FIGURE 4–1 Anatomy of the arterial and venous circulatory systems The circulatory system consists of the cardiac, arterial, venous, and lymphatic systems. The arterial system is further delineated into the macrocirculation (arteries large enough to be named) and microcirculation (capillaries and arterioles too small to be named). The lymphatic system is illustrated in Chapter 5.
Vascular diseases such as peripheral arterial occlusive disease (PAOD) and chronic venous insufficiency (CVI) cause the majority of lower extremity wounds; the majority of arterial wounds are caused by PAOD. The clinical spectrum of PAOD ranges from asymptomatic disease to mild claudication, to tissue loss or gangrene of the foot or lower extremity. When patients with PAOD have an ulcer or gangrene of the lower extremity, it is termed critical limb ischemia (CLI). The major cause of CLI is a reduction in distal tissue perfusion below the resting metabolic requirements usually associated with atherosclerosis; however, other conditions may cause wounds that appear to be arterial or ischemic. (TABLE 4-1) Diabetes mellitus (DM) is one of the most serious and prevalent of these disorders. The combination of DM and PAOD may lead to foot ulceration or gangrene, which may result in amputation. The overall risk of amputation is 15 times higher for patients with DM than in those without diabetes. The reason for the increased amputation rate is related to the complex pathophysiology of neuropathy and ischemia in the diabetic foot.1
TABLE 4-1 Differential Diagnosis of Lower Extremity Wounds
The pathologies listed in this chart can cause wounds that appear similar to wounds caused by peripheral arterial occlusive disease. Making the correct differential diagnosis is imperative because treatment of the underlying disorder is the first step toward successful wound healing. Some of these disorders are discussed further in Chapter 8.
The presence of any lower extremity wound requires an evaluation of vascular status since it will determine the ability of the wound or surgical incision to heal. Healing of a foot wound may take months despite undergoing revascularization procedures. The presence of CLI in a patient is significant not only for potential limb loss; it is also an independent risk factor for cardiovascular morbidity and mortality. The goal of taking care of these patients is to assure that the maximum amount of arterial perfusion is present to help in the healing of these wounds. There is a high rate of recidivism and subsequent amputation when the treatment of the vascular insufficiency is not performed in a timely manner.
ARTERIAL WOUNDS
Epidemiology
An estimated 10 million people in the United States, and 27 million people in North America and Europe, suffer from PAOD.2 As the population ages, the prevalence of PAOD will increase to approximately 25% for individuals more than 80 years of age.3 The true incidence of CLI is unknown; however, some studies have estimated around 500,000 to 1 million new cases occur each year.4 A similar incidence of 400 per 1 million population per year was found in a national survey of the Vascular Surgical Society of Great Britain and Ireland.5 The majority of individuals who have CLI with ulceration or gangrene also suffer from DM. It is estimated that up to 70% of all lower extremity amputations are diabetes related and the majority of those patients present with a foot ulcer that develops into an infected limb or gangrene.6,7 Almost 50% of those patients who undergo amputation for CLI will require amputation of the opposite limb within five years.
The economic impact involved in the care of patients with vascular wounds is staggering. The annual costs in treating lower extremity ulcers are around $25 million and the individual cost for treating a foot ulcer can be as high as $28,000.8 In England, the cost of care for an individual with a leg ulcer was around $130,000 annually.9 Included in the estimates are physician visits, hospital admissions for wound debridement or surgical revascularization, rehabilitation, and wound care supplies.
The prevalence of PAOD with intermittent claudication among males and females is between a ratio of 1:1 and 2:1. This ratio increases when an ulcer or gangrene is present to at least 3:1. The prevalence of CLI increases substantially as the population ages.10
The natural progression of CLI is limited since most large studies include performance of some revascularization procedure. However, there are some patients for whom an operation is prohibitive due to multiple co-morbidities or limited life expectancy. A recent study by Marston followed a cohort of patients with CLI who presented with uncomplicated limb ulcers.11 Revascularization was not performed due to medical co-morbidities or anatomic considerations that did not allow surgical intervention. A total of 142 patients were followed for 1 year with the primary endpoint being major limb amputation. During the study, the wounds were treated with a specific protocol that emphasized pressure redistribution, debridement, infection control, and moist wound healing. The limb loss or amputation rate for these patients was 19% at 6 months and 28% at 12 months. Interestingly, complete wound closure was achievable in 25% at 6 months and 52% at 12 months. The only significant factor that affected wound closure was the initial size of the wound.
Arterial insufficiency not only causes wounds, it also portends negatively on the patient lifespan. The most common cause of death in patients with severe PAOD or CLI is coronary artery disease. Depending upon the severity of the CLI, patients with resting pain have more than 70% mortality rate at 5 years. Even though this patient population may have a high mortality rate and are often treated in a palliative manner, conservative care can help alleviate pain and/or heal wounds.
Pathophysiology
Risk Factors The most common causes of PAOD are arteriosclerosis and atherosclerosis. (FIGURE 4-2) Risk factors for the development of these pathologies include age, smoking, diabetes mellitus, hypertension, hypercholesterolemia, dyslipidemia, family history, and obesity. Prevention and treatment of arterial wounds depend upon adequate identification and management of these risk factors.
FIGURE 4–2 Atherosclerosis Atherosclerosis is one type of arteriosclerosis in which fatty plaques composed of low-density fatty acids erode the artery wall with resulting deposition of macrophages and white blood cells. The plaque increases in size over a period of time, causing a gradual decrease in the size of the arterial lumen and reduced blood flow to the distal tissues. The critical level is occlusion of more than 80% of the arterial lumen. In addition, particles of plaque can break away, migrate to smaller arteries or arterioles (termed thromboemboli), and also cause tissue ischemia. (Copyright Medmovie.com with all rights reserved.)
Macro- and Microcirculation Occlusion of the arterial system can occur in either the macrocirculation (defined as those arteries large enough to be named or with a diameter more than 0.5 mm) or the microcirculation (defined as the arterioles and capillaries too small to be named or with a diameter less than 0.5 mm). Tissue ischemia that leads to lower extremity wounds tends to occur more in the presence of large vessel or mixed disease. In addition to PAOD, the arterial vessels can be occluded by a thrombus or emboli (eg, after surgery or trauma).
Critical Phases of Ischemia In the early stages of PAOD, the circulatory system compensates by establishing collateral circulation around the occlusions in order to maintain peripheral blood flow. The first critical phase of the disease occurs when the collateral circulation is insufficient for the metabolic needs of the affected extremity; therefore, the limited blood supply is shunted to the muscle arteries where flow resistance is low instead of to the skin where resistance is high. A wound caused by trauma (eg, a blister from poorly fitting shoes, a skin tear, or a cut from podiatric care) during this period of decreased skin perfusion will heal more slowly than normal, or will be more likely to become infected and fail to heal. The non-healing wound may be the first indication that a patient has PAOD.
Because exercise increases the muscle oxygen demand, and thereby its blood volume requirements, a second critical phase occurs when activity or exercise causes relative ischemia and pain. Intermittent claudication, the term for the symptoms of muscle pain and cramping that occur with exercise, is a second indication that the patient may have PAOD.
When the PAOD becomes severe, the third critical phase, the patient will probably experience resting pain, gangrene, and non-healing wounds in the extremity below the occlusion. During this phase, the patient may exhibit dependent leg syndrome, a position that allows gravity to assist blood flow to the distal extremity and thereby alleviate some of the pain. The patient frequently complains of rest pain during the night, a result of lower blood pressure and subsequent diminished flow to the lower leg and foot.
Etiology
Impairment of blood flow can occur acutely (trauma or thrombosis) or chronically (atherosclerosis or arteriosclerosis). Both acute and chronic arterial insufficiency at any level (arteries, arterioles, capillaries) can lead to the formation of lower or upper extremity wounds. Reduced capillary flow (also called small vessel disease) is observed most frequently as a result of diabetes.
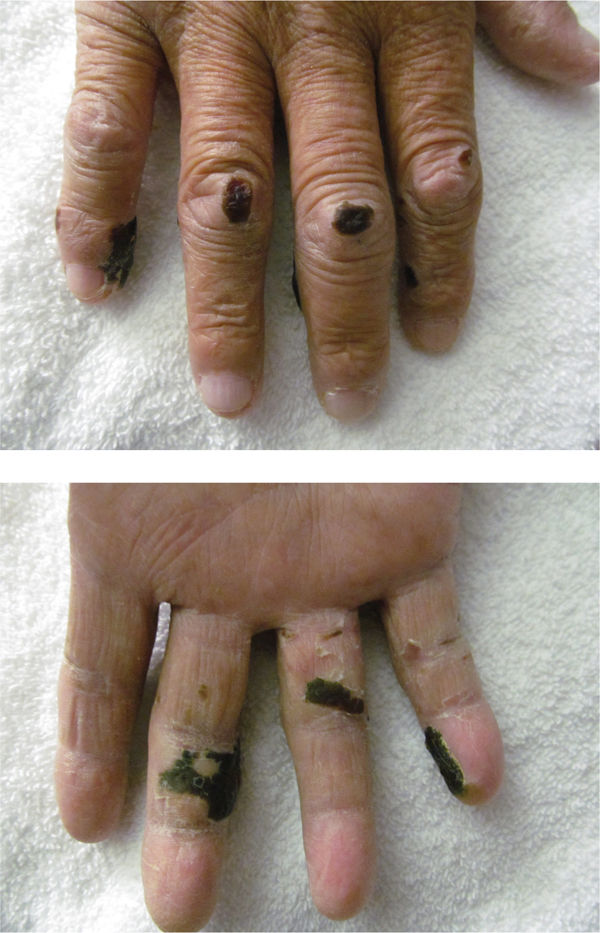
Obstruction of arterial flow can also be classified as anatomic or functional. Anatomic causes of obstruction include thrombo-emboli and vasculitis. (FIGURES 4-3, 4-4) Functional impairment occurs in conditions such as Raynaud’s phenomenon in which abnormal vasomotor function leads to reversible obstruction. (FIGURE 4-5) In severe cases this may result in ulceration. Other potential causes of impaired arterial flow include upper extremity arterio-venous fistulas and aneurysms. (FIGURE 4-6)
FIGURE 4-3 A. Arterial wound due to thromboemboli Arterial wounds that are caused by thromboemboli begin as dusky discoloration (as noted in the third toe) and progress to dry or wet gangrene (as noted in the fourth and fifth toes). If the tissue reperfuses as the medical condition improves, milder cases can resolve and healing can progress almost like a bruise healing. The tissue necrosis becomes well-defined by a process termed demarcation. Debridement is usually deferred until demarcation is completed unless there are signs of clinical infection; protective measures are recommended to prevent further tissue loss. Keeping the extremity warm facilitates vasodilation, which can help maximize perfusion. B. Arterial wound due to trauma Trauma from multiple causes, including surgery, can result in clotting and thrombi that occlude vessels of any size. Distal tissue will become necrotic unless flow is restored emergently.
FIGURE 4-4 Ischemic wound due to vasculitis Vasculitis, an inflammation of the vessels that results in edema and occlusion, most often occurs in patients who have autoimmune disorders (eg, systemic lupus erythematosus, rheumatoid arthritis, untreated hepatitis). The wounds are exquisitely painful, do not become necrotic like other arterial wounds, and may occur on any part of the body. (See Chapter 8, “Atypical Wounds.”)
FIGURE 4-5 Raynaud’s phenomenon Raynaud’s syndrome is caused by vasospasm of the small arteries and arterioles resulting in ischemic changes such as skin color, numbness, and cold sensations. The attacks can be triggered by cold exposure or emotional distress. Symptoms are bilateral, begin distal and progress proximally, and in severe chronic cases can result in ulceration or gangrene.
FIGURE 4-6 Arterial wound due to AV shunt for hemodialysis Patients who are on long-germ hemodialysis and have a history of clotted AV shunts may develop arterial wounds in the fingers as a result of decreased blood flow distal to the shunt.
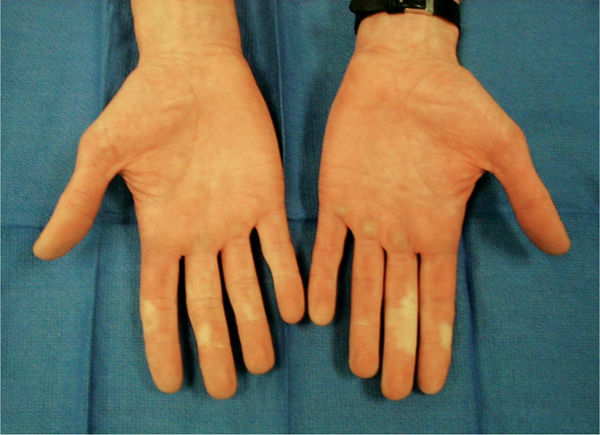
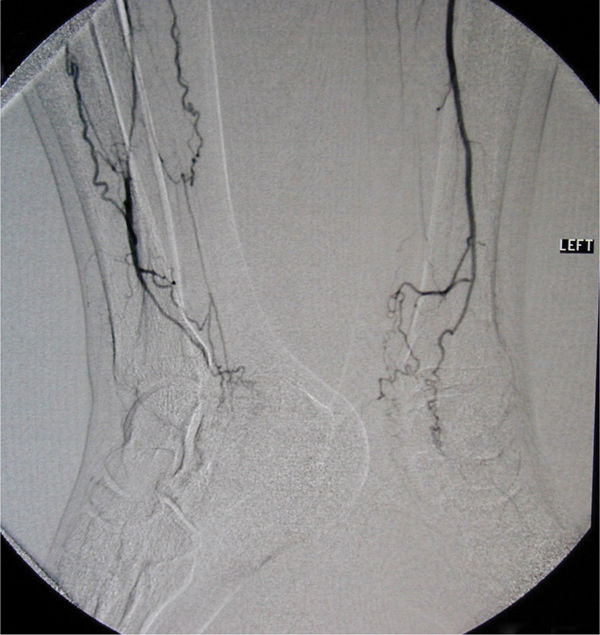
Non-atherosclerotic or vasculitic disorders need to be considered in the patients who present with signs of tissue ischemia in the presence of normal pulses or diminished pulses. For example, thromboangiitis obliterans, also known as Buerger disease, is a macrovascular disorder. Common in men who are heavy smokers, the pathology is an immune and inflammatory disease of the peripheral arteries accompanied by vasospasm and thrombi in the arterial segments to the feet and/or hands. Occlusion of the arteries causes tissue ischemia with resulting thin, shiny skin and thickened malformed nails. Other symptoms include pain, tenderness, erythema caused by dilated capillaries, thin, shiny skin, and cyanosis caused by deoxygenated blood cells in the interstitium. If the disease exacerbates, the patient is at risk for gangrene or ulceration. Successful treatment must include cessation of smoking.12 (FIGURES 4-7, 4-8) Chapter 8, Atypical Wounds, includes further discussion of ischemic wounds due to unusual pathologies.
FIGURE 4-7 Buerger disease Buerger disease, also known as thromboangiitis obliterans, is an immune inflammatory disease of the smaller peripheral arteries. Symptoms can vary from mild pain of the area distal to the inflamed arteries to severe vasospasm with cyanosis or occlusion with gangrene.
FIGURE 4-8 Radiograph of Buerger disease Arterial radiograph of patient with Buerger disease shows the convoluted, distorted vessels in the distal lower extremity.
Patient Evaluation
The initial assessment of any wound begins with a thorough history and physical examination, a process necessary to establish a diagnosis of wound etiology. The history includes screening for risk factors of atherosclerosis—especially smoking, diabetes, hyperlipidemia, and hypertension. Patients who have these risk factors need aggressive education and treatment to modify these factors and to encourage lifestyle changes. A thorough vascular medical history of coronary artery disease (angina pectoris or myocardial infarction) and carotid disease (transient ischemic attacks or ischemic stroke) increases the likelihood of PAOD because atherosclerosis is a systemic disease and not just localized to a specific part of the body. Assessment of ambulation tolerance (by both patient report and treadmill testing) may uncover mild chronic limb ischemia with intermittent claudication. Other co-morbidities, medications, and surgical history are obtained to determine any other contributing factors that may inhibit wound healing.
Clinical Presentation
A thorough wound assessment and information about how the wound began are important in determining the etiology. Refer to Chapter 3 for more details on obtaining a subjective history.
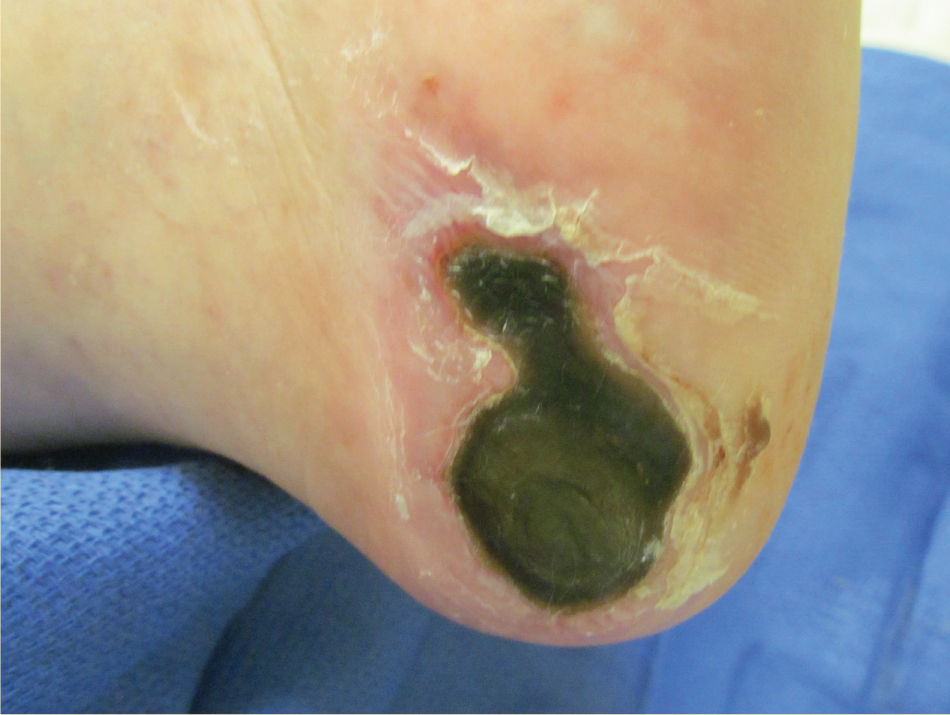
The location, size, and depth of the wound are defining characteristics of ischemic wounds, which tend to be small and round with smooth, well-demarcated borders. The wound base is typically pale (lack of arterial inflow), lacks granulation tissue, and may be shallow or deep. (FIGURE 4-9) Wet or dry necrotic tissue may be present; wet gangrene is significant for active infection and must be urgently debrided. (FIGURES 4-10, 4-11) Arterial wounds tend to occur at the distal digits; although wounds that occur on other parts of the foot (eg, the malleoli) from pressure may not heal due to arterial insufficiency. (FIGURE 4-12) Because of the ischemia, arterial wounds are painful and often accompanied by complaints of pain when the feet are elevated, especially at night. Pain that is reduced with leg dependence is indicative of rest pain.
FIGURE 4-9 Typical arterial wound The typical arterial wound due to PAOD is located on the distal digit, has a round punched-out appearance, dry-to-necrotic wound bed, and little or no granulation tissue. The wounds tend to be painful with poor healing potential without restoration of blood supply.
FIGURE 4-10 Dry gangrene Arterial wounds with dry adhered eschar and no signs of infection are termed dry gangrene.
FIGURE 4-11 Wet gangrene If the necrotic tissue becomes infected with drainage, detached edges, and wet periwound skin, it is termed wet gangrene.
FIGURE 4–12 Non-healing pressure ulcer secondary to arterial insufficiency Wounds of other etiologies (eg, trauma, pressure, or venous insufficiency) that fail to heal may be one of the first signs that a person has PAOD. If the edges stay adhered with no signs of infection, debridement is deferred or not recommended until perfusion is restored and signs of angiogenesis are visible at the edges. Loose detached edges, as seen in this heel pressure ulcer, may be removed to increase the oxygen perfusion of the periwound skin and decrease the risk of infection.
Clinical signs of infection such as malodor, exudate, and erythema are noted in order to initiate appropriate antibiotic treatment and proper debridement. The presence of any exudate should also be characterized by the amount and color (refer to Chapter 3). If the wound can be probed to bone, there is a high probability of osteomyelitis. (FIGURE 4-13)
FIGURE 4–13 Osteomyelitis Osteomyelitis is suspected in any arterial wound that can be probed to bone or that has an edematous “sausage” appearance.
Other observations indicative of PAOD include hair loss, muscle atrophy, atrophy of subcutaneous tissues and skin and appendages, dry, fissured skin, discoloration, and dependent hyperemia. (FIGURE 4-14)
FIGURE 4–14 Typical appearance of extremity with PAOD Extremities that have PAOD tend to have thin shiny skin, atrophied subcutaneous tissue and muscles, thick yellow nails, lack of hair, dry fissured skin, discoloration, and dependent hyperemia (termed rubor of dependency).
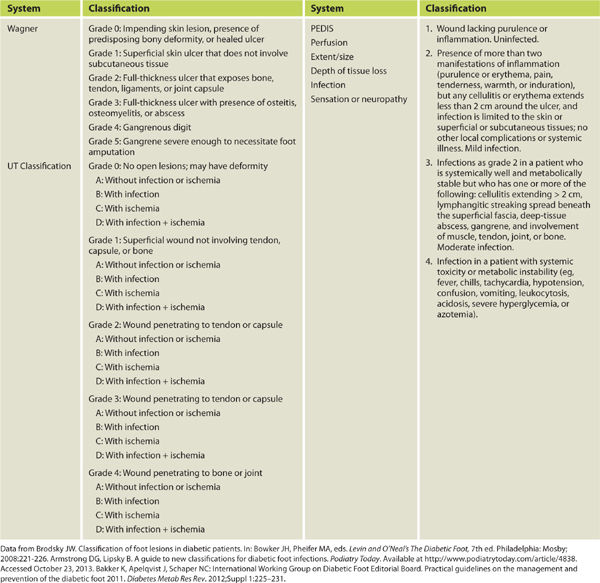
Wound classification systems exist to stratify the severity of the ulceration and are based on the size, location, tissue loss, presence of infection, and the status of the arterial blood flow. There are three classification systems: Wagner grading; the University of Texas (UT) classification; and PEDIS or Perfusion, Extent, Depth, Infection, Sensation, which was developed by the International Consensus on the Diabetic Foot.13 (TABLE 4-2) These classification systems were developed for diabetic foot wounds and are not applicable to other types of wounds (eg, venous, pressure, or atypical).
TABLE 4-2 Classification Systems for Diabetic Foot Wounds
Non-Invasive Vascular Studies
Pulses The initial step of any vascular examination is palpation of pulses in the involved extremity that are compared with pulses of the contralateral limb in order to help determine the extent of diminished flow. The palpation of peripheral pulses is affected by the skill of the examiner and the room temperature. Patience is sometimes needed to feel the pedal pulses and the examiner may be misled by “feeling” one’s own pulse, especially when using the forefinger which has a strong digital pulse. Strength and interpretation of pulses have two different commonly used grades, thus consistency among team members is needed for accurate communication. (TABLE 4-3)
TABLE 4-3 Grading Scales for Pulse Examination
Data from Hill DR, Smith RB. Examination of the extremities: pulses, bruits, and phlebitis. In: Walker HK, Hall WD, Hurst JW, eds. Clinical Methods: The History, Physical, and Laboratory Examinations, 3rd ed. Boston: Butterworths; 1990. Available at http://www.ncbi.nlm.nih.gov/books/NBK350. Accessed October 20, 2013.
The character of the pulse refers to the upstroke, downstroke, and presence of thrills. In stiffened vessels or in vessels with high outflow resistance, the upstroke or radial expansion of the vessel may be slowed. In the presence of low outflow resistance, such as proximal to a traumatic arteriovenous fistula, downstroke may be significantly reduced. The absence of pulses suggests a proximal critical stenosis or occlusion. After palpation of the pulses, auscultation of the pulses by the examiner permits the detection of bruits, frequently an indicator of an upstream or nearby stenotic lesion. The pulse examination, when correlated with clinical symptoms, helps identify the site and severity of arterial occlusive lesions and indicates when further vascular testing is necessary.
Doppler Examination If pulses are faint or not palpable, a hand-held Doppler can detect flow within the vessel; however, the presence of a signal is not an indication of normal flow. (FIGURE 4-16) Even in the most severe cases of PAOD and gangrene, patients may continue to have Doppler signals in the pedal arteries. The Doppler examination is usually begun distally, and is not indicated at the more proximal locations if a pulse is palpable.
FIGURE 4–16 Hand-held Doppler A hand-held Doppler is used to detect blood flow if pulses are not palpable; however, a positive Doppler sound is not indicative of normal blood flow. Doppler sounds can be described as triphasic, biphasic, monophasic, or absent; or they can be described as weak or strong.
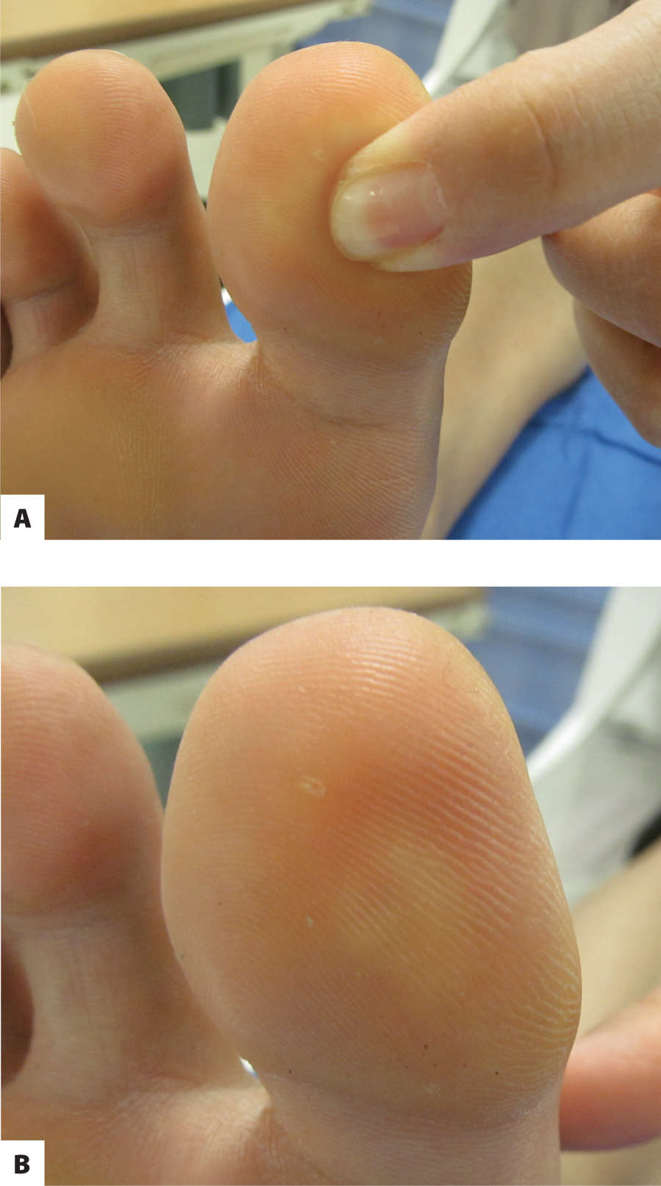
Capillary Refill Time The severity of microvascular disease (eg, with patients who have diabetes or Raynaud phenomenon) can be estimated by counting capillary refill time (CRT). CRT is measured by pressing the end of the toe or the skin just proximal to the wound until the color disappears and by measuring the time for recovery to the original color. (FIGURE 4-17) Normal CRT is less than 3 seconds; however, it is prolonged in extremities with microvascular disease and may vary greatly among patients. Thus it is only a screening test and an indicator that more precise vascular testing may be indicated.
FIGURE 4–17 Capillary refill time Capillary refill time is measured by pressing the skin until it blanches, releasing, and counting the seconds it takes to return to normal color. Normal capillary refill time is 2 seconds; more than 3 seconds is indicative of microcirculation or small vessel disease.
Rubor of Dependency Rubor of dependency test is a screening procedure for ischemia that can be performed at bedside; thus, it is not definitive but indicative of PAOD. The extremity is elevated to 30° and observed for pallor. When the foot with normal circulation is placed into a dependent position, it will become a healthy pink color in approximately 15 seconds. If the reperfusion takes 30 seconds or longer and causes a dark-red or rubor appearance, the test is positive for severe ischemic disease.15
Ankle Brachial Index The ankle-brachial index (ABI), a ratio of the ankle systolic blood pressure to the brachial systolic blood pressure, indicates the severity of peripheral arterial disease present in the lower extremity. A 10–12 cm sphygmomanometer cuff is placed just above the ankle and inflated. A hand-held Doppler is used to measure the systolic pressure of the posterior tibial and the dorsalis pedis arteries of each leg by noting the pressure at which the pulse returns as the cuff is deflated. Then, the pressures are normalized to the higher of the brachial pressures. The equations for the ABI are as follows:
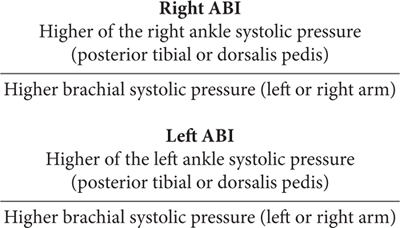
The only contraindication for performing the ABI examination is the presence of an ulcer near the ankle, since compression of the ulcer with the sphygmomanometer cuff may cause significant pain to the patient. Interpretations of ABI values are listed in TABLE 4-4. In some patients with diabetes, renal insufficiency, or other diseases that cause vascular calcification, the pedal vessels at the ankle become non-compressible. This leads to an elevation of the ankle pressure and consequently an ABI > 1.30. In these patients additional noninvasive diagnostic testing is indicated to evaluate the patient for PAOD.
TABLE 4-4 Interpretation of Ankle Brachial Index
Ankle-brachial index (ABI) is used to determine the severity of peripheral arterial occlusive disease and to select interventions that will promote healing without causing more tissue necrosis, eg, by using too much compression for lower extremity edema or by debriding a poorly-perfused wound with eschar. The test can be easily performed in any clinical setting with a blood pressure cuff and hand-held Doppler.
Toe Pressures Toe pressures are used in patients with calcified vessels and abnormally high ABI or non-compressible vessels, typical of patients with diabetes. A pneumatic cuff, about 1.2 times the diameter of the digit, is wrapped around the proximal phalanx and a flow sensor is applied distally to the digit. Toe pressures that are greater than 50 are considered normal and those that are less than 50 are abnormal. The majority of patients with foot ulcers or wounds that are caused by PAOD have a toe pressure less than 30. In non-diabetic patients, a toe pressure greater than 30 mmHg, and in diabetic patients, 55 mmHg, will usually lead to healing.16 The normal toe/brachial index, also considered a reliable indicator of lower extremity vascular status, is 0.8–0.99.17
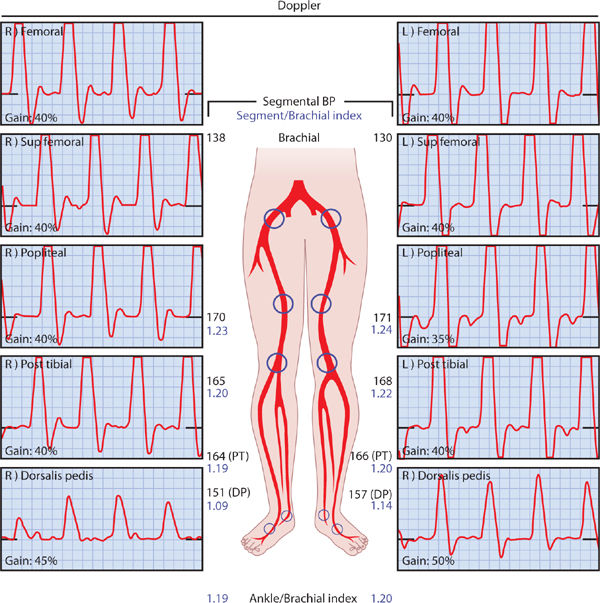
Segmental Pressures Segmental limb pressure is measured by combining Doppler ultrasound or plethysmography with blood pressure measurements at various locations in the arms and legs. Segmental pressures are a useful adjunct to the physical examination and ABI because they can illustrate differences in blood pressure at specific sites in the extremities and identify gradients that indicate the presence of disease.
A normal variation in the pressures between limb segments is 20–30 mmHg. A difference of 30 or greater indicates significant obstruction. Similarly, variations of pressure between symmetric limb segments do not differ by more than 20 mmHg unless there is an abnormality. Although they are strong indicators, limb pressure measurements are far less sensitive and specific than duplex imaging in the accurate diagnosis of arterial disease.19 (FIGURE 4-18)
FIGURE 4–18 Arterial profile includes segmental pressures This study shows arterial waveforms from the femoral artery through the toes. Pressures and waveforms analyses are evaluated at each arterial segment. Triphasic arterial waveforms are identified throughout all segments except the right dorsalis pedis artery where the waveform displays a biphasic pattern. Comparison to the brachial artery pressure allows calculation of the ankle-brachial index.
Transcutaneous Oxygen Perfusion (TcPO2) Another important tool in evaluating the patient with the chronic wound is measurement of transcutaneous oxygen measurements (TcPO2), defined as skin oxygenation. The measurement of TcPO2depends on the cutaneous blood flow, the oxyhemoglobin dissociation, and the diffusion of oxygen through the tissues and thus reflects the metabolic state of the target tissues. The measurements are taken usually on the dorsum of the foot, antero-medial calf approximately 10 cm below the patella, and in the thigh approximately 10 cm above the patella. (FIGURE 4-19) The reference site is usually on the chest in the infraclavicular area. The limb is maintained in the dependent position to help increase blood flow.
FIGURE 4–19 Measuring transcutaneous oxygen tension Transcutaneous oxygen tension, measured on the foot of a patient with arterial wounds on the toes, is a good indicator of healing potential.
A normal TcPO2 is between 60 and 90 mmHg. A measurement greater than 30 mmHg indicates adequate perfusion for healing, whereas if the tissue surrounding an ulcer has a TcPO2 less than 20 mmHg, the wound typically will not heal. In addition, patients with a TcPO2 less than 20 mmHg will typically experience rest pain. A TcPO2 value greater than 40 mmHg is desirable to support minor amputation site healing (toe amputation or transmetatarsal amputation). (TABLE 4-5)
TABLE 4-5 Interpretation of TcPO2
Transcutaneous oxygen tension (TcPO2) is a measure of oxygen tension in the skin and is used to determine severity of microvascular disease. The readings also serve as indicators for wound healing potential and safe debridement of necrotic tissue.
Exercise Stress Test The exercise stress test (EST) assesses PAOD in patients with borderline ABIs (0.92–1.0) and symptoms of claudication. A resting ABI is performed first, after which the patient walks on a treadmill (typically at 2 miles per hour with an incline of 10–12%) for five minutes or until symptoms of claudication cause the patient to cease the activity. An alternative exercise activity is performance of 50 heel raises in the standing position. The duration of exercise and the nature of the symptoms are recorded. The patient is placed in a supine position and the ankle pressure measurements are recorded every 30 seconds until (1) the BP has returned to baseline or (2) 10 minutes have elapsed. BP values after exercise are compared to pre-exercise values. Normally, there is little or no change in the ankle or brachial BPs; however, PAOD sufficient to cause claudication will result in a drop in the ankle pressure of at least 25 mmHg, 25% decline of the resting ankle pressure, or a decrease in the ABI > 0.15. A negative EST with the same symptoms suggests cardiorespiratory, neurologic, or musculoskeletal disease.18
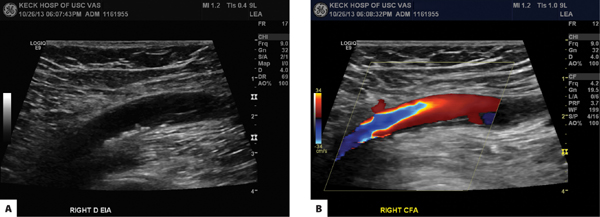
Arterial Duplex Ultrasonography is one of the most important diagnostic tools for the vascular system. Many of the terms associated with ultrasound are often used interchangeably and/or incorrectly. A basic understanding of how the technology is applied will help understand when which test is needed.
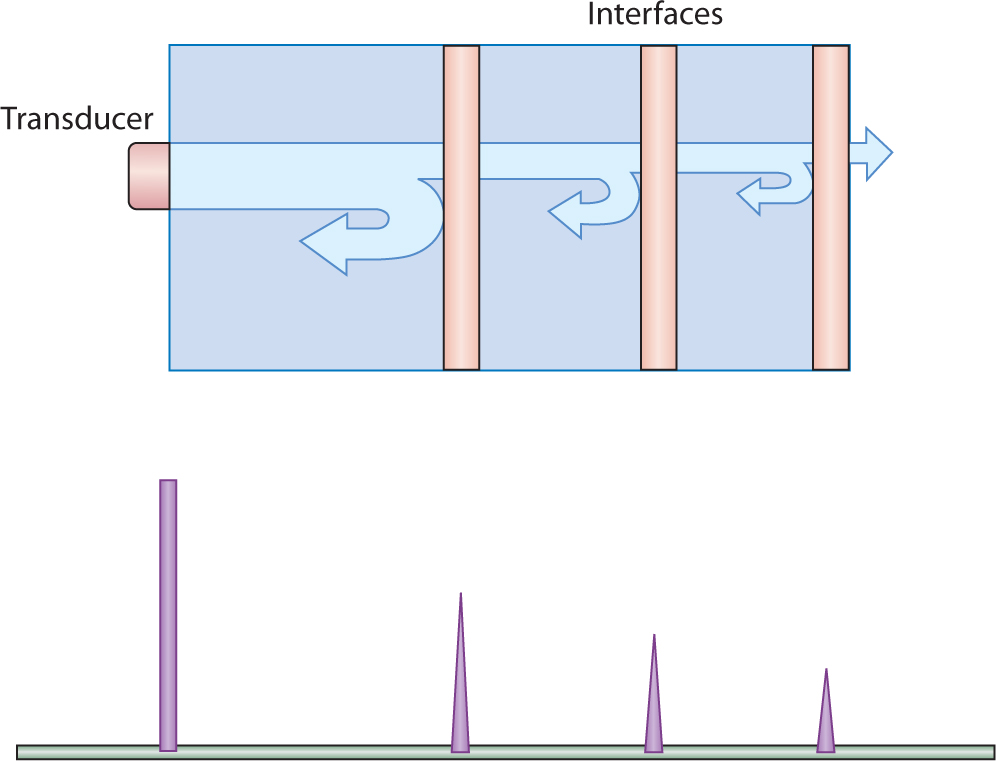
The principle of ultrasound is bouncing sound waves away from a probe and back to a receiver that measures the time for the echo or returning sound wave to return after it was emitted. (See Chapter 16 for more discussion on ultrasound.) Time and strength of the returned sound waves are amplified and transformed into a visual representation described as A-mode or B-mode. A- or “amplitude” mode represents the signal as an amplitude (FIGURE 4-20). B- or “brightness” mode adds a linear array of scanners that scan a plane through the body to create a 2D image with densities represented as varying degrees of “brightness.” This creates a more anatomical representation (FIGURE 4-21).
FIGURE 4-20 Ultrasound, A-mode A-mode ultrasound simply shows the amplitude of the sound waves and is rarely used for diagnostic purposes with the development of Duplex scans.
(Used with permission from DeMaria AN, Blanchard DG. Chapter 18. Echocardiography. In: Fuster V, Walsh RA, Harrington RA, eds. Hurst’s The Heart. 13th ed. New York, NY: McGraw-Hill; 2011. http://www.accessmedicine.com/content.aspx?aID=7805593. Accessed November 16, 2013.)
FIGURE 4–21 Ultrasound, B-mode B-mode ultrasound is the reflected sound waves plotted on an oscilloscope to create a two-dimensional image of the anatomical structure. Figure (A) is the external iliac artery without color (the artery is the dark area in the middle of the image), and figure (B) is the right common femoral artery with color added to show direction of flow. Red is typically flow away from the heart and blue is flow toward the heart. A mosaic of color is interpreted as a stenosis, a point at which flow is scattered in both directions.
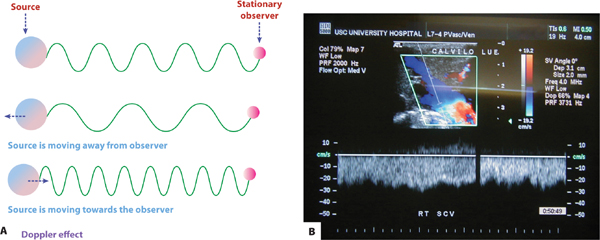
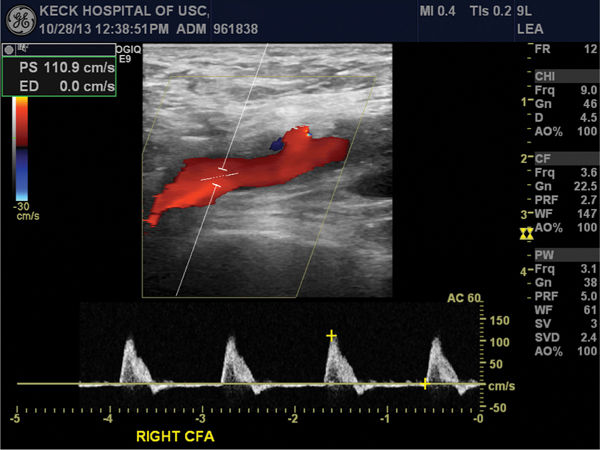
Doppler ultrasound builds on this by using the Doppler effect. (FIGURE 4-22) This is a change in the frequency of a detected wave when the source or the detector is moving, and can measure flow, or in arterial studies, specifically blood flow from the heart to the peripheral extremities. Differences in flow can be represented as changes in color flow Doppler. Additionally, Doppler ultrasound can be continuous or pulsed waves. Pulsed wave Doppler has the advantage of detecting velocities in a small area very accurately, whereas continuous wave can measure higher velocity flows over a larger area. Finally, the term duplex ultrasound refers to a simultaneous presentation of Doppler (usually pulsed wave) and 2D or B-mode imaging. (FIGURE 4-23)
FIGURE 4-22 Doppler with color flow imaging The Doppler effect is used to measure the velocity of blood flow in a vessel and is based upon the principle that flow toward the receiver creates shorter waves than flow away from the receiver. The velocity of flow in the vessel (in this case a vein) is shown on the bottom of the screen in the color flow imaging.
FIGURE 4–23 Arterial duplex with color flow imaging Arterial duplex scan of the common femoral artery. The flow pattern is laminar in nature (as identified by the homogeneous color of the moving blood through the vessel imaged). The waveform is a triphasic waveform with a peak systolic velocity of 110.9 cm/sec. Signs of a stenotic lesions would show a more mosaic flow color and higher velocities (over 250 cm/sec).
Duplex ultrasound imaging provides both anatomic and hemodynamic blood flow assessment in a noninvasive manner. Duplex ultrasound can provide spectral analysis, which shows the complete spectrum of frequencies (that is, blood flow velocities) found in the arterial waveform during a single cardiac cycle.
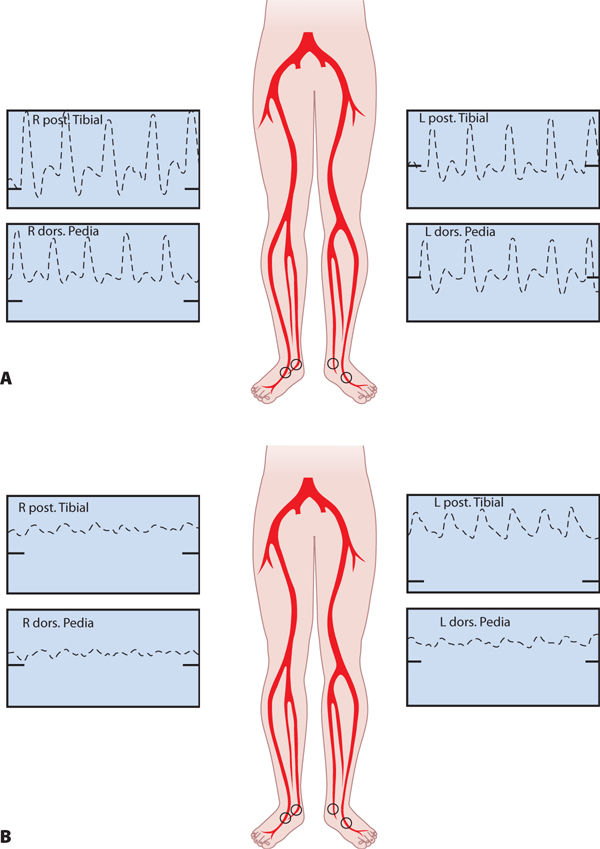
The normal (“triphasic”) waveform is made up of three components that correspond to different phases of arterial flow: rapid antegrade flow reaching a peak during systole, transient reversal of flow during early diastole, and slow antegrade flow during late diastole. Lesions are identified by a change in waveform from triphasic to monophasic, or an increase in peak systolic velocity (PSV) followed by a drop in velocity. (FIGURE 4-24A and B) Certain ratios of the PSV within an area of stenosis to the PSV of the proximal normal segment correlate with the degree of stenosis.
FIGURE 4–24 Arterial waveforms A. Normal arterial waveforms are triphasic and correspond to phases of arterial flow. B. Abnormal waveforms occur with macrovascular occlusion and vary from moderate (biphasic) to severe (monophasic and flat), depending on the extent of the occlusion.
Computerized Tomographic Arteriography Accurate evaluation of the arterial blood supply is paramount for successful revascularization of the ischemic extremity for patients with or without diabetes. Arterial imaging is challenging for patients with ischemic complications because they frequently have underlying renal insufficiency, a condition that limits the amount of iodinated contrast that can be injected.
Computerized tomographic arteriography (CTA) involves injection of contrast medium into an upper extremity vein followed by CT scan of the diseased arteries. CTA is a safe, noninvasive procedure that provides high-quality imaging of the arteries; however, significant arterial calcification can impede the transit of contrast in the distal segments of the extremity, in which case more images and higher radiation doses are required. In addition, CTA is only a diagnostic tool and not sufficient for pre-surgical evaluation.
Magnetic Resonance Angiography Magnetic resonance angiography (MRA) can be performed with a contrast agent injected intravenously, termed flow dependent because the presence of the contrast in the diseased arteries depends upon the blood flow getting to that area. The MRA can also be done without contrast, termed flow independent. MRA images are not obscured by arterial calcification; however, the disadvantages are motion artifact, long acquisition times, anxiety in patients who are claustrophobic, and possible nephrogenic systemic fibrosis in the patient with renal insufficiency.
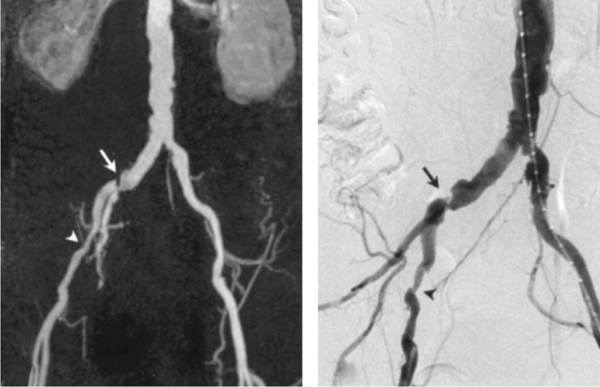
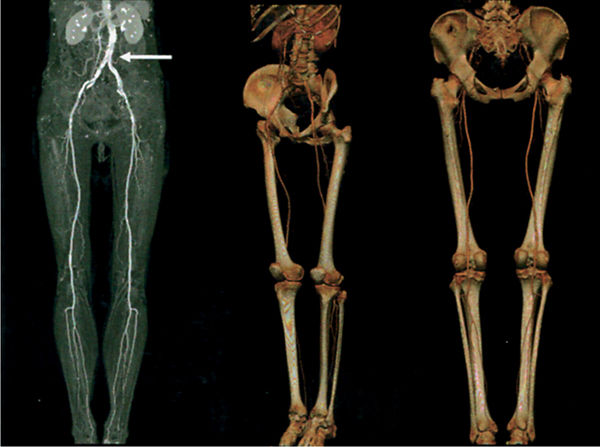
For patients who require revascularization, arteriography using digital subtraction techniques is preferred to determine appropriateness for endovascular revascularization versus surgical bypass. (FIGURES 4-25, 4-26)
FIGURE 4-25 Magnetic resonance arteriography Magnetic resonance arteriography of a male with intermittent claudication. The arrows point to the stenoses in the right common iliac artery and external iliac artery.
FIGURE 4-26 Computerized tomography arteriography CTA image of a male with calcifications in the abdominal aorta. The peripheral vessels are patent in both lower extremities.
Invasive Tests
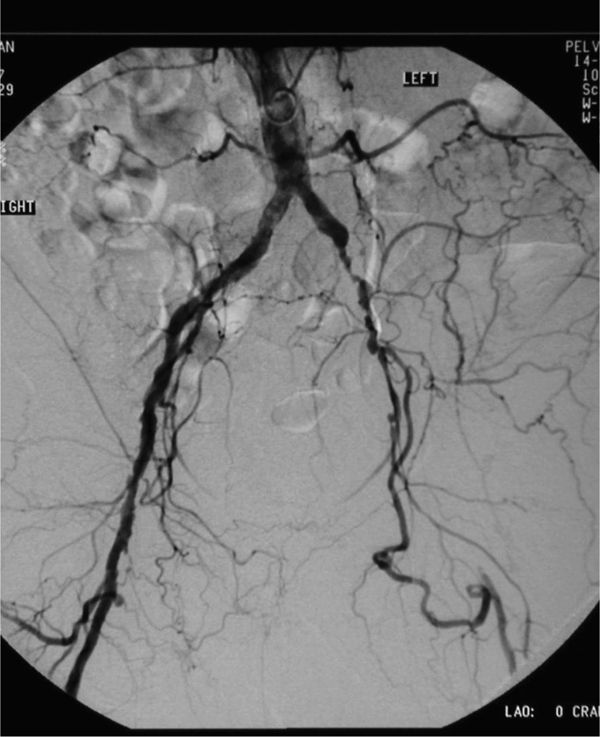
Arteriogram Angiography (or arteriography when referring specifically to the arterial system) is radiographic imaging of a contrast-filled blood vessel. (FIGURE 4-27) Despite advances in the quality and availability of the previously described modalities, arteriography remains the “gold standard” for pre-surgical evaluation of the diseased arteries. There are clinical scenarios in which angiography is not the first choice because of its invasiveness; however, the explosion of endovascular therapy of vascular disease has strengthened angiography as a preferred method because of its sensitivity and ability to be easily combined with endovascular treatment.
FIGURE 4–27 Arteriogram of lower extremity vessels Arteriogram of the aortoiliac segment of the arterial circulation. Extensive disease is seen in the left distal common iliac and the external iliac is occluded. The vessel seen traversing through the pelvis is the internal iliac artery, which is the main collateral vessel for the occluded external iliac artery on the left.
Arteriography is performed in a procedure room with a fixed, mounted fluoroscopic unit or in an operating room with a mobile x-ray unit that has its own generator, c-arm, and image intensifier or panel detector. The contrast agent is injected manually or via a power injector into the target vessel. One emerging technique is CO2 arteriography, in which CO2 gas is injected to transiently displace blood in the vessel and thereby create an image. CO2 as a contrast agent is preferable in circumstances where systemic or renal toxicity from iodinated contrast is contraindicated or risky for the patient.
Digital subtraction refers to enhancement of the imaging prior to interpretation. The fluoroscopic image is processed, digitized, and amplified to create a more accurate anatomic picture. Arteriography is done through single-injection with staged or stepped technique (the contrast is injected and images are taken either at various points along the extremity to follow the contrast load or via a rotational method). This technique can create a 3D image of the contrast outline using a detector that rotates between two points as the contrast is injected.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Granuloma annulare
Granuloma annulare Necrobiosis lipoidica
Necrobiosis lipoidica Pyoderma gangrenosum
Pyoderma gangrenosum Sweet’s disease
Sweet’s disease Malignant transformation of long-standing ulcer (Marjolin’s)
Malignant transformation of long-standing ulcer (Marjolin’s) Metastatic malignancies
Metastatic malignancies Primary skin malignancies
Primary skin malignancies Ulcers associated with hematologic or internal malignancies
Ulcers associated with hematologic or internal malignancies Bacterial (Pseudomonas, staphylococcal scalded skin syndrome, streptococcal necrotizing fasciitis)
Bacterial (Pseudomonas, staphylococcal scalded skin syndrome, streptococcal necrotizing fasciitis) Fungal (blastomycosis, chromomycosis, Madura foot)
Fungal (blastomycosis, chromomycosis, Madura foot) Mycobacterial (M. leprae, M. tuberculosis, M. ulcerans)
Mycobacterial (M. leprae, M. tuberculosis, M. ulcerans) Parasitic (Chagas disease, leishmaniasis)
Parasitic (Chagas disease, leishmaniasis) Viral (herpes simplex, herpes zoster)
Viral (herpes simplex, herpes zoster) Drug reactions leading to blisters and large-scale wounds (erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis)
Drug reactions leading to blisters and large-scale wounds (erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis) Blistering (epidermolysis bullosa, pemphigoid, pemphigus)
Blistering (epidermolysis bullosa, pemphigoid, pemphigus) Nonblistering (dermatomyositis, lupus, rheumatoid arthritis, scleroderma)
Nonblistering (dermatomyositis, lupus, rheumatoid arthritis, scleroderma) Hypertensive ulcers (Martorel’s)
Hypertensive ulcers (Martorel’s) Sickle cell disease
Sickle cell disease Thromboangiitis obliterans
Thromboangiitis obliterans Vasculitis
Vasculitis Antiphospholipid antibody syndrome
Antiphospholipid antibody syndrome Disseminated intravascular coagulation, purpura fulminans
Disseminated intravascular coagulation, purpura fulminans Heparin necrosis
Heparin necrosis Homocystinuria
Homocystinuria Livedoid vasculitis
Livedoid vasculitis Polycythemia vera
Polycythemia vera Thrombotic thrombocytopenic purpura
Thrombotic thrombocytopenic purpura Vasospastic/Raynaud’s disease
Vasospastic/Raynaud’s disease Venous ulcers
Venous ulcers Diabetes
Diabetes Leprosy
Leprosy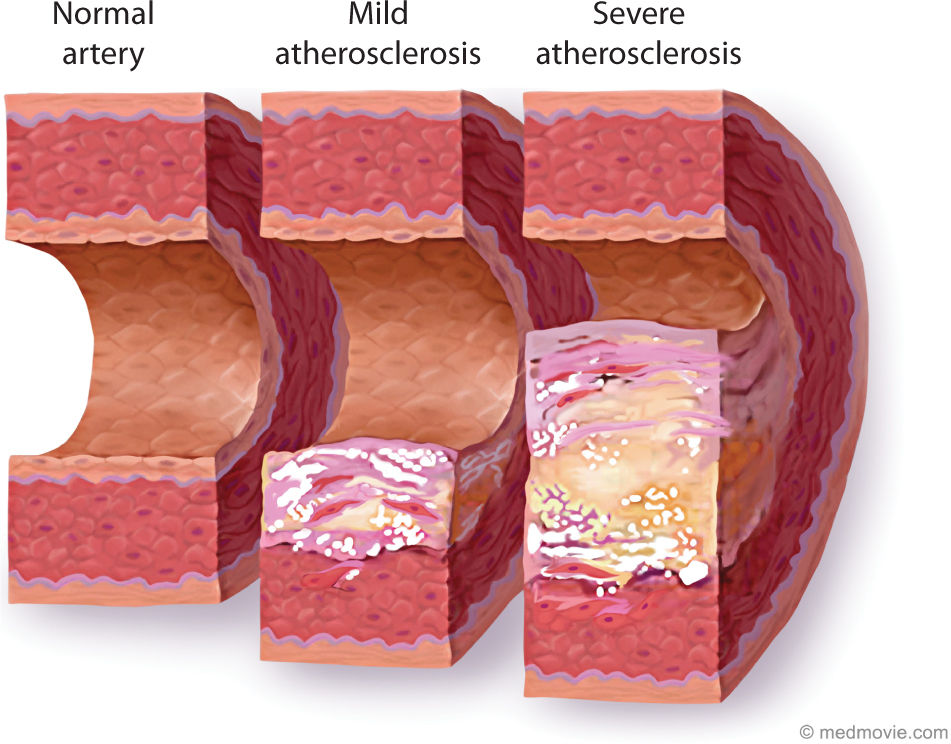









 Aspirin 81 mg daily
Aspirin 81 mg daily Clopidogrel (Plavix) 75 mg daily
Clopidogrel (Plavix) 75 mg daily Furosemide 40 mg daily
Furosemide 40 mg daily Isoniazid 300 mg daily
Isoniazid 300 mg daily Sevelamer (Renvela) 800 mg daily
Sevelamer (Renvela) 800 mg daily Sitagliptin (Januvia) 25 mg
Sitagliptin (Januvia) 25 mg Fish oil
Fish oil Vitamin B6
Vitamin B6 Vital signs: normal for age.
Vital signs: normal for age. Hematocrit—31.3%
Hematocrit—31.3% Hemoglobin—10.4 g/dL
Hemoglobin—10.4 g/dL Platelets—140,000/mm3
Platelets—140,000/mm3 Albumin—3.8 g/dL
Albumin—3.8 g/dL HbA1C—8.7
HbA1C—8.7 INR—1
INR—1 Prothrombin time (PT)—13.3 sec
Prothrombin time (PT)—13.3 sec Partial thromboplastin time (PTT)—30.4
Partial thromboplastin time (PTT)—30.4 BUN—50 mg/dL
BUN—50 mg/dL Creatinine—8.33 mg/dL
Creatinine—8.33 mg/dL