Competency Versus Performance in Plastic Surgery
Navigating Through New Technologies and Medical Devices
Keywords
• Plastic surgery • Novel technology • Surgeon competence
New methods in plastic surgery: interplay of technology and technique
The practice of plastic surgery combines knowledge of basic and clinical science in addition to development of technical skill. The acquisition of technical and manual skill, however, is closely associated with the use of surgical technology. Learning to use a surgical instrument and applying it appropriately to human tissue is defined as technique. Advances in surgical methods in plastic surgery combine new techniques, new applications of existing techniques, and new medical devices (Table 1). The 1 paramount requirement for successful application of any and all of these 3 modalities is the plastic surgeon’s closest mentor: detailed knowledge of surgical anatomy and physiology.
Table 1 Examples of advancements in plastic surgery methods
Data elucidated from evidence-based research and clinical trials as well as structured technical cases form the building blocks for the clinician to safely extrapolate indications for the use of new or existing technologies to treat existing surgical challenges or address aesthetic concerns. The first reported use of botulinum toxin was in 1980 for the treatment of strabismus and blepharospasm.1 Since then, indications, (albeit some off-label) have grown to include treatment of glabellar frown lines, facial and cervical dystonias, and as of October 2010, migraine headaches as described by multiple authors.2,3 Successful application of botulin toxin for nonsurgical management of migraines helped advance surgeons’ understanding of muscle function alteration and its impact on adjacent nerve structures, and a permanent solution to migraine headaches using transection of the corrugator supercilii muscles, a technique described as part of the classical browlift procedure, was proposed and effectively applied.4
Techniques in microsurgery first developed in 1921 with the indication to surgically repair a labyrinthine fistula of the middle ear. Vascular surgeon Jules Jaconson is credited for the first true microvascular anastomosis, coupling 1.4 mm vessels in 1960. In 1963, this application was extended for replantation of a partially amputated digit, and, in 1966, transfer of a second toe for thumb reconstruction was performed by Dong-yue Yang and Yu-dong Gu in Shanghai, China. Since then, microsurgical techniques have been applied toward peripheral nerve reconstruction by extension of cable grafts, and in microlymphatic surgery in the treatment of chronic lymphedema. With the advent of face transplantation over the last 5 years, this technique has evolved exponentially to something that may have never been conceptualized had it not been for earlier advancements.5,6 The history of microsurgery and teaching of microsurgery at different levels (beginner, intermediate, and advanced) exemplifies the importance of appropriately targeted continuing education and maintenance of skills.
The leukotriene inhibitor Singulair has been used to prevent capsular contracture or hypertrophic scarring, and human growth hormone has been used for its antiaging effects. Nonetheless, off-label use has to be tempered with a thorough knowledge of reported clinical and scientific precedents in the literature. Additionally, the practitioner has to educate the patient, through informed consent, before embarking on off-label uses of approved products. This not only strengthens the bond between physician and patient, but also serves to legally protect the surgeon from intent-to-harm clauses if litigation should ensue.7 Current examples of creative, sometimes off-label application of biomaterials are discussed elsewhere in this issue by Kim and Evans et al.
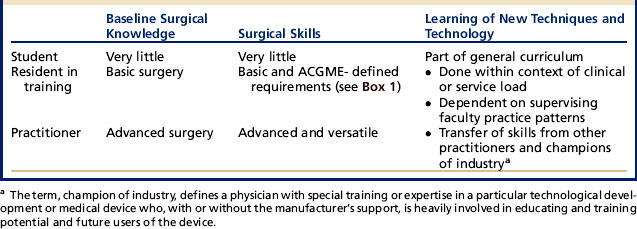
As surgical technology continues to grow, so does the responsibility of plastic surgeons at every level from medical student to independent practitioner, to achieve proficiency in various techniques using new technology. Given the dynamic nature of plastic surgery as a field, continuing medical education (CME) and maintenance of competency have become vital to sustainability in an increasingly regulated and competitive health care arena. In the next section, the authors discuss how knowledge and skill levels are acquired at different levels of training (Table 2) and how independent practitioners maintain high performance and patient safety standards.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree