and Peter M. Prendergast2
(1)
Elysium Aesthetics, Bogota, Colombia
(2)
Venus Medical, Dublin, Ireland
History
The use of ultrasound in surgical procedures is not new. Kelman introduced phacoemulsification for cataracts in 1967 after being inspired by his dentist’s ultrasound device for descaling [4]. Since then, ultrasound has been used extensively in neurosurgery for selective destruction of tumors and in general surgery, particularly for cutting and coagulating during laparoscopic surgery [5]. In the late 1980s and early 1990s, Scuderi and Zocchi pioneered the application of ultrasound for selective emulsification and removal of fat for body contouring [6–8]. The first-generation ultrasound-assisted lipoplasty device was developed by SMEI Company in Italy. SMEI’s sculpture consisted of large 4–6 mm solid probes that emulsified fat at a frequency of 20 kHz. In the mid-1990s, two second-generation ultrasound-assisted lipoplasty devices were introduced. Lysonix 2000 (Lysonix Inc., Carpenteria, CA) featured hollow ultrasonic cannulae of 4.0 and 5.1 mm diameter. Fat emulsification and aspiration occurred simultaneously through the golf-tee and bullet-design cannulae at a frequency of 22.5 kHz. During the same period, Mentor Corporation introduced their Mentor Contour Genesis device. This employed 3.0 and 5.1 mm hollow cannula at a frequency of 27 kHz. Excessive ultrasound delivery to the tissues with these devices compounded with the elimination of protective wetting solution due to simultaneous aspiration during ultrasound delivery resulted in significant complications [9–11]. The popularity of ultrasound-assisted lipoplasty dwindled in the late 1990s. In 2001, Sound Surgical Technologies introduced a third-generation device that was designed to improve safety by reducing the power delivered to the tissues while maintaining efficacy. The smaller-diameter solid probes (2.2–4.5 mm) and unique grooved tip design emulsify fat efficiently at 36 kHz while preserving surrounding tissues and structures. The tunable nature of the system allows almost all body areas to be treated safely and effectively [12]. VASER® is currently the gold standard for use in high-definition body contouring. Figure 6.1 shows the difference between the smaller-diameter VASER® probes and the previous-generation large-diameter hollow cannula.


Fig. 6.1
A comparison of the third-generation VASER solid probes and the Lysonix 2000 hollow ultrasonic cannula
VASER® technology is fairly different from previous generations of ultrasound in the sense of better results and less complication rates. The key is in how it works: the resonance. Resonance is a physical effect seen in nature. It is not a laboratory reaction or an invention. The main description of what resonance is lies in music. Famous singers like Ella Fitzgerald were known for reaching a specific note breaking glass. How could a simple wave of sound do that? There is a specific frequency of natural vibration. The glass and other materials have a vibration frequency in which they start vibrating by themselves, increasing the vibration in a logarithmical way until reaching a break point.
The concept of resonance in VASER® is based in two notions: One is that the frequency of the VASER® (36 mHz) is closest to the resonance of fat. While fat vibrates, it gets emulsified with less power delivered. The second notion is the cell size: comparatively, the fat cells are ten times bigger than the other cells around (blood vessels, nerves, connective tissue), making fat more sensitive to the ultrasonic energy than the other tissues.
Principles of UAL and VASER
Vibration amplification of sound energy at resonance (VASER®) is a third-generation of ultrasound-assisted liposuction (UAL) that uses ultrasonic energy as a means to eliminate fat. Ultrasound technology emulsifies the fat for removal in such a delicate way that preserves as much of the tissue matrix as possible while emulsifying the desired amount of fatty tissue [3].
Third-generation ultrasound-assisted lipoplasty (UAL) requires three main steps: infiltration of tumescent fluid, emulsification of adipose tissue with solid probes, and aspiration of the fatty emulsion. The solid metal probes are made to vibrate at ultrasonic frequencies (above 20 kHz) in order to induce their effects on the subcutaneous fat. The basic physics of UAL, tissue interactions, and advantages of third-generation UAL in high-definition body sculpting are described in this section [3].
The UAL system comprises an electronic generator and an ultrasonic handpiece. Within the handpiece, electrical energy is converted to mechanical energy in the form of vibration through a piezoelectric transducer. This vibratory motion is channeled through the handpiece to the attached titanium probe. As such, the metal probe is made to vibrate at ultrasonic frequencies; this is 36 kHz with the VASER® system. At this resonant frequency, probes of certain lengths vibrate longitudinally with the handpiece. The forward and back movement of the probe is maximal at the tip where energy is focused. Although the displacement of the tip of the probe is only in the order of microns, it is sufficiently powerful to exhibit its effects on the surrounding tissues. By increasing the amplitude on the generator, the displacement becomes greater and the power increases. It is the interaction of the tip of the probe with the surrounding tissues that determines the efficacy of the system. The unique grooved design of the VASER® probes plays a significant role in the coupling of power to the tissues.
The tissue interaction between titanium ultrasonic probes and wet adipose tissue that leads to disruption and emulsification can be broadly divided into three mechanisms: cavitation, mechanical, and thermal [3, 13]. Although it is not certain which mechanism prevails, it is likely that cavitation and mechanical disruption of the adipose tissue are important, whereas thermal destruction of fat is undesirable and may lead to burns. Cavitation occurs when microscopic air bubbles in the tumescent fluid surrounding fat expand due to the compressive and rarefactive forces caused by the vibrating ultrasonic probe (Fig. 6.2). The bubbles (not the adipocytes) get larger and larger until they finally implode, releasing energy that disrupts the adipocytes from their architectural support within the lobules. The fat cells themselves do not burst or implode. It is important to remember that the cavitation process occurs close to the tip of the probe, in a halo region within a few millimeters of it. It does not occur in a spray gun fashion. As such, the probe must pass methodically in every proposed treatment area.
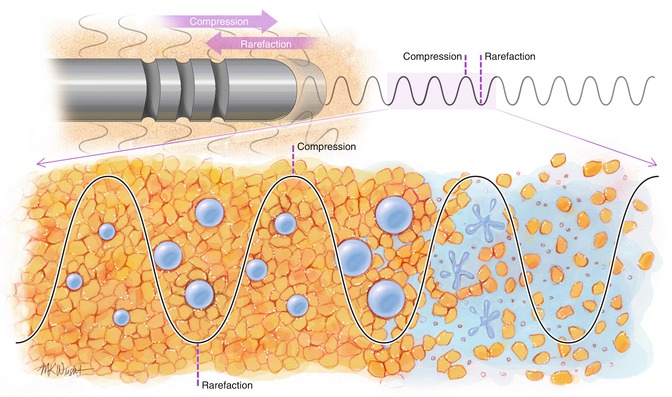
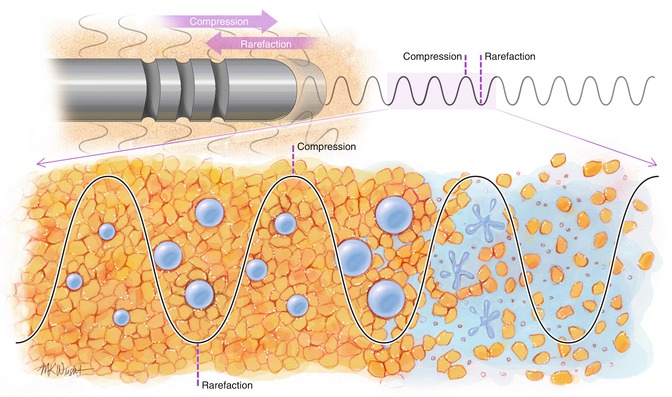
Fig. 6.2
The cavitation effect. The VASER® probes vibrate at ultrasonic frequencies creating compressive and rarefactive forces around the grooved tip. Cavitation microbubbles expand and then implode, releasing energy that disrupts the adipocyte architecture until an emulsion of fat and fluid is formed
Mechanical disruption of fat occurs at the tip of the probe, where the vibrating metal surface comes in contact with the adipocytes. If the probe is not in constant to-and-fro motion within the tissues, the high-frequency vibration begins to heat the tissues. This thermal energy is not the desired mechanism of action of UAL and only serves to increase the incidence of burns and seromas. Cavitation and mechanical disruption of adipose tissue occurs due to the relative fragility of this tissue compared to other tissues such as vessels, muscle, and nerves.
The main advantages of the VASER® third-generation UAL system relate to its safety, smoothness, and ability to treat the superficial tissues. VASER® is safer than previous UAL technologies for a number of reasons. Firstly, solid probes are used so the protective tumescent fluid is not withdrawn during ultrasound delivery to the tissues. Ultrasound energy should never be delivered to dry tissues. Secondly, the probes are smaller in diameter compared to its predecessors. Since the amount of energy delivered to tissues is approximately proportional to the square of the diameter of the probe, narrower probes deliver much less energy and are safer. The efficiency of the narrower VASER® probes is not just preserved but increased due to the grooves at the tip of the probes. The grooves increase surface area and increase coupling with the surrounding tissues. Cavitation occurs in front of as well as to the sides of the grooved tip, increasing efficiency and reducing the amount of total energy required to disrupt a given volume of adipose tissue. Thirdly, ultrasound energy delivered to the tissues is selective for lobules of fat bathed in tumescent solution, such that collateral damage to the tissue matrix, lymphatics, nerves, and vessels is minimized. This translates to an easier recovery for the patient with less bruising, swelling, and pain. The ability to halve energy delivered to the tissues using the pulsed (VASER) mode is important during the very superficial work required for high-definition lipoplasty. Fourthly, the unique vented cannulae and small port holes featured with the VentX design facilitate refined contouring in delicate and superficial tissues and reduce avulsion and trauma to tissues. Finally, VASER®-assisted lipoplasty has shown to reduce blood loss and improve skin retraction compared to suction-assisted lipoplasty [14]. This has important implications in high-definition contouring where large surface areas are often treated in a single procedure and where excellent skin retraction is essential in order to reveal underlying muscular anatomy.
VASER® Lipo System is designed to optimize all phases of the body sculpting procedure. It is a unique technology that maximizes fat extraction without compromising comfort and safety of their patients.
As the technology is based on pulsed energy delivery and specialized probe designs, we need to know the different fatty tissues and some other technical aspects to actually understand why VASER® is by now the gold-standard in liposculpture.









