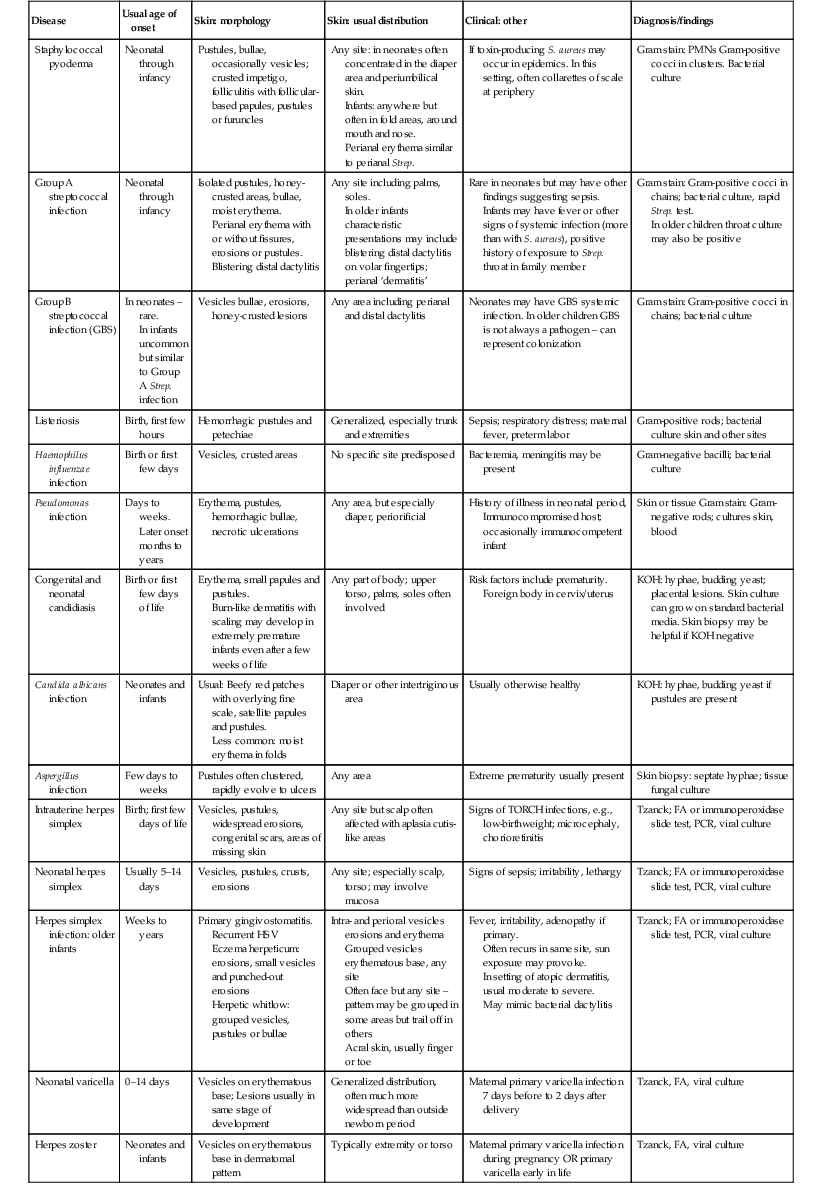
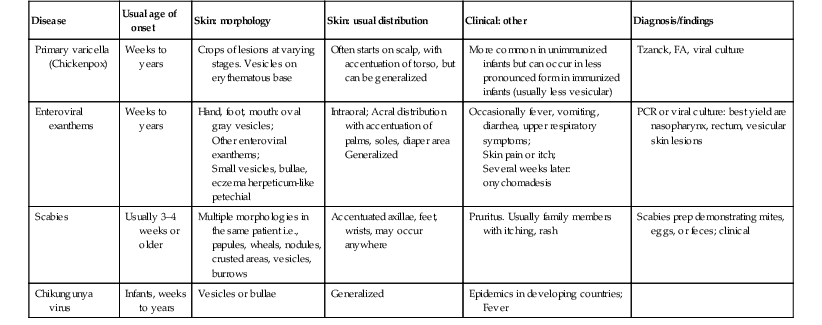
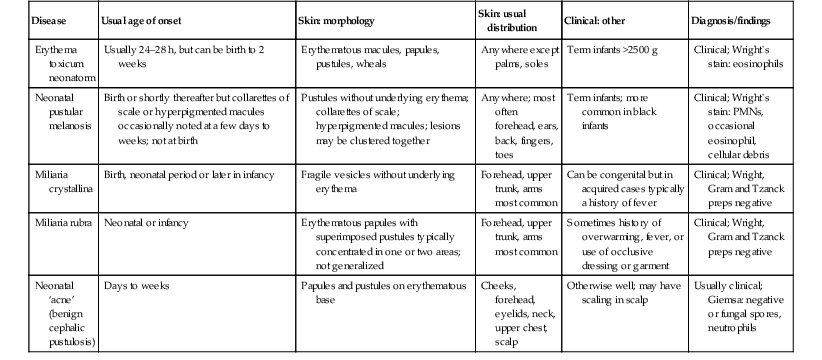
Renee M. Howard, Ilona J. Frieden Vesiculopustular and bullous disorders are common in the neonatal period and the first years of life. Accurate and prompt diagnosis is essential because some conditions that present with blisters and pustules are truly life-threatening. In contrast, many others are innocuous and self-limited; misdiagnosis of a more serious condition can lead to iatrogenic complications, unnecessary expense, and parental anguish. The causes of blisters and pustules in newborns and young infants are influenced by the clinical setting, including geography and whether patients are seen in a hospital or clinic. Infection is the most common etiology in developing countries. In a study of neonates in India with blisters and pustules, bacterial infection was the most common overall, whereas erythema toxicum was the most prevalent non-infectious etiology.1 In a prospective study of newborn inpatients in California examined by pediatric dermatologists, the most common eruption in newborns was erythema toxicum.2 In a retrospective European study done in a Level 3 nursery, vesicles and pustules were the sole reason for admission to the Neonatal Intensive Care Unit (NICU) in 29.8% of infants admitted because of skin lesions.3 Several articles have reviewed an approach to infants with these cutaneous findings,4–6 including infants with hemorrhagic vesiculopustules.7 There is also considerable overlap with the subject matter in other chapters of this book, most notably Chapter 7 (Transient Benign Cutaneous Lesions in the Newborn), and Chapters 12, 13 and 14 (Bacterial, Viral, and Fungal Infections, respectively), so the main discussion of specific disorders are discussed therein. Chapter 11 discusses the diagnosis and management of epidermolysis bullosa and other non-infectious causes of bullae, so those conditions are covered in far less detail in this chapter. In addition to a discussion of vesicles, pustules and bullae, this chapter also includes conditions presenting with erosions and ulcerations. Although vesicles, pustules, and bullae are primary skin lesions, they can quickly progress to secondary skin lesions (i.e. erosions and ulcerations). This can occur rapidly or have transpired in utero, such that erosions and ulcerations are the main presenting finding. Examples include staphylococcal scalded skin syndrome, where erythema and skin erosions predominate over blisters, and Pseudomonas skin infection, where pustules rapidly evolve into necrotic ulcers. Because of the wide range of diagnoses discussed in this chapter, there are boxes and tables to help with a systematic approach to evaluation and differential diagnosis. Tables 10.1–10.3 summarize key findings and differential diagnosis of vesiculopustular diseases in newborns and infants, including infectious causes, relatively common transient skin lesions, and uncommon and rare causes of this clinical presentation. Tables 10.4–10.6 summarize these same categories for the differential diagnosis of bullae, erosions, and ulcerations. Box 10.1 lists conditions in neonates where pustules and vesicles predominate, Box 10.2 lists the conditions in neonates where bullae predominate, and Box 10.3 lists conditions in neonates where erosions or ulcerations may predominate. TABLE 10.3 Differential diagnosis of vesiculopustular diseases – Uncommon and rare causes
Vesicles, Pustules, Bullae, Erosions, and Ulcerations
Introduction
Disease
Usual age of onset
Skin: morphology
Skin: usual distribution
Clinical: other
Diagnosis/findings
Acropustulosis of infancy
Birth or days to weeks
Vesicles and pustules
Hands and feet, occasional lesion elsewhere
Severe pruritus accompanying lesions which tend to come in crops
Clinical; skin biopsy: intraepidermal vesicle/pustule
Eosinophilic pustular folliculitis
Birth or days to weeks
Pustules, erythema
Mainly scalp and face; occasionally trunk, extremities
Pruritus; waxing and waning course with recurrent crops
Skin biopsy: dense perifollicular mixed infiltrate with eosinophils
Incontinentia pigmenti
Birth to days
Vesicles, hyperkeratosis in linear array
Most common on trunk, scalp, extremities
Extracutaneous involvement common but often not evident at birth.
Mothers may have history of IP or other findings (e.g., missing teeth, areas of decreased hair growth)
Skin biopsy: eosinophilic spongiosis with dyskeratosis
Gene testing can also be used to establish diagnosis in atypical cases
Neonatal Behçet disease
First week of life
Small punched out vesicles, pustules, ulcerations and scarring
Perioral and oral mucous membranes, hands and feet, occasionally other sites
Maternal history of Behçet disease
Clinical findings and maternal history
Erosive pustular dermatosis of the scalp
Weeks to months
Crusting, pustules, scaly erythema
Scalp, superimposed on areas of alopecia, scarring from scalp injury
Severe scalp edema or necrosis of delivery; similar findings in Hay–Wells and Rapp–Hodgkin ectodermal dysplasias
Clinical findings and prior history of scalp injury or ectodermal dysplasia
Hyper-IgE syndrome
Days to months
Single or grouped pustules, vesicles, or crusting
Face, scalp, upper torso
Blood eosinophilia
Note: IgE levels often become elevated after neonatal period
Skin biopsy: intraepidermal vesicle with eosinophils or eosinophilic folliculitis.
Gene testing for STAT-3 mutation
Lipoid proteinosis
Usually ≥1 year
Erythematous papulovesicular lesions resulting in atrophic scarring
Face, ears, extremities and occasionally trunk
Thickening of the skin, especially lips, perinasal skin, tongue; hoarseness
Skin biopsy shows thick hyalinized material with characteristic PAS-positive staining.
Positive FH in some cases
Pustular psoriasis or deficiency of interleukin-1 receptor antagonist
First weeks or months of life
Pustules generalized, but especially palms, soles; may have underlying erythroderma
Generalized
Irritability, occasionally fever
Skin biopsy: epidermal microabscesses and acanthosis, parakeratosis, dilated capillaries
Pustular eruption of myelodysplasia in Down syndrome/neonatal eosinophilic pustulosis
First few days to months of life
Extensive pustules on erythematous base, often aggregating in areas of skin injury
Face most common site but can occur elsewhere
Very high WBC count: usually in setting of Down syndrome but can occur without obvious Down phenotype or with other causes of severe leukocytosis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

Vesicles, Pustules, Bullae, Erosions, and Ulcerations
10