FIGURE 6-1 Moisture on skin Moisture is one of the contributing factors to pressure ulcers, especially in the perineal and perianal areas. The changes in skin as a result of prolonged exposure include maceration, blanched color, and a papillary-like texture, as seen on the area around this sacral pressure ulcer. The drainage can be fecal, urinary, or wound moisture. In addition, the moisture can cause changes in the skin pH, especially in the case of fecal incontinence, which further weakens the skin and increases the risk of pressure ulcer formation.
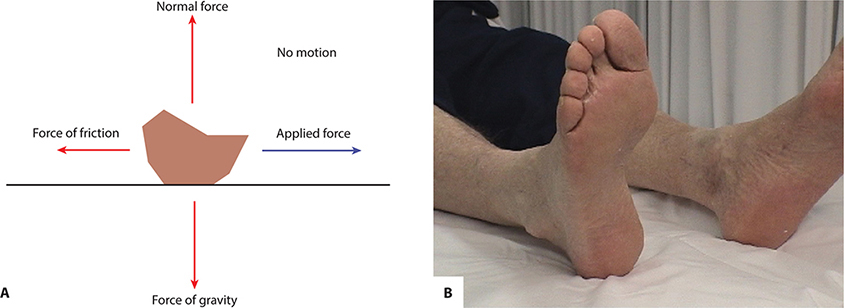
FIGURE 6-2 A, B Friction is defined as the force that results when two objects rub against each other. When skin moves back and forth over a surface (eg, heels on the bed linens), friction occurs and causes erosion of the epidermis and/or blistering between the epidermis and dermis. The schematic demonstrates the small surface area of the heel that becomes the surface area in contact with the bed surface, and the photograph illustrates the most common source of friction, heels rubbing on the bed linen.
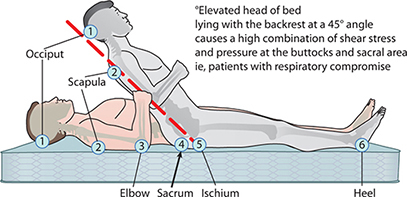
FIGURE 6-3 Shear
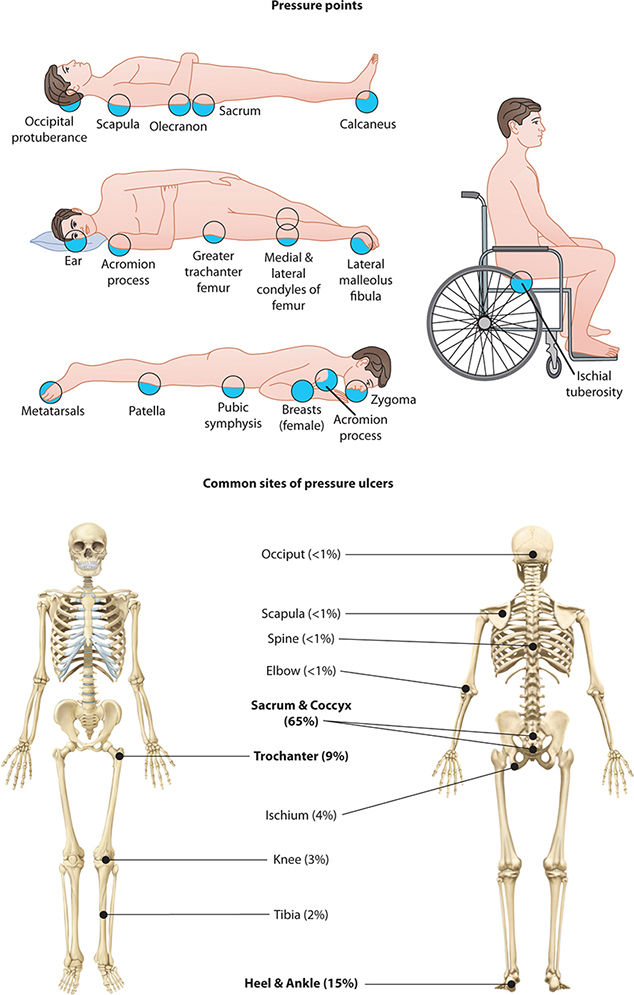
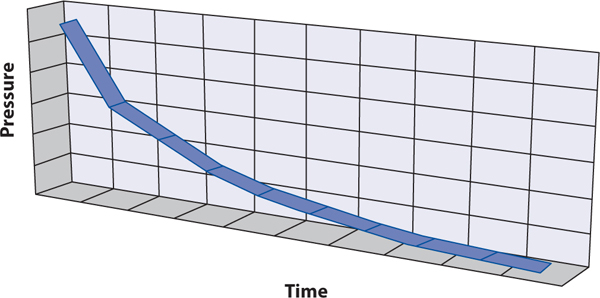
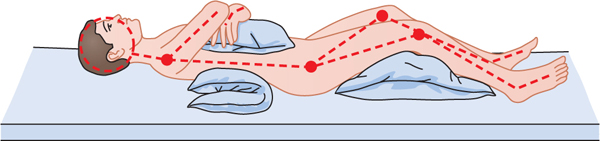
The most common sites for the development of pressure ulcers are the sacrum, ischial tuberosities, trochanters, and heels; however, they can occur on any part of the body where there is unrelieved pressure between an external surface and a bony prominence for a prolonged period of time. The location of pressure ulcer risk changes whether the patient is lying supine or sitting. If the patient is supine, the most common sites will be the sacrum and heels, but in a seated position, the greatest pressure will be on the ischial tuberosities. (FIGURE 6-4) The amount of time leading to destruction varies as described in TABLE 6-1. Reversal of tissue necrosis may or may not occur depending on the patient’s clinical co-morbidities and the healing potential. Skin ulceration is an open wound that occurs within two weeks of tissue necrosis.8 There is an inverse time/pressure curve to skin necrosis, meaning the higher the amount of sustained, unrelieved pressure, the shorter the time frame in which tissue death can occur (FIGURE 6-5).9
FIGURE 6-4 Areas of the body at risk for pressure ulcers By definition, pressure ulcers develop from mechanical forces applied over bony prominences where there is little or no soft tissue to dissipate the forces (friction, shear, or direct pressure). The most vulnerable areas depend upon the individual’s body build.
TABLE 6-1 Time to Tissue Destruction
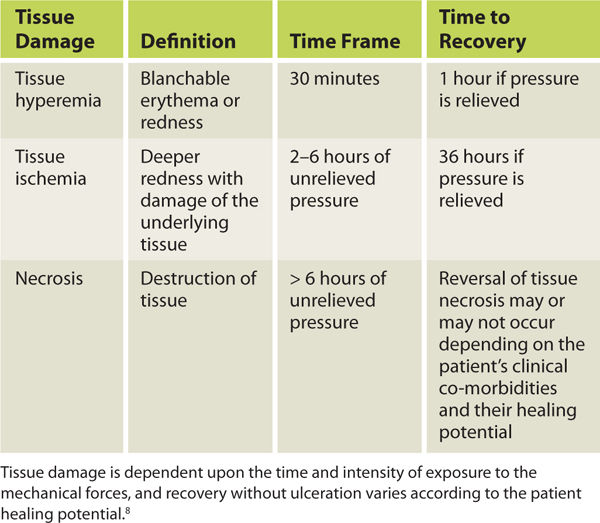
FIGURE 6-5 Time/pressure curve for pressure ulcer formation Tissue damage can occur with prolonged exposure to low pressures or short exposure to high forces, depending on the body morphology, the surface, and the underlying comorbidities. Thus care plans need to be individualized to the patient’s medical status, body type, and risk factors.
Given that the highest rates of pressure ulcers occur on the sacrum, trochanters, and heels, it is estimated that 70% of pressure ulcers occur from the waist down. Healthcare professionals have an obligation to monitor patient skin and to implement a care plan to prevent pressure ulcers from occurring or to facilitate healing of any pressure ulcers a patient may develop. The purpose of this chapter is to educate the healthcare professional on prevention, assessment, and treatment of pressure ulcers.
PREVENTION
The prevention of pressure ulcers begins with a thorough assessment of the patient’s skin. Once this is complete, any lesions (or lack of) are documented in the medical record by the primary practitioner, be that the physician, the midlevel practitioner, or the physical therapist. The nurse or physical therapist can document and photograph the pressure ulcers, but the MD has to sign the documentation within 48 hours of admission. Not only is this good clinical practice, but as of October 2008, Center for Medicare and Medicaid Services (CMS) has linked payment of the higher Diagnostic Related Group (DRG) associated with pressure ulcers to this documentation.10 An assessment tool for the risk of skin breakdown is advised both on admission and periodically thereafter. The most common and most validated scale used in the United States is the Braden scale. (TABLE 6-2)
TABLE 6-2 Braden Scale for Predicting Pressure Sore Risk
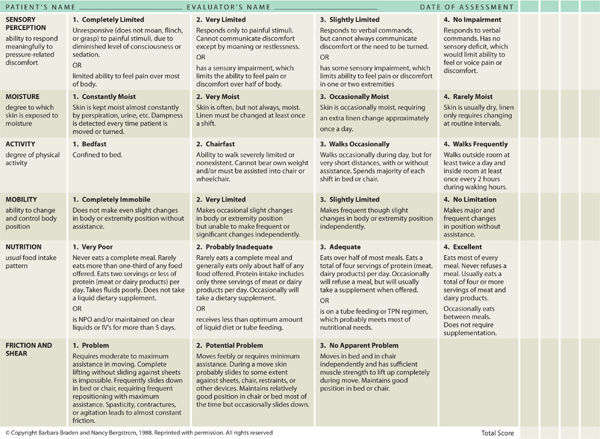
This tool assesses 6 parameters, including activity, mobility, nutrition, sensory perception, moisture, and friction/shear. The highest possible score on the exam is 23; any score less than 18 is considered at risk. This scale, however, is not meant to replace clinical judgment. The assessment is also subject to change depending on the patient’s medical condition; therefore, it needs to be rescored if changes in the clinical assessment occur. For example, when admitted to the hospital for an elective knee surgery, the patient is usually alert and oriented, able to toilet independently, has limited activity and mobility due to knee pain, but is eating well and has no issues with friction or shear. That patient would have a Braden score of 21 and would be considered at low risk for pressure ulcer development. If the patient has complications during surgery and cannot be weaned off of the ventilator, the medical status changes. The patient is now in an ICU setting, intubated, sedated, and incontinent, and therefore at moderate risk for friction/shear when being turned and repositioned. The nutrition is adequate because parenteral nutrition is initiated. This patient now has a Braden score of 10 and is considered high risk for pressure ulcer formation.
Once risk is assessed, prevention strategies are implemented to minimize the risk of skin breakdown. The first of these strategies is turning and repositioning, which will be discussed in detail. Use of pressure redistribution surfaces for both the bed and the wheelchair will help reduce pressure on bony prominences. Another aspect of prevention is management of the medical factors that can put patients at higher risk for skin breakdown. Containment of urinary or fecal incontinence, protection of the skin with a moisture barrier or silicone-backed foam dressing, assessment and maximization of the patient’s nutrition, improved mobility, and proper management of underlying medical conditions such as diabetes mellitus and hypertension are several strategies that decrease the risk of skin breakdown.
INTERVENTIONS TO MANAGE TISSUE LOADING
As described above, both the magnitude and duration of tissue loading are important in the prevention of pressure ulcers. When a pressure ulcer is present, managing the duration and magnitude of loading requires a greater level of attention and is accomplished by using bed support surfaces and wheelchair cushions. These devices are designed to redistribute pressures away from the primary load-bearing parts of the body that are the areas at highest risk for skin breakdown. Clinically, managing the duration of loading is accomplished with postural changes that redistribute loads away from tissues for periods of time (eg, with turning schedules for persons in bed and with weight-shifting activities for persons sitting in wheelchairs). In addition, some cushions and support surfaces can actively change their load redistribution properties to reduce the duration of loading.
Research has not defined a specific threshold for an acceptable magnitude of pressure on tissues. This is not surprising considering the variation in physiology and tissue biomechanics of people at risk for pressure ulcers. Without a clear mandate of acceptable loading on the tissues, clinicians are challenged to manage loads through interventions that must take into account ever-changing technology and the idiosyncrasies of any particular patient. Decisions about appropriate interventions can be facilitated by a working knowledge of support surfaces and positioning technologies, as well as the benefits and deficiencies of the different designs.
Support Surfaces: Beds, Mattresses, and Overlays
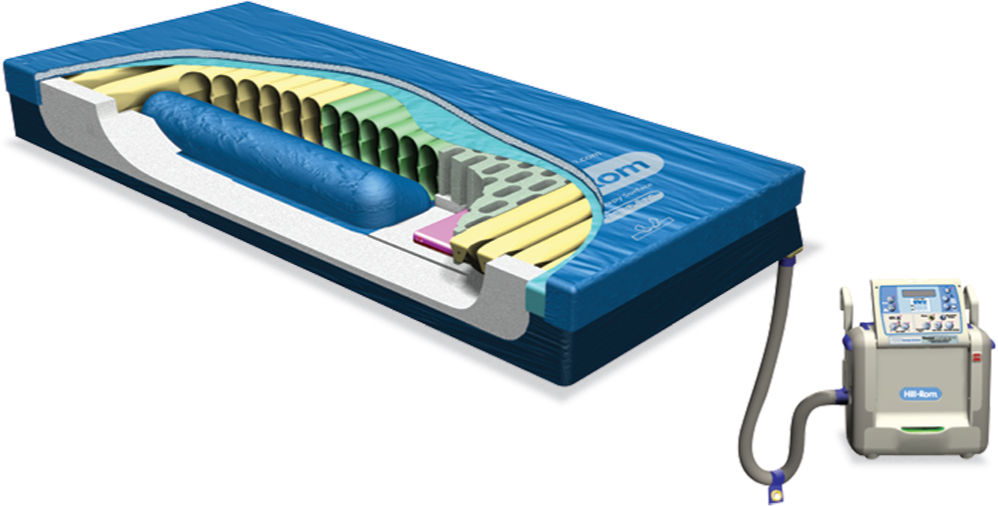
Horizontal support surfaces (such as bed systems, mattresses, and overlays) play a large role in managing tissue loads, especially in the many environments where people are in bed for extended periods, are potentially immobile, and have co-morbidities and/or injuries that weaken the body. Being comfortable with the terminology used to characterize and describe horizontal support surfaces is important for any clinician when reading research about this technology and when communicating with other professionals about appropriate interventions. The National Pressure Ulcer Advisory Panel (NPUAP) has developed a list of common terms and definitions for such purposes.11 TABLE 6-3 lists several categories and features of support surfaces and their respective definitions, and FIGURES 6-6 to 6-9 illustrate some of the designs.
TABLE 6-3 Categories and Features of Support Surfaces
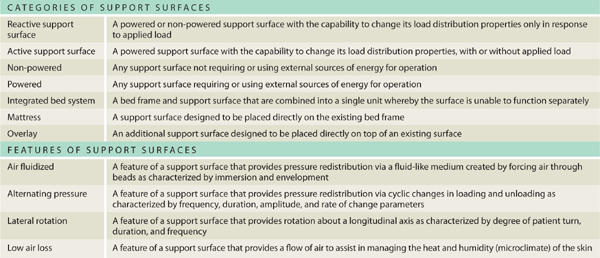
FIGURE 6-6 Cross-section of support surface A cross-section of a pressure-redistribution surface illustrates the combination of materials, construction, and air flow provided by an external pump. (Hill-Rom® P500 Therapy Surface Mattress Replacement System, Hill-Rom Services, Inc. Reprinted with permission. All rights reserved.)
FIGURE 6-7 Active support surface Air is circulated inside cells within the support surface to both immerse and envelope the patient and provide pressure redistribution. This type of powered mattress can be used on an existing bed frame. (Envision® E700 Wound Surface, Hill-Rom Services, Inc. Reprinted with permission. All rights reserved.)

FIGURE 6-8 Alternating-pressure, low-air-loss support surface Alternating pressure in achieved by a pump blowing air through chambers to get rhythmic inflation and deflation and thereby redistribute the pressure. The air blowing through the cover reduces the skin/surface interface temperature and reduces the risk of maceration from moisture. Plastic bed liners should be avoided on these beds as the plastic obstructs the flow of the air and holds both heat and moisture against the patient’s skin. (Synergy® Air Elite Mattress Replacement System, Hill-Rom Services, Inc. Reprinted with permission. All rights reserved.)
FIGURE 6-9 Air-fluidized bed The air-fluidized bed, an integrated bed system, contains millions of silicone-covered beads that are continuously being blown by an air pump, thereby providing floatation to the patient. These beds are used for patients with multiple pressure ulcers, complex Stage III or Stage IV ulcers, or postsurgical repair with a flap. (Clinitron® II Air Fluidized Therapy Unit, Hill-Rom Services, Inc. Reprinted with permission. All rights reserved.)
Selection of the most appropriate support surface for the patient might be constrained by the hospital or care environment, but generally multiple options will exist. Informed decisions, of course, begin with an evaluation of the patient or client, but also must include basic knowledge of products.
Pressure ulcer risk evaluation is a natural place to start and is combined with assessment of function, including the patient’s ability to reposition in bed and the ability to transfer into and out of bed. Differences in features and design form the basis of an informed clinical decision that is best made by the multidisciplinary team involved in the patient’s care. Some support surface characteristics are technical in nature, such as the quality of component parts, warranty, expected lifespan, and maintenance requirements. For example, a support surface that requires periodic adjustment and maintenance may be appropriate in a facility with the capacity to handle those tasks, whereas it might not be a good choice in certain homecare environments, unless the patient and/or caregivers are comfortable in making those adjustments.
Support surfaces are designed to protect the skin and underlying tissues by allowing the patient to immerse or sink into the surface. Immersion redistributes pressures and envelops the body in an attempt to equalize external forces as much as possible. A support surface must be soft enough to allow immersion without bottoming out. Compliant support surfaces can deflect only so far before they cannot deflect further. This defines a “bottomed-out” state and results in high pressures on tissues. Because achieving an appropriate amount of immersion is so important, the optimal stiffness of the surface must take into account the patient morphology. A surface that is too firm will not allow the person to immerse, whereas one that is too soft might not afford a stable surface for functional mobility (eg, turning and moving in bed). Foam and gel materials generally have a fixed functional stiffness; thus, a surface with appropriate stiffness and thickness needs to be selected in order to provide requisite support. Surfaces using air typically offer adjustability, thereby allowing functional stiffness to be appropriately adapted for each patient. In both cases, reevaluation after selection must be done to insure that the support surface is properly configured to protect tissues and support the body.
Evaluating the Effectiveness of Support Surfaces
A large amount of research has focused on the effectiveness of support surfaces. Some use direct measures of clinical outcomes such as pressure ulcer incidence or time for pressure ulcers to heal. Others use indirect measures, including variables such as interface pressure, blood flow, and temperature. Both approaches have merit but report quite different information about support surface performance. An effective review of the literature requires an assessment of methodologies and devices with respect to how they apply to a particular situation. The patient population (eg, orthopedic, neurological), care environments (eg, ICU, homecare, long-term care), and types of support surfaces may impact how results influence care decisions. Notably, treatment studies—in which subjects already have ulcers—are fundamentally different from prevention studies. For the purpose of this chapter, a select number of comparisons are highlighted as a means to illustrate how studies are configured to investigate effectiveness. Several recent articles and documents have provided an overview of support surface research and can be referred to for more detailed information.12–15
Most studies compare different classes of products as defined in TABLE 6-3 rather than compare similarly designed products. For example, many more studies compare a standard hospital mattress to a specialty mattress instead of comparing two different types of low-air-loss beds. Moreover, studies tend to focus on a specific model from one manufacturer. It would be impossible to study all makes and models that exist in a single support surface category. Any study involving technology has the potential to become outdated simply because technology changes. This does not mean that historical studies have no value; instead it acknowledges the challenge of focusing solely on published literature to make clinical decisions and highlights the need to keep abreast of this ever-changing body of knowledge.
The most common research comparison is against a “standard” hospital bed or mattress. Even though there are differences in what constitutes a standard hospital mattress, the results are clear: standard mattresses are not very effective to prevent or to treat pressure ulcers. Non-powered, constant-low-pressure support surfaces (foam, air, gel, and combinations of these materials) are more effective in preventing pressure ulcers than a standard mattress.12–14 In fact, standards of practice recognize this by mandating the use of alternative surfaces in the plans of care for persons who are at risk for or already have pressure ulcers.
Studies comparing advanced active technologies including low-air-loss, alternating-pressure, and fluidized surfaces tend to find them to be equivocal in effectiveness.16–18 This offers evidence that these types of advanced support surfaces have roles to play in both prevention and treatment of pressure ulcers. Equivocal results should also motivate clinicians to read the literature in order to better understand the results and how the lack of significant results can also be clinically useful. For example, consider a comparison of two support surfaces in preventing pressure ulcers in a critically ill population.8 Sixty-two persons were enrolled and 9 of them developed pressure ulcers. The low incidence of pressure ulcers in this high-risk patient group resulted in an inability to detect differences in the two surfaces. Clearly, too few pressure ulcers are not a bad outcome, so the lack of a difference is still an important finding.
Protecting the Heels and Lower Extremities
For patients in bed, heels are particularly prone to pressure ulcers. This is not surprising if one reflects on the anatomy of the posterior aspect of the heel, the portion in contact with the support surface, and the amount of both direct pressure and friction that occurs at the heel. (FIGURE 6-2) The calcaneous forms a small, narrow prominence that must bear the weight of the foot and part of the leg when the patient is supine. Even though the foot is a small mass, the small surface area results in damaging pressure. In fact, the heel is often cited as the second most common site for ulcers, accounting for 25–30% of pressure ulcers.19,20
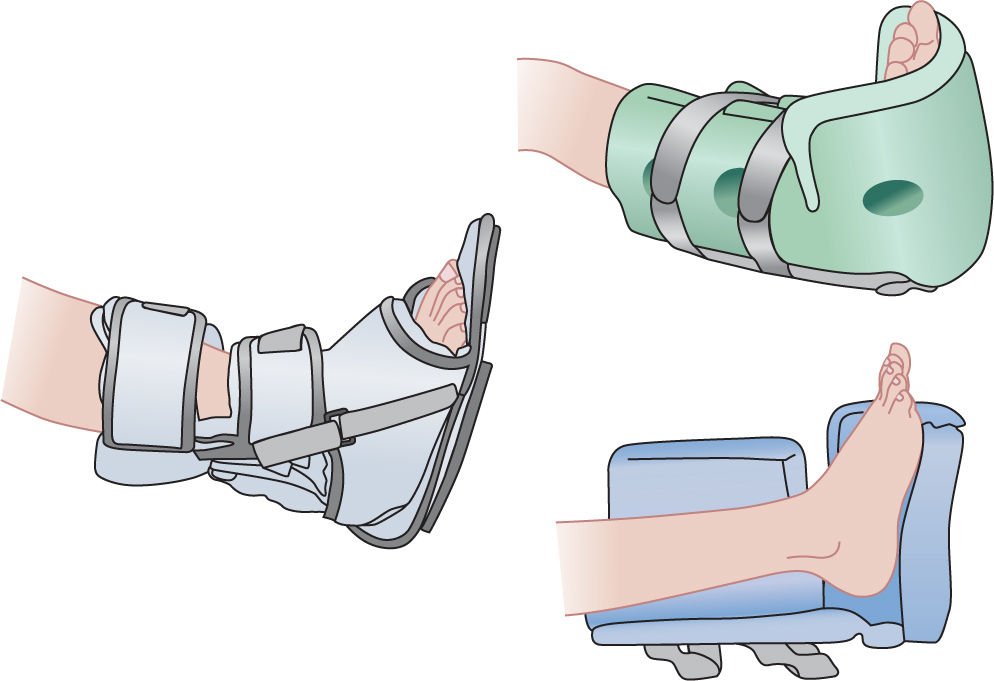
Many commercial devices and approaches are available to reduce or eliminate pressure on the heels. Mattresses and overlays are often designed to support the heels using softer materials or different designs than those used to support the rest of the body. Two additional types of devices are available: (1) user-worn boots or heel protectors, and (2) positioners to elevate the heels.
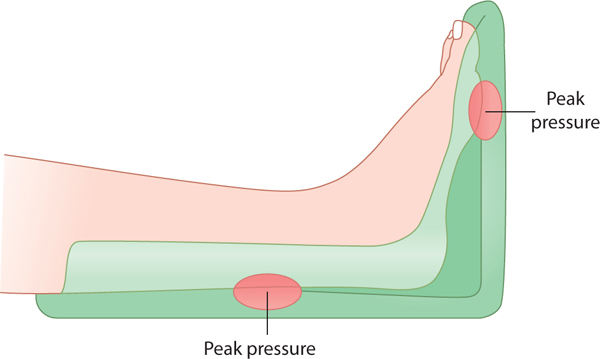
The user-worn approach consists of a boot or pad that encases the foot and heel and attaches directly to the person. (FIGURES 6-10 to 6-12) These can be made from air bladders, foam, gel, or sheepskin materials. These devices remain in place during changes in positioning and as the legs move in bed; therefore, the fit and securement must be assessed. Most user-worn devices help prevent the ankle from plantar flexing (aka, foot drop) and some are designed to keep the ankle and foot aligned even in the presence of tone or spasm via the use of a rigid shell. If, however, the patient already has a plantar flexion contraction, the rigid support is contraindicated because peak pressures will occur at the plantar metatarsal heads and the Achilles tendons, causing the pressure ulcers in these areas. (FIGURE 6-13) Ambulation while wearing heel boots and pads is typically contraindicated (unless there is an ambulation sole attached); thus, these devices are not recommended when encouraging patients to transfer out of bed independently. Many studies have documented interface pressure and other outcomes about various products. Reviews of these studies are often useful;21–24 however, clinicians should read the primary source when using the results of a specific study to determine clinical decisions.

FIGURE 6-10 User-worn heel protector The Rooke boot is made of pliable sheepskin-like material that can be worn in bed and for limited ambulation. It is available with a rigid frame to maintain ankle range of motion and without a frame to accommodate plantar flexion contractures.
FIGURE 6-11 Rigid ankle-foot orthotic with heel relieved of any contact, both in supine and standing positions
FIGURE 6-12 Foam boots with suspended heels
FIGURE 6-13 Plantar flexed ankle A plantar flexed ankle that cannot be passively stretched to neutral placed in a rigid AFO will have peak pressures at the metatarsal heads and the Achilles tendon, thus putting these tissues at risk for pressure ulcer formation. Some AFOs have adjustable ankle joints to adapt to plantar flexion contractures.
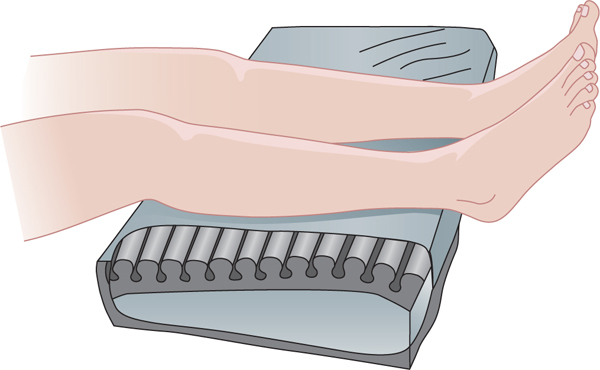
The other category of heel protection is achieved by elevating (or floating) the heels completely off the surface by placing a positioning pad or pillow under the calf. Although some may extend to the knee, caution is advised with orthopedic patients when support under the knee may lead to knee flexion contractures (eg, after a total knee replacement). Several products can be purchased to provide heel elevation function (FIGURE 6-14) and are made from inflatable bladders or foam. Regular head pillows can be used to elevate the heels; however, they have been shown to be less effective because they compress and get out of position more easily.14 (FIGURE 6-15) Heel elevation devices do not necessarily accommodate changes in position and therefore must be assessed whenever a person returns to a supine posture or moves the legs. In addition, care must be taken not to elevate the foot in a manner that induces hyperextension at the knee, which will become uncomfortable. Any lower extremity positioning approach should be done after assessing ranges of motion at the hip, knees, and ankle to insure that external positioners maintain appropriate joint positions.
FIGURE 6-14 Heel and foot elevating pad Pads under the calves are effective in off-loading or floating the heels; however, they may be displaced as the patient repositions. Care must be taken to avoid prolonged pressure on the posterior calf if the patient is insensate or atrophied (eg, a patient with spinal cord injury).
FIGURE 6-15 Pillows used to off-load the heels When commercial devices are not available or not adaptable to a patient, pillows can be used creatively to accomplish pressure redistribution. This patient has bilateral foot drop and also tended to slide down in bed, putting the plantar metatarsal heads at risk. A pillow under the calves floats the heels and a folded pillow between the feet and the end of the bed offloads the plantar surfaces. While improvisations may not be ideal, they can be effective when combined with frequent repositioning.
Positioning people in varying degrees of side-lying requires padding and positioners to insure bony prominences are adequately protected. (FIGURE 6-16) The malleoli and knees can be subjected to high pressures when in side-lying. These issues are discussed in the section on recumbent postures.
FIGURE 6-16 Thirty-degree side-lying posture Thirty-degree side-lying posture uses a foam wedge for positioning and pillows under the arms and legs and between the knees to protect bony prominences of all extremities and the sacrum. Folded pillows may be used behind the back and sacrum if foam wedge is not available. (Used with permission of Stephen Sprigle PT, PhD.)
Wheelchairs and Wheelchair Cushions
People who use wheelchairs are as varied as people who ambulate. They exhibit a wide range of medical diagnoses, but share the functional limitation of being non-ambulatory or unable to ambulate functionally or safely. Because many wheelchair users sit throughout the day, many are at risk of developing pressure ulcers. Wheelchair users are assessed with respect to two common pressure-ulcer risk factors, immobility and sensation. Persons who are unable to recognize pain or discomfort while sitting are naturally at high risk for developing ulcers. Similarly, persons unable to move in their seat or to shift weight and correct posture are also at heightened risk. In both cases, these wheelchair users will be unable to recognize when damaging loads are placed on their skin and subcutaneous tissues.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree