Key points
- •
The use of barbed sutures to suspend non-dissected soft tissue requires placement of several sutures and the degree and duration of the correction are limited
- •
Bi-directional absorbable barbed sutures allow correction of all three thirds of the aging face when the soft tissues are properly dissected.
- •
The brow can be adjusted and shaped by a one-to-one correction that is achieved with barbed sutures that exit the lowest brow hairs.
- •
The midface can be supported at the subperiosteal plane with placement of bi-directional absorbable barbed sutures for reliable repositioning of ptotic midface soft tissue.
- •
Midline platysma contouring and lateral platysmal advancement are easily achieved with the placement of bi-directional absorbable barbed sutures.
Introduction
The placement of barbed sutures at the subcutaneous plane was an early application of this technology. Failure to achieve long-term correction with this technique (inability of the sutures to hold non-dissected soft tissue in an elevated position) stimulated the development of procedures and suture materials that apply to all levels of the soft tissue of the face. Therefore, the evolution of barbed suture technology has advanced to the current availability of a variety of absorbable and non-absorbable bi-directional barbed sutures that have applicability to the upper, middle, and lower-thirds of the aging face. As is true with all facial aesthetic plastic surgical procedures, an understanding of the two major components of the aging face is mandatory for proper procedure selection. Achieving a harmonious facial rejuvenation requires attention to proper vectors and to volume replacement. To achieve a long-lasting correction, tissues must be dissected at various levels and supported in their new position with the bi-directional barbed sutures. Applied in this way, the result that is obtained is predictable and long-lasting. In some cases, minimally invasive applications of this technology provide a satisfactory, long-lasting result. Most cases, however, require more aggressive surgical maneuvers to achieve and to maintain the desired result.
Patient selection
Although there are indications for the pure placement of barbed sutures in the subcutaneous plane, with or without a modest undermining, correction is variable in duration. My experience with this technique, i.e., solely placing the sutures subcutaneously, is that it only works in young patients with minimal soft tissue ptosis of the midface and neck. Elevation of the malar fat pad in young patients with good quality of soft tissue and excellent malar projection can be maintained for 6–12 months or longer. However, patients with more significant midface ptosis and loss of volume require a more aggressive undermining of the soft tissues combined with proximal fixation to a non-mobile, anatomical structure, and volumetric augmentation of the tear trough, malar, and/or submalar areas. My experience has also taught me that I can achieve reliable correction of early loss of definition of the sub-jaw area by combining ultrasonic assisted liposuction and limited undermining with a blunt cannula along with the placement of absorbable barbed sutures close to the dermis to accentuate the mandibular border. In most cases, the pure placement of barbed sutures in the subcutaneous or subgaleal plane of the forehead will not maintain the corrected, elevated position of the brow, without undermining the soft tissue. A muscle relaxant (such as Botox® Cosmetic, Allergan, Inc., Irvine, CA) is required to maintain the position of the elevated brow when only subcutaneous threads are used, which begs the question: why use threads at all if satisfactory elevation of a few millimeters can be achieved with botox alone?
Indications
Bi-directional barbed sutures may be used in correcting soft tissue ptosis in the upper, middle, and lower thirds of the aging face.
Upper third indications
Most patients (mainly female) who exhibit brow ptosis with or without upper eyelid hooding can achieve long-lasting elevation of the brow when the barbed sutures are utilized to shape and to hold the brow following adequate soft-tissue mobilization. Asymmetric brows, typically very difficult to correct, can be improved with the placement of barbed sutures as well as incorporating post-operative adjustment of the brow as described below. Although applicable in men, limited undermining of heavy, ptotic, forehead tissues will usually not achieve significant long-term correction, unless only modest elevation is desired (which it typically is). Even so, heavy tissues seem to resume their ptotic position unless more aggressive maneuvers are utilized such as an open-coronal forehead lift, aggressive endoscopic soft tissue release, or direct excision of forehead skin in an existing forehead rhytid or above the brow. The later indications are rare and modest elevation can be achieved with a transblepharoplasty browlift.
Middle third indications
Men and women aged 35 years and older may be candidates for midface elevation utilizing barbed sutures. Although young patients may achieve modest midface elevation with the placement of subcutaneous threads combined with limited subcutaneous undermining, most patients require a more aggressive approach that includes soft tissue undermining at several planes with or without the simultaneous addition of volume (autologous or non-autologous). Patients with the following clinical findings are appropriate candidates for utilizing the subperiosteal approach for middle third facial correction:
- •
Long faces.
- •
Full or flat malar eminences.
- •
Moderate to marked tear trough deformities.
- •
Periorbital hollowing.
- •
Elongation of the lid-cheek junction.
- •
Prominent nasolabial folds.
- •
Volumetric loss of bone and soft tissue of the malar and/or submalar zones.
Typically, suitable candidates have more than one of the above findings. In youth, the long axis of the orbit is horizontal. With aging, the long axis rotates 90 degrees to a vertical direction. An essential finding in patients who are candidates for a midface lift is descent of the lid/cheek junction. Although this movement may be an illusion and in reality represents only a loss of soft tissue volume (Lambros’s theory), the correction, as mentioned above, may require both vector and a volume based maneuvers.
Unsuitable candidates for a subperiosteal midface lift utilizing barbed sutures include:
- •
Patients with thin skin and little subcutaneous tissue (barbs may be palpable and/or visible, but dissolve with time).
- •
Patients with severe sun-damaged skin (these tissues simply do not hold sutures well and relapse may occur).
- •
Patients who are obese and have very heavy, ptotic, soft tissues (holding the correction may be less successful due to the load on the sutures).
- •
Patients with a wide interzygomatic distance , very full malar eminences, and very little soft tissue descent (these patients will show a widening of the interzygomatic distance after a subperiosteal midface lift due to the lateral reset of the origins of the zygomaticus major and minor muscles).
- •
Patients who have undergone a midface lift and present with unknown degrees of deep facial soft tissue scarring (the dissection may be hazardous and the result less predictable).
- •
Patients with unrealistic expectations (even with an acceptable result, these patients may be unhappy).
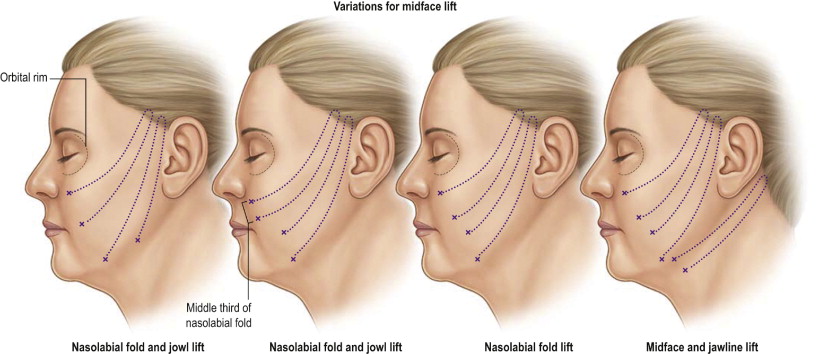
The middle third of the aging face can be corrected via a lateral approach that requires a high-SMAS resection, plication or a combined undermining and resection at the deep plane to elevate the midface along with the lateral cheek. Incorporating barbed sutures in these procedures (MACS lift, SMAS and malar fat pad plication, lateral SMASectomy, high SMAS dissection, or a composite rhytidectomy) requires very little operating time, avoids the ‘purse-string’ effect on the elevated tissues and requires less suture material to achieve the correction.
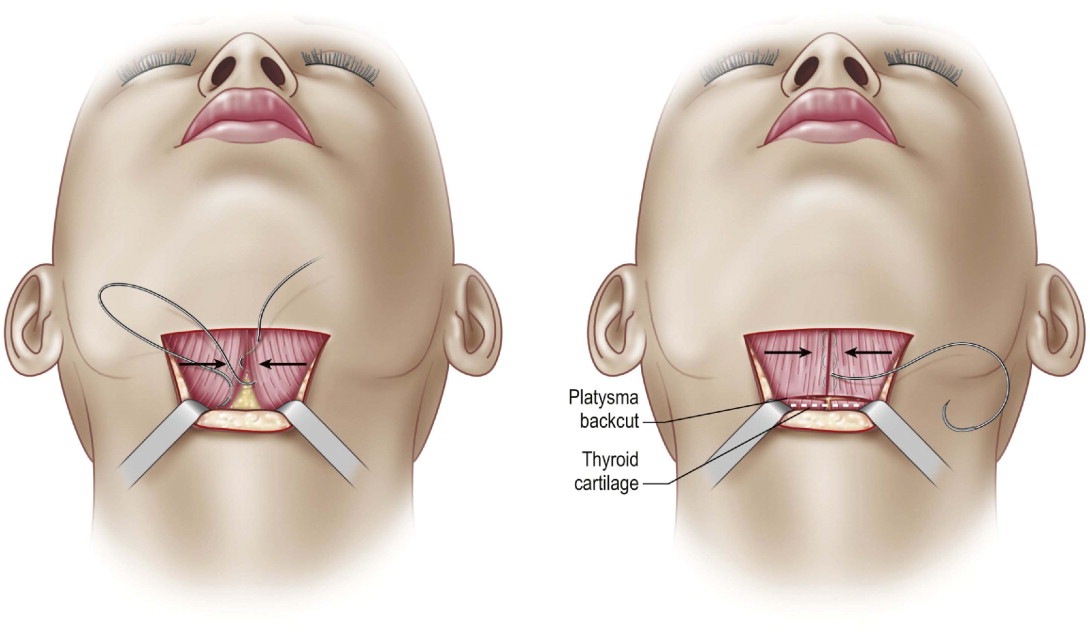
Lower third indications
Correction of the middle third via a lateral approach will, of course, improve some of the changes observed in the lower third. However, whether one chooses to use a technique of SMAS plication, lateral SMASectomy, composite rhytidectomy or other manipulations, the Quill SRS barbed sutures can be used to expedite the closure and avoid the tying of knots when an oblique or linear closure is performed. One of the exciting indications for the bi-directional barbed suture technology is the use in contouring the subjaw area which includes a ‘corset platysmaplasty’ and/or lateral contouring. Patients who do not exhibit platysma bands may be improved with submental liposuction and the placement of subcutaneous threads after ultrasonic assisted liposuction from the infralobular approach and the submental approach. Patients who exhibit short platysmal bands require open neck dissection and lateral plication of the platysma to the mastoid fascia with two Quill bi-directional sutures (liposuction may be needed as well). Patients who exhibit long platysmal bands that may reach from the mandible to the clavicles are best treated with closed liposuction followed by a full midline platysmaplasty utilizing the Quill bi-directional suture with or without a backcut at or below the thyroid cartilage for optimal contouring.
Operative technique
Pre-operative preparations
As is true with all facial aesthetic plastic surgical procedures, obtaining an optimal result is dependent upon careful clinical analysis and selecting the most appropriate technique(s). The use of computer imaging, although clearly not a guarantee of obtaining the result seen on the computer, is a valuable tool in showing the patient his or her pre-existing asymmetries and is helpful in understanding what the patient wants to achieve with the surgical procedure(s). Deciding on the need for soft tissue or bony augmentation with the use of alloplastic and/or autologous materials is an important discussion point. Showing the patient his or her deficient midface volume and or a short mandible will educate the patient concerning the need for adding volume to achieve a harmonious, youthful appearance. Reviewing photos from youth (frontal and oblique, if available) will provide an opportunity to know whether the patient wants to return to his or her youthful appearance, or wants to achieve a different look (typically patients with insufficient malar projection, submalar fullness, and or projection of the mentum). I digitize the important photos, add them to the patent’s digital file, print them along with the current photos, bring them to the operating room, and refer to them frequently as I work my way through the procedures.
Patients are always seen twice before the surgical procedure, firstly in an initial consultation and secondly on the pre-operative visit, to answer any questions or concerns. All patients are instructed to discontinue any medications that may affect coagulation and any form of herbal medications and diet pills. Smokers are warned of the dangers in terms of delayed wound healing, unfavorable scarring, pulmonary issues, etc., related to smoking. Certainly, patients who state that they have stopped smoking at least 2–3 weeks before surgery pose risks and I, therefore, perform more limited subcutaneous undermining, relying on extensive subSMAS dissection to obtain a healthy fascio-cutaneous flap. Appropriate laboratory screening tests and medical clearance is obtained as indicated by the patient’s age, medical history, length of planned procedures, etc. Patients use an iodine containing soap when showering and shampooing the night before and the morning of surgery.
All marking are made in the pre-operative area and I frequently provide a mirror to allow the patient to visualize and to agree to the proposed incision lines, areas of undermining, vectors of correction, and areas chosen to receive fillers or facial implants ( Figure 6.1 ). This discussion should be a part of the dictated operative report. For applying the markings for a browlift utilizing an endoscope, the proposed high point of the brow is transferred to a vertical incision behind the anterior hairline. The temporal access incision is determined by placing a ruler from the ala to the tail of the brow ending behind the temporal hairline. A 3–4 cm incision is planned obliquely about 1 cm behind the hairline, lateral to the anterior temporal crest. If a modification of the central depressors of the brow is indicated, this may be accomplished either via a transpalpebral incision or with an endoscope passed from a 1.5 cm transverse incision behind the anterior hairline. If a midface lift is planned, the pathways of the two or three planned thread placements are marked with parallel lines that are drawn between the cheek lateral to the nasolabial crease ending about the middle of the temporal access incision. If a face and a necklift is planned, the incisions are drawn in the usual manner (transversely at the sideburn, retrotragal, retroauricular, and into the hair bearing scalp). I rarely if ever use a short scar approach. With proper placement and closure with attention to realigning the hairline, the scar is rarely if ever a problem and this approach allows better visability and avoids any pleating behind the ear. The platysma bands, if present, are marked in their entirety as is the planned submental incision 2 mm for closed liposuction or 3–5 cm for an open lipectomy and platysmaplasty.
The proposed level of back-cut of the platysma is marked as is the lowermost line of dissection. This line is connected with the post-auricular incision. The anteriormost line of dissection of each cheek is marked. Areas selected for soft tissue or bony augmentation are marked as well. Male patients and borderline or known hypertensive females are given 0.2 mg of clonidine p.o. before surgery and have a clonidine patch applied for continuous release of anti-hypertensive medication for 5–6 days. This medication also reduces the required amount of anesthesia. Patients with a history of nausea and/or vomiting are given 40 mg of Emend (Merck Pharm., Inc.) several hours pre-operatively. This single tablet will, in most cases, prevent post-operative nausea and/or vomiting for 72 h which is important for patient comfort and to reduce the risk of hematoma formation.
Techniques
When performing procedures in the upper, middle, and/or lower thirds of the aging face, the following steps occur:
All patients are operated upon utilizing general endotracheal anesthesia supplemented with a generous infiltration of local anesthesia. Standard 1% lidocaine with epinephrine 1 : 100,000 (Astra Pharm) is infiltrated along the proposed incision lines as well as the anterior temporal crest and, as indicated, the glabella and the superior orbital rims. I limit the amount of 1% lidocaine and epinephrine 1 : 100,000 to a maximum of 20 mL and only inject each area before I begin working in that area to avoid absorption of a large amount of solution which may cause lidocaine toxic effects as well as hypertension and arrhythmias. A superwet infusate containing 500 mL of lactated Ringer’s solution, 30 mL of 1% lidocaine plain, 1 mL of epinephrine, and 10 mg of triamcinolone is infused under pressure utilizing a liposuction infiltration pump, after prepping and draping of the patient. This also prevents untoward events related to the volume of local anesthesia and epinephrine that is injected. This solution therefore contains lidocaine 0.06% and epinephrine 1 : 500,000 with a very small amount of cortisone for its anti-inflammatory effect.
A standard facelift tray of instruments is provided and the following instruments are added:
- •
Periosteal elevators (short and endoscopic).
- •
Short and long army-navy retractors.
- •
An Aufricht retractor with or without fiberoptic lighting (for use through a temporal access incision).
- •
An endoscopic setup if more than a temporal browlift is planned (camera, 30 degree angled endoscope, endoscopic scissors and grasper, long insulated cautery, suction and irrigation).
- •
A Xomed bone-bridge (Meditronic Xomed Corp, Jackson-Ville, FL) for drilling a cortical tunnel if correction of a ptotic brow requires a more medially placed access incision for passing the barbed-sutures.
- •
Quill SRS unidirectional or bi-directional absorbable barbed sutures, 0 and 2-0 PDO (polydioxanone).
The eyes are protected with an aqueous based lubricant (Merocel®) and disposable corneal protectors. Small pledgets of Xeroform® gauze (Invacare Inc.) are placed in each ear canal. If I am planning to perform a subperiosteal midface lift which will incorporate an intraoral incision, I cleanse the upper gingival-buccal sulcus with povidone iodine solution and lay a povidone iodine solution soaked 4 × 4 gauze over the sulcus to prevent bacterial contamination through this incision. A full face prep with povidone iodine scrub is performed and the endotracheal tube is prepped into the field with povidone iodine solution, and wrapped with a sterile towel which is held in place with staples. Patients receive intermittent compression devices applied to both calves. Patients are given 1 g of a cephalosporin (if not allergic to penicillin) intravenously, and 10 mg of dexamethasone IV push before receiving the injections of local anesthesia. Dexamethasone is given to overnight patients every 8 h for 2–3 more doses of 4 mg each and patients are given a Medrol DosePak and a cephalosporin to be taken orally for 6 days. I always begin with the neck and work my way superiorly for two reasons:
- •
I like to see the soft tissues stack in the superior and oblique directions. Many times, I have achieved significant midface correction with an aggressive subSMAS dissection and I, therefore, do not need to perform a subperiosteal midface lift to obtain the correction that I envision.
- •
The most likely place for development of a hematoma is in the post-auricular area and/or the neck. By performing the necklift first, I have the opportunity to examine the neck after I complete the other procedures (assuming I am performing more than a necklift from a submental and a retroauricular incision without a facelift)
Technique for a necklift
Limited access necklift
- •
I begin with closed liposuction (when excess submental fat and mandibular or submandibular fat is present) using a 2.4 mm flat, single hole spatula cannula.
- •
When planning an open platysmaplasty, I make a 3–4 cm incision 3–5 mm posterior to the submental crease and dissect as low as my pre-operative skin markings.
- •
I examine the platysma and its overlying fat as well as the interplatysmal and subplatysmal fat which, of course, is specific to the clinical findings in each patient. The planned resection of excessive fat requires that I leave about 3–5 mm of fat on the flap to prevent irregular skin contour and/or adhesions between the dermis and the platysma muscle.
- •
I begin the midline platysmaplasty by inserting one end of the Quill SRS bi-directional suture lateral to one edge of the platysma muscle after freeing the edges of both muscles. I invert the sutures to prevent the development of a palpable seam.
- •
I continue passing the suture from one edge to the other until I reach the bottom of the planned plication (which I marked pre-operatively on the skin of the central neck), return the suture under the last two passes, and gradually apply tension on the suture which allows the barbs to engage the soft tissue. This provides for enhanced ability to contour the muscle and to shorten the muscle which improves the cervico-mental angle ( Figure 6.2 ). There is no need to tie any knots which avoids several potential problems: