How are vascular anomalies classified?
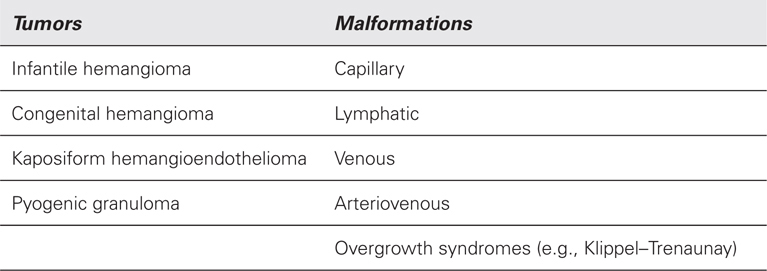
Lesions are divided into tumors and malformations.
 What is infantile hemangioma?
What is infantile hemangioma?
A benign tumor of endothelial cells.
 How common is infantile hemangioma?
How common is infantile hemangioma?
It is the most common tumor of infancy; 4% to 5% of Caucasians are affected.
 What does infantile hemangioma look like?
What does infantile hemangioma look like?
Red; but deeper lesions under the skin may appear bluish.
 What tissues are affected by infantile hemangioma?
What tissues are affected by infantile hemangioma?
Skin and/or subcutaneous tissue of the head and neck (60%), trunk (25%), or extremity (15%). The liver is the most common visceral location.
 Are there risk factors for infantile hemangioma?
Are there risk factors for infantile hemangioma?
Yes. The tumor is more common in females (4:1), premature infants, and Caucasians.
 Is infantile hemangioma present at birth?
Is infantile hemangioma present at birth?
No, although some infants may have a telangiectatic stain, pale spot, or ecchymotic area.
 When is infantile hemangioma first noted?
When is infantile hemangioma first noted?
Usually, within the first 2 weeks after birth; lesions beneath the skin may not be obvious for a few months.
 What is the life cycle of infantile hemangioma?
What is the life cycle of infantile hemangioma?
It grows for the first 3 to 9 months of age and then slowly regresses.
 When does infantile hemangioma stop improving?
When does infantile hemangioma stop improving?
Lesions typically stop involuting by 3.5 years of age.
 Does infantile hemangioma completely go away?
Does infantile hemangioma completely go away?
Not usually, in at least 50% of children telangiectasias, damaged skin, destroyed structures, or fibrofatty tissue remains.
 Can an infant have multiple infantile hemangiomas?
Can an infant have multiple infantile hemangiomas?
Yes, 20% have more than one lesion.
 Can multiple lesions be problematic?
Can multiple lesions be problematic?
Yes, patients with more than five small, dome-like tumors are at risk for having a hepatic hemangioma.
 How is infantile hemangioma diagnosed?
How is infantile hemangioma diagnosed?
History and physical examination.
 Does infantile hemangioma require treatment?
Does infantile hemangioma require treatment?
No. 90% of lesions are allowed to enlarge and regress without intervention.
 When is intervention indicated for a proliferating infantile hemangioma during infancy?
When is intervention indicated for a proliferating infantile hemangioma during infancy?
If a tumor is causing functional problems (i.e., blocking the visual axis or airway), or is at risk for leaving a significant deformity (large lesion on the face).
 What is the first-line intervention for a small, localized problematic infantile hemangioma?
What is the first-line intervention for a small, localized problematic infantile hemangioma?
Lesions ≤3 cm in diameter can be injected with corticosteroid (triamcinolone 40 mg/mL) not to exceed 3 mg/kg per injection.
 How effective is corticosteroid injection?
How effective is corticosteroid injection?
All lesions will stop growing, and two-thirds will become smaller.
 What is the intervention for a problematic infantile hemangioma that is too large to inject with corticosteroid?
What is the intervention for a problematic infantile hemangioma that is too large to inject with corticosteroid?
Oral pharmacotherapy with either prednisolone (3 mg/kg) or propranolol (2 mg/kg).
 What are the advantages and disadvantages of prednisone therapy?
What are the advantages and disadvantages of prednisone therapy?
~100% response rate (10% will stop growing and 90% will become smaller), safe, minimal monitoring, and no long-term side effects.
 What are the advantages and disadvantages of propranolol therapy?
What are the advantages and disadvantages of propranolol therapy?
10% nonresponse rate, long duration of treatment, may have greater initial shrinkage of the tumor compared to prednisone, more complicated monitoring for bradycardia, hypotension, hyperkalemia, and hypoglycemia.
 Is resection of a problematic infantile hemangioma generally recommended in infancy?
Is resection of a problematic infantile hemangioma generally recommended in infancy?
No. Operative morbidity is high while the tumor is vascular and rapidly growing.
 What is the ideal time for operative intervention?
What is the ideal time for operative intervention?
Between 3 and 4 years of age. At this time the tumor has completed involution, become less vascular, and decreased in size. Resection is still performed before long-term memory and self-esteem begin.
 What are the indications for operative intervention?
What are the indications for operative intervention?
Damaged or excess skin, injured anatomic structures, fibrofatty residuum, and residual telangiectasias.
 Should laser therapy be used to treat a cutaneous infantile hemangioma during infancy?
Should laser therapy be used to treat a cutaneous infantile hemangioma during infancy?
No, laser does not stop the growth of the tumor and increases the risk of ulceration.
 Should laser be used to treat an infantile hemangioma after it has involuted?
Should laser be used to treat an infantile hemangioma after it has involuted?
Yes, pulse-dye laser can effectively eliminate residual telangiectasias in childhood.
 What is a congenital hemangioma?
What is a congenital hemangioma?
A hemangioma that is fully grown at birth and does not enlarge postnatally.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


