11. Venous Thromboembolism and the Aesthetic Surgery Patient
Christopher J. Pannucci, Amy Kathleen Alderman
■ VTE is a life- or limb-threatening complication that can occur after surgical procedures.
■ It has been designated by the CDC as the most common cause of “preventable” hospital deaths and has been designated by the Centers for Medicare and Medicaid Services as a “never event” for some surgical procedures.
■ The annual estimate of VTE events is 500,000 cases with 100,000 deaths in the United States.
■ VTE occurs in 18,000 plastic surgery patients a year, and, although this may seem rare, it can be particularly devastating when it occurs in elective aesthetic surgery patients.
■ Surgeons should consider patients’ VTE risk as part of the standard aesthetic surgery workup.
■ Although research in plastic surgery patients has clearly demonstrated that all VTEs are not preventable, surgeons can minimize VTE risk preoperatively, intraoperatively, and postoperatively.
WHAT DO THE GUIDELINES SAY?
■ Both the American Society of Plastic Surgeons (ASPS) (2012) and American Association of Plastic Surgeons (AAPS) (2016) have published evidence-based consensus statements on VTE risk stratification and prophylaxis.1,2
■ Both sets of recommendations advocate for individualized VTE risk stratification using the 2005 Caprini Risk Assessment Model (RAM).3
■ Both sets of recommendations recommend different VTE prevention strategies based on baseline VTE risk, characterized by Caprini score and by procedure type.
• A “one size fits all” approach is not recommended
SUMMARY OF CURRENT GUIDELINES
■ The ASPS VTE Task Force1 makes recommendations for aesthetic surgery patients who have surgery under general anesthesia. Direct quotes are provided from their 2012 manuscript.
• Risk stratification: “Should consider completing a 2005 Caprini RAM…to stratify patients into a VTE risk category based on their individual risk factors”
• For elective surgery patients with Caprini scores of ≥7: “Should consider utilizing risk reduction strategies such as limiting OR times, weight reduction, discontinuing hormone replacement therapy, and early postoperative mobilization”
• For body contouring or abdominoplasty under general anesthesia with procedure time >60 minutes:
► Caprini score 3-6: “Should consider the option to use postoperative low-molecular weight heparin or unfractionated heparin”
► Caprini score ≥3: “Should consider the option to utilize mechanical prophylaxis… for nonambulatory patients”
► “Should strongly consider the option to use extended (duration) low-molecular-weight heparin postoperative prophylaxis”
■ The AAPS published a systematic review/meta-analysis and consensus panel on DVT/PE prevention in 2016. Source data were largely derived from inpatient surgery, but several recommendations were applicable to the aesthetic surgery population.2 Direct quotes are provided from their manuscript.
• “We recommend using nongeneral anesthesia when appropriate. When possible, consideration should be given to using monitored anesthesia care, local anesthesia with sedation, or neuraxial anesthesia instead of general anesthesia.”
• “We recommend using intermittent pneumatic compression to prevent perioperative VTE events in plastic surgery patients…intermittent pneumatic compression is superior to elastic compression stockings.”
• “We recommend all plastic and reconstructive surgery patients should be risk stratified for perioperative VTE risk using a 2005 Caprini score.”
• “We do not recommend adding chemoprophylaxis to intermittent pneumatic compression for VTE prophylaxis in the general non-risk-stratified plastic surgery population.”
• “We recommend that surgeons consider chemoprophylaxis on a case-by-case basis in patients with Caprini score >8.”
• “We do not recommend adding routine chemoprophylaxis for VTE prophylaxis in non-risk-stratified patients undergoing…body contouring.”
UNDERSTANDING THE CAPRINI RISK ASSESSMENT MODEL3
■ This is a VTE risk assessment model that has been validated in >20,000 patients, including plastic, general/vascular/urology, gynecology oncology, and otolaryngology/head and neck.
■ The Caprini RAM is a one-page questionnaire that is easy to complete at either the patient’s initial consultation or preoperative visit (Fig. 11-1).
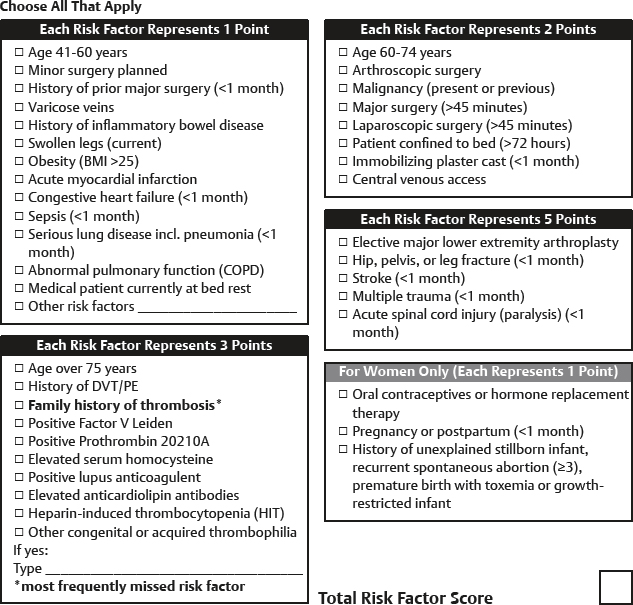
Fig. 11-1 Caprini risk assessment model.
• Assigns different point values for the various risk factors based on the patient’s personal medical history and family history.
• An aggregate risk factor score is generated and correlates with a percentage value for postoperative VTE risk.
• Using this information, physicians can make a decision about chemoprophylaxis an other risk-reduction strategies.
■ Current recommendations support the use of the 2005 Caprini RAM and not the 2010 Caprini RAM, which places more patients in a higher-risk category but does not increase the sensitivity of predicting VTE.4
WHAT AESTHETIC SURGERY PATIENTS ARE AT HIGHEST RISK?
■ Among cosmetic procedures, abdominoplasty alone or in combination with another procedure has the highest risk of VTE. The procedure type with the greatest risk is circumferential abdominoplasty, which has an associated VTE frequency of 3.40%.5
■ The Doctors Company has seen an increase in malpractice claims involving VTE, and a major issue is inadequate prophylaxis in high-risk patients.
• In a review of 12 claims, 8 were abdominoplasty cases (6 of those 8 were combined procedures). Half of all patients had general anesthesia, the other half had IV sedation. Death occurred in 9 patients.
■ Why is the risk of VTE increased with abdominoplasty?
• Multifactorial. Contributing causes include length of procedure (venous pooling with general anesthesia), prone positioning for hip liposuction (increased venous pressure from hip roll), fluid shifts with liposuction, increased intraabdominal pressure from rectus plication, flexed posture and postoperative abdominal binder,6 and decreased postoperative mobility.
WHAT CAN BE DONE BEFORE SURGERY—RISK STRATIFICATION
■ Complete a full history and physical examination and a VTE risk assessment tool such as the 2005 Caprini RAM. This tool reminds surgeons to ask about family history of VTE (the most commonly missed risk factor), genetic hypercoagulability, and current estrogen usage, among other often missed risk factors.
• Studies among plastic surgery inpatients7 and surgical outpatients8 have identified an 18- to 20-fold variation in VTE risk among the overall surgical population.
• Individualized risk stratification allows surgeons to conceptualize and quantify this risk.
NOTE: No VTE risk stratification tool has been validated for aesthetic surgery patients.
■ Data from plastic surgery inpatients not given chemoprophylaxis can be used to estimate VTE risk.9
• Caprini 3-4: 0.32% 60-day VTE risk
• Caprini 5-6: 1.22% 60-day VTE risk
• Caprini 7-8: 2.55% 60-day VTE risk
• Caprini >8: 8.54% 60-day VTE risk
■ If a risk stratification tool is not used, risk estimate based on procedure type can be provided and discussed during the informed consent process.5,10,11
• Circumferential abdominoplasty: 3.4%
• Abdominoplasty with intraabdominal procedure: 2.1%
• Abdominoplasty with concomitant procedure: 0.67%
• Abdominoplasty alone: 0.34%
• Breast augmentation: 0.02%
• Facelift: 0.02%
■ Preoperative hematology consultation can be considered if patients have family member(s) with VTE or other notable risk factors.12
• Hypercoagulability testing can be affected by many drugs and clinical circumstances.
• Hypercoagulability testing is best ordered and interpreted by a hematologist.
• Hematologists can help to estimate level of VTE risk and can make recommendations for VTE prevention strategies in high-risk patients.
• Aesthetic surgery is elective and can be delayed until the entire workup is complete.
WHAT CAN BE DONE BEFORE SURGERY—RISK MODIFICATION
■ Many patient-level risk factors are potentially modifiable before surgery.3
• BMI, presence of central line or chemoport, use of estrogen-based contraceptives, among others
• Encourage patients to lose weight, have a general surgeon remove a chemoport, wait at least 30 days between procedures, and hold estrogen products and tamoxifen for 3-4 weeks before surgery—all of these examples of risk modification will theoretically decrease VTE risk.13
► Help patients to understand that their safety is the principal concern.
■ Studies have associated increased number of surgical procedures and increased length of surgery with higher risk for VTE.5,14–16 The two are related, and the driving force is unknown.
• Limiting number of concurrent procedures, and thus operative time, is a modifiable risk factor.
► Aesthetic surgeons need to be aware that they often combine procedures more than any other surgical specialty for patient convenience (single recovery), expedited patient gratification, competitive market forces, and patient costs.
► ≤6 hours should be the targeted length of aesthetic surgery.
◆ ASPS has recommended: “Ideally, office procedures should be completed within 6 hours…this might involve staging multiple procedures into more than one case.”17
◆ Surgeons should be aware of state-based surgical time and liposuction volume limits on office-based surgery.
• For example, compared with abdominoplasty alone, abdominoplasty plus intraabdominal procedure has 6× increased risk (0.34% versus 2.17%), and abdominoplasty plus other procedure has 2× increased risk (0.34% versus 0.67%).5
• In another example, Tracking Operations and Outcomes for Plastic Surgeons (TOPS) and CosmetAssure data suggested that among those having combined procedures, the risk of VTE increases fivefold among those having breast augmentation and 30% for those having an abdominoplasty, compared with single procedures.10
■ Plastic surgery tourism can increase risk for VTE
• Screening duplex ultrasound before and after long flights in economy class showed that 4.9% of people developed deep or superficial thrombosis during flight.
• The clinical relevance of these asymptomatic DVTs is unclear.
• Below-knee elastic compression stockings significantly decreased DVT rate from 4.5% to 0.24%.18
• Systematic review of air travel and VTE showed that elastic compression stockings, but not aspirin or low-molecular-weight heparin, prevented DVT.19
■ For patients at very high risk, the decision to perform a surgical procedure is the last consideration in risk modification.
• Surgeons may deem some patients’ VTE risk as too high to safely offer an aesthetic procedure.
WHAT CAN BE DONE DURING SURGERY—RISK REDUCTION
■ Type of anesthesia is a modifiable risk factor in the intraoperative setting.
• General anesthesia increases risk, compared with other anesthesia types.
• VTE with abdominoplasty is significantly higher among patients having general versus IV sedation (OR: 0.11, CI: 0.03-0.43).20
► Cause is probably loss of calf muscle pump and resultant venous stasis, as well as other mechanisms.
• Nongeneral anesthetic, when feasible for surgeon and patient, is preferred and safer.
■ Mechanical prophylaxis options include elastic compression stockings and intermittent pneumatic compression.
• Elastic compression shunts blood from the superficial to deep systems and minimizes stasis.
• Use of stockings is more effective than nonuse in prevention of VTE.21
• Intermittent pneumatic compression physically pumps blood from caudal to cranial, re-creating the action of the calf muscle pump, and activates the body’s endogenous fibrinolytic mechanism.22
• The AAPS consensus statement recommended intermittent pneumatic compression as superior to elastic compression stockings.2
■ Slight knee flexion (5 degrees) on a pillow can promote venous egress.
■ Abdominal wall plication and bed flexion during abdominoplasty increases intraabdominal pressure.6,23 This may cause inferior vena cava and femoral vein stasis, predisposing to DVT.
• Surgeons should plicate only when clinically necessary, and not as a matter of course.
WHAT CAN BE DONE AFTER SURGERY—RISK REDUCTION
■ Early ambulation and adequate hydration are critical.
■ Postoperative abdominal binders and compression garments can constrict the common femoral vein in the thigh and may require modification.24,25
■ Mechanical prophylaxis (intermittent pneumatic compression) can be used to mimic the calf muscle pump after surgery, at least until patients are ambulatory.
• There are no data on VTE risk reduction with postdischarge mechanical prophylaxis.
• Chemoprophylaxis, including unfractionated heparin and enoxaparin/low-molecular-weight heparin, has been studied extensively among plastic surgery inpatients.
► For inpatients, enoxaparin prophylaxis provided for the duration of inpatient stay reduced VTE risk among high-risk patients (Caprini scores of 7-8 and >8), but not in lower-risk patients (Caprini scores of 3-4 and 5-6).9
► For inpatients, postoperative enoxaparin prophylaxis did not significantly increase bleeding risk.26
► Despite the injectable delivery, enoxaparin is well tolerated among aesthetic surgery patients and is affordable.
► Preoperative or intraoperative chemoprophylaxis significantly increases bleeding risk in body contouring27 and facelift28 surgery.
► Providing chemoprophylaxis to all patients may have an unfavorable risk/benefit relationship.2
◆ The ASPS and AAPS recommend prophylaxis based on Caprini scores as opposed to all patients.
■ Some surgeons use oral Factor Xa inhibitors for chemoprophylaxis.
• Limited data exist, and, presently, oral Factor Xa inhibitors are not FDA approved for prophylaxis in nonorthopedic surgery patients.
• In abdominoplasty patients, oral Factor Xa inhibitors have low rates of reoperative hematoma (2.3%), but no studies on effectiveness have been published.29
■ Current guidelines explicitly recommend against aspirin as a single-agent chemoprophylaxis for VTE.30
■ Screening duplex ultrasound for all patients, instead of other mechanical and pharmacologic means of prophylaxis, has been recommended.31
• Among 200 aesthetic surgery patients, the rate of asymptomatic DVT was 0.5%.
SENIOR AUTHOR TIP: I strongly disagree with this practice of screening via duplex ultrasound when performed instead of other mechanical and pharmacologic means.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




