18 Urethral Injection of Bulking Agents for Intrinsic Sphincter Deficiency
INDICATIONS AND CONTRAINDICATIONS
Contraindications to the use of periurethral bulking include active urinary tract infection, high residual urine (>100 mL), severe detrusor overactivity, and reduced bladder capacity (<250 mL). Periurethral bulking can be done after radiation therapy, but results have not been encouraging.
MATERIALS (see Box 18-1)
BOX 18-1 INJECTABLE AGENTS IN NORTH AMERICA
| Trade Name | Company | Approval |
|---|---|---|
| Contigen | CR Bard Inc., Covington, GA | 1993 |
| Durasphere EXP | Carbon Medical Technologies Inc., St. Paul, MN | 1999 |
| Tegress | CR Bard Inc., Covington, GA | 2005 |
| Macroplastique | Uroplasty BV, Geleen, The Netherlands | FDA trials ongoing |
| Zuidex | Q-Med AB, Uppsala, Sweden | FDA trials ongoing |
| Coaptite | Bioform Medical Inc., San Mateo, CA | 2006 |
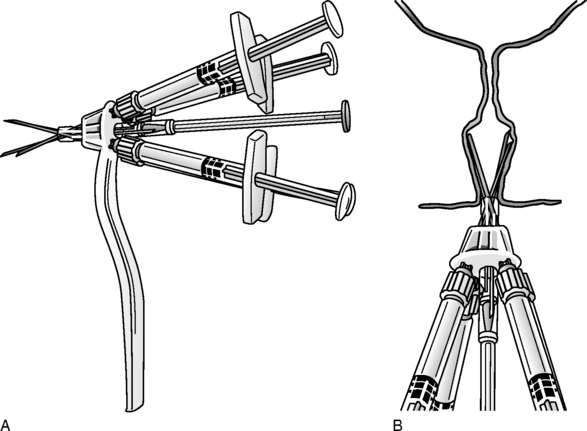
Zuidex gel (Q-Med AB, Uppsala, Sweden) is a combination of dextranomer (cross-linked polysaccharides) and hyaluronic acid. Dextranomer has been used in wound treatment for several years. Nonanimal stabilized hyaluronic acid is similar to natural hyaluronic acid found in the body. The material is prepared in 0.7-mL syringes and used transurethrally with an implantation device (Implacer) and the injection of four syringes of material (see Fig 18-3). The material is in current use in the United States for ureterovesical reflux and is marketed as Deflux.