7 Urodynamics: Cystometry and Urethral Function Tests
The term urodynamics means observation of the changing function of the lower urinary tract over time. Two principal methods of urodynamic investigation are known. Conventional urodynamic studies take place in the urodynamic laboratory and involve filling the bladder via a catheter, usually at a specified rate. Ambulatory urodynamic (AUD) studies are defined as a functional test of the lower urinary tract, using natural filling and thus reproducing the subject’s everyday activities. Urodynamic tests have been slow to achieve acceptance and are by no means universally used; however, in recent years there has been a resurgence of interest in the hydrodynamic and neurophysiologic aspects of the storage and evacuation of urine. An abundance of new diagnostic procedures, methodologies, and testing equipment has made it exceedingly difficult for the clinician to decide what tests are necessary to adequately evaluate lower urinary tract dysfunction in women.
Results of urodynamic investigations should be recorded in a way that can be communicated among physicians and other health care personnel. For this reason, the recommendations detailed in the standardization reports of the International Continence Society (ICS) should be followed (see Appendices A and B).
Chapters 7 and 8 discuss urodynamic modalities used in the evaluation of filling, storage, and evacuation of urine. The intent is to give the reader a clear understanding of the rationale, technique, use, and limitations of each test.
PRINCIPLES OF CYSTOMETRY
The first cystometer dates back to 1872 when Schatz accidentally discovered a crude technique for measuring bladder pressure while trying to record intra-abdominal pressure. Shortly thereafter, in 1876, DuBois studied the effects of changes in body position on intravesical and intrarectal pressures and observed that the desire to void was associated with contraction of the detrusor muscle. The currently popular water cystometer was designed by Lewis in 1939. The later use of air and carbon dioxide as filling media further simplified the procedure.
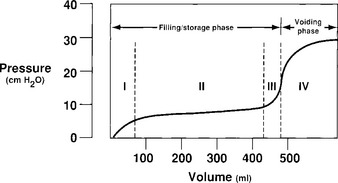
A cystometrogram has two phases: a filling/storage phase and an emptying (voiding) phase (Fig. 7-1). The filling phase is subdivided into a brief initial rise in pressure to achieve resting bladder pressure, followed by a tonus limb that reflects viscoelastic properties of accommodation of the smooth muscle and collagen of the bladder wall. There may be a third increase in the pressure, which is attributed to the stretching of detrusor muscle and collagenous elements of the bladder wall beyond their limits at bladder capacity. During this third stage, the patient is still able to suppress voiding. A detrusor contraction is then initiated voluntarily in conjunction with a relaxation of the outlet, and the patient voids.
STANDARDIZED TERMINOLOGY AND NORMAL CYSTOMETRIC PARAMETERS
The ICS has recently redefined certain terms that are used in the reporting of cystometric results.
A female bladder normally experiences a first desire to void at a volume of approximately 150 to 250 mL, a normal desire to void at 300 to 400 mL, and a strong desire to void at 400 to 600 mL. During filling, an initial rise in true detrusor pressure between 2 and 8 cm H2O usually occurs. The average pressure rise is approximately 6 cm H2O and normally never exceeds 15 cm H2O. Provocation of a normal bladder by rapid filling, change of posture, coughing, or catheter movement should not incite any abnormal rises in detrusor pressure.
EQUIPMENT
A discussion of all commercially available cystometers is beyond the scope of this chapter, but reviews by Blaivas (1990) and Rowan et al. (1987) provide an overview of available urodynamic machines. The simplest cystometer is a water manometer connected by a Y tube to both a reservoir and a catheter. A variation of this technique is discussed in Chapter 5.
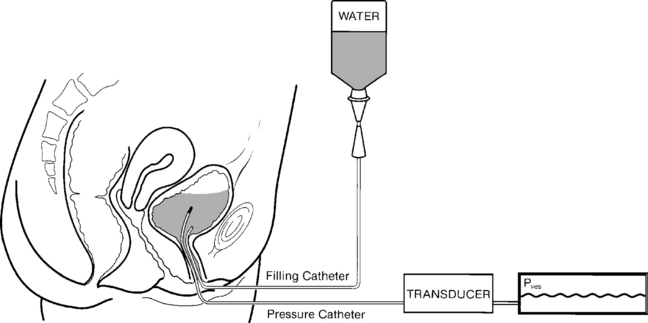
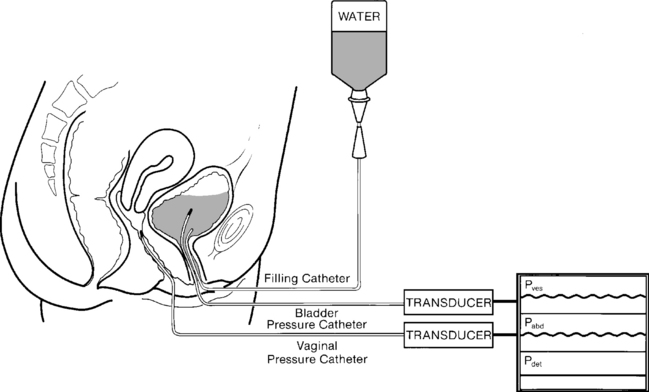
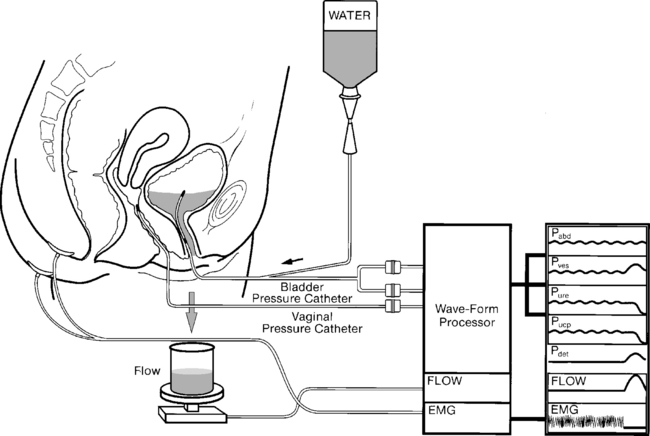
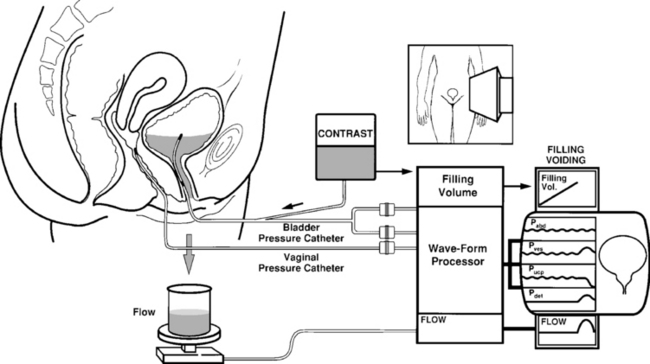
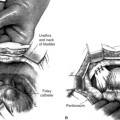
Commercially available cystometers can be broadly classified into single-channel and multi-channel machines (subtracted cystometry). Single-channel cystometry involves the placement into the bladder of a pressure-measuring catheter that produces an electronic signal, creating a graph on a recording device (Fig. 7-2). Multichannel cystometry relies on the measurement of both abdominal (Pabd) and intravesical pressures (Pves), thereby enabling one to distinguish changes in intra-abdominal pressure from changes in intravesical pressure (Fig. 7-3). Abdominal pressure can be measured via either transrectal or transvaginal catheters or less commonly from extraperitoneal pressure or a bowel stoma. We prefer vaginally placed catheters because they are more comfortable and easier to clean and maintain, and measurements are not cluttered by rectal peristalsis. Electronic subtraction of intra-abdominal from intravesical pressure allows for the calculation of true detrusor pressure (Pdet).
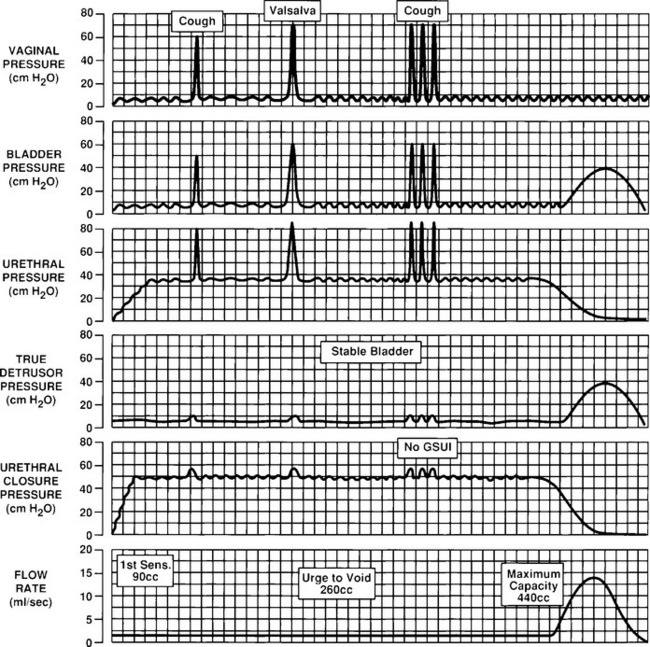
Subtracted cystometry may be enhanced further by additional measurement of urethral pressure (Pure). This measurement allows for the calculation of urethral closure pressure (Pucp), which is the difference between urethral and bladder pressures. Certain machines also allow for the simultaneous measurement of EMG activity and the performance of flow studies (Fig. 7-4). These standard urodynamic techniques may be combined with videocystourethrography, which is termed video urodynamics.
METHODOLOGY
Filling Media
The commonly used infusants for cystometry include water, carbon dioxide, and radiographic contrast material. In 1971, Merrill et al. introduced the use of carbon dioxide (CO2). Although once popular in North America, it is rarely, if ever, used for the following reasons: (1) It further decreases the physiologic nature of the test; (2) if gas is used, the bladder volume cannot be assessed because CO2 is compressible; (3) CO2 dissolves in urine to form carbonic acid, which irritates and reduces cystometric bladder capacity; (4) abdominal pressure is not usually measured during CO2 cystometry, making interpretation more difficult; and (5) when CO2 is used for filling cystometry, it is impossible to perform a stress test or voiding studies.
Types of Catheters
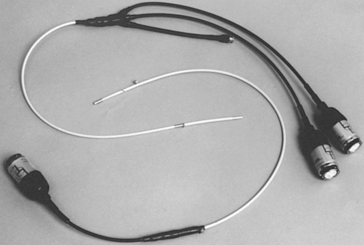
Various catheters have been used for cystometry. Simple or manual cystometry can be performed with a transurethral Foley catheter. Electronically monitored studies require more sophisticated balloon or microtransducer catheters. Water-filled balloon catheters or water perfusion catheters have been used with moderate success. These catheters are inexpensive, disposable, and easy to use. However, more sophisticated laboratories usually use sensitive microtransducer catheters (Fig. 7-5). These catheters are available with one to six microtransducers on the catheter. They have small diameters, are flexible, and can measure accurately rapid changes in pressure during repetitive coughing or other provoking maneuvers. Disadvantages include their expense, their need to be replaced after approximately 100 studies, and their tendency to produce rotational artifacts; pressure readings may vary depending on the orientation of the transducer to the bladder or urethral wall.
Technique of Cystometry
The technique of subtracted urethrocystometry used in our laboratory is as follows:
INDICATIONS FOR CYSTOMETRY
Indications for single-channel cystometry versus subtracted or multichannel cystometry have been debated extensively; however, few comparisons exist in the literature. One study by Ouslander et al. (1987) reported a sensitivity of 75% in geriatric patients undergoing simple supine cystometry when compared with multichannel testing. Sutherst and Brown (1984) compared single-channel and multichannel urodynamics in a blinded crossover study of 100 incontinent women. They noted single-channel studies to be 100% sensitive and 89% specific compared with multichannel studies. Multichannel cystometry may have a higher sensitivity for recognizing low-pressure detrusor contractions. Multichannel techniques also improve the specificity of cystometry by avoiding false-positive test results created by increases in abdominal pressure. Whether the cost of multichannel testing is justified for most patients remains to be proved. Box 7-1 lists suggested indications for subtracted cystometry.
BOX 7-1 INDICATIONS FOR MULTICHANNEL SUBTRACTED CYSTOMETRY
Inconclusive single-channel studies
Stress incontinence before surgical correction
Urge incontinence not responsive to therapy
Recurrent urinary loss after previous surgery for stress incontinence
Frequency, urgency, and pain syndromes not responsive to therapy
Nocturnal enuresis not responsive to therapy
Lower urinary tract dysfunction after pelvic radiation or radical pelvic surgery
VIDEO–URODYNAMIC TESTING
Video-urodynamic studies of the lower urinary tract represent a combination of video-cystourethrography and standard urodynamic techniques. Video-urodynamics requires equipment for cystometry, plus an image intensifier and a videotape recorder. In addition, various interface modules are necessary, depending on the exact design of the system. A television camera positioned above the recorder with a mixing device projects the recording channels on a television monitor alongside the radiographic image of the bladder (Fig. 7-7). Radiopaque-filling medium is used for video-urodynamic studies. As with all other urodynamic studies, every effort must be made to limit the inhibitory effect of the additional machinery and personnel imposed on the patient.
AMBULATORY URODYNAMICS (AUD)
The technique for performing AUDS, as described by Abrams (1997), involves the recording of three micturition cycles: a resting cycle, when the patient sits in a chair; an ambulant cycle, when the patient moves around the hospital; and an exercising cycle, which should include any specific incontinence-provoking measures. Once the three cycles are recorded, the information is downloaded to a computer for analysis. This analysis is time-consuming and requires considerable expertise.
Besides providing objective evidence and the cause of the patient’s lower urinary tract symptoms, additional interesting information is being generated by AUDS. Present ideas on bladder compliance, detrusor overactivity, and voiding function are being questioned. AUDS studies performed on asymptomatic, neurologically intact volunteers have shown a 30% incidence of detrusor overactivity. It has been previously suspected that bladder compliance is related to the speed of bladder-filling, and AUDS has confirmed this fact (Kulseng-Hanssen and Klevmark, 1996). Finally, voiding pressures during AUDS in women have been shown to be significantly higher than those obtained during conventional urodynamics.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree