CHAPTER 8 Upper Blepharoplasty: Volume Enhancement via Skin Approach: Lowering the Upper Lid Crease
Over the years, success of a particular surgical procedure, even aesthetic, has been measured mostly by perceived outcome and to some degree by the frequency of complications. Since the overwhelming majority of aesthetic periorbital ‘complications’ have occurred with lower blepharoplasty, most of the attention on newer and improved techniques has focused on the lower periorbita1–6 (see Chapters 14–19, Lower blepharoplasty).
As functional misadventures are a much less encountered occurrence after upper blepharoplasty, complacency with existing methods and perpetuation of ill-perceived solutions to rejuvenation of the upper periorbita prevail.7,8
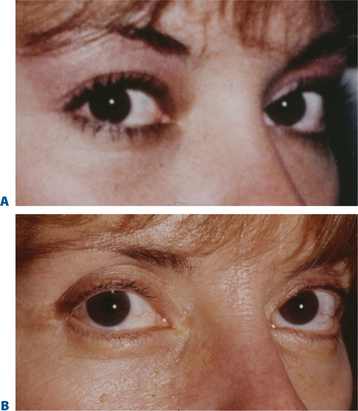
With rare exception, the approach to upper blepharoplasty has not been particularly physiologic or individualized and the universal application of traditional remedies for upper periorbital rejuvenation has translated to mediocrity.7–9 The prevailing perception has been that the appearance of the aged upper eyelid is primarily due to excessive skin, muscle, and fat often in conjunction with brow descent. Additionally, there is the confounding erroneous memory in many individuals of what their upper periorbita looked like in youth. Finally, there is the influence of the ‘famous and beautiful’ people on what patients may request for their eventual appearance despite their configuration in earlier years (Fig. 8-1) that may explain some of the historical aesthetic desires as well as changes in ideas and what is currently expected after surgery.
The consultation
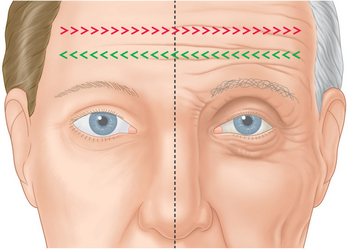
As with all surgical approaches to rejuvenation, we must take into account what are the actual changes that occur in the upper periorbita and whether the existing methods consider these occurrences for a wide variety of individual presentations (Fig. 8-2). Do these techniques result in a rejuvenative appearance or simply achieve a ‘cause and effect’ outcome whereby an altered appearance replaces youth? (Fig. 8-3). And, ultimately, what surgical procedures are some patients willing to undergo and what do they expect from surgery?
Often when a patient consults with one or a number of surgeons in consideration of rejuvenation of the upper periorbita, the possibility of brow lift is discussed. Some surgeons may suggest that a patient requires a brow lift while others may not. What is the basis of this inconsistency and what has been the justification and anatomic rationalization of either approach? Moreover, if the patient who presents for upper periorbital rejuvenation has a mild to moderate degree of perceived brow ptosis and refuses to undergo a brow lift of any sort, are there other methods that can significantly improve the appearance without the incorporation of browplasty/pexy?
We are all aware that at times particular procedures are offered for lack of knowledge or ability to achieve a desired effect in another, perhaps more accurate, manner. For instance, when consulting with a young female who presents for improvement of the appearance of the upper periorbita, what are the findings on examination that suggest a particular approach? How much has the eyebrow actually descended and why would one then offer a brow lift if there has been little change over the patient’s lifetime? (Fig. 8-4). What has been the justification and anatomic rationalization of any given approach?9 What effects have been ignored with this approach that could be improved upon? Is there ever an indication for a 35 to 40-year-old (or younger) to have a brow lift? (Fig. 8-5). Have we considered what this individual patient’s brow position was in youth? Why, in fact, are many patients resistant to brow lifts? What should we strive for to accomplish the most acceptable and aesthetic rejuvenative result? A review of some simple but common observations of the changes in the aging upper periorbita for a majority of our patients sheds more light on which surgical solutions are both physiologically and aesthetically feasible (Figs 8-2, 8-6):
Eyebrow position and volume
The term brow ptosis suggests a descent of the eyebrow position from its ‘normal’ state. Obviously some younger individuals with ‘low’ brows may request a ‘change’ or improvement of their brow position much as one would desire otoplasty or rhinoplasty (Fig. 8-5). Additionally, many patients will present wishing for surgical correction to accomplish more pretarsal ‘show’ for reasons that include creating more area to apply cosmetics, a mistaken memory of what their upper eyelid looked like in youth, or simply their desired outcome. A review of old photographs is most often revealing, yet the ultimate determination must rest on the choice of each individual patient. Careful analysis including the use of morphing techniques as shown by Lambros11 and others,12 repeatedly and consistently has shown that the deflationary effects from facial volume loss with age can yield the apparent and illusionary effects of facial soft tissue ptosis. These misperceptions include an illusion of brow ptosis in some individuals that is due to soft tissue volume depletion, particularly in the temporal and lateral infrabrow regions, which may have prompted a brow lift when replacement of soft tissue volume has been shown to enhance aesthetics (Fig. 8-7)13 (see Chapter 23). There are also some individuals who would have compromised aesthetic results by not undergoing the necessary brow lift. Which individuals then, benefit from which procedures?
The upper eyelid crease and fold
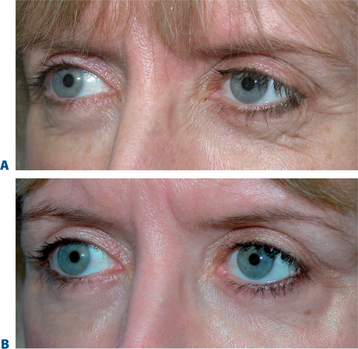
What has been less understood, are the actual changes that occur to the upper eyelid crease and fold. Often the position of the eyelid crease is obscured by the appearance of redundant upper eyelid skin and fold displacement. A careful analysis of the crease in most individuals shows varied change from youth. The changes may also be asymmetric in any one individual (Fig. 8-8). This includes an elevated crease that may manifest in one or both upper eyelids. The solution has been, in most cases, to raise the eyelid crease of the affected upper eyelid with the excision of ‘excess’ soft tissue with or without brow lift. This maneuver, however, is routinely and repeatedly performed without respect for the presenescent appearance or understanding of the actual age-related changes of the upper periorbita (Figs 8-2, 8-3, 8-6).
The routine applications of traditional concepts in incision placement and soft tissue excision have also plagued some other technical aspects in upper blepharoplasty. The usual design of the upper eyelid crease commonly involves the use of 10 mm or greater (height) eyelid crease incision with excision of skin, orbicularis oculi muscle, and preaponeurotic fat.7,8 This is customary whether or not upper blepharoplasty is performed with or without a brow lift. In part, the basis of this approach has been an attempt to elevate the upper eyelid crease, in essence, to expose a greater amount of the pretarsal surface and to ‘debulk’ the upper eyelid fullness by en-bloc or separate resection of skin and muscle.8 This approach, however, facilitated additional steps in upper blepharoplasty that are also aesthetically detrimental, including better access to the preaponeurotic fat (resulting in further soft tissue reduction and volume depletion) and the levator aponeurosis for supratarsal fixation. Concerns with a lower placed incision included possible visibility of the upper eyelid incision scar, inability to achieve adequate final pretarsal exposure, and risk to the levator aponeurosis insertion to the pretarsal surface, especially when utilizing a full thickness skin muscle excision whether removed in separate ‘layers’ or ‘en-bloc.’ The long-term consequences of the traditional approach, however, can be suboptimal. Deep or ‘hollow’ upper eyelid sulci are common effects, presumably from over-resection of soft tissue (Fig. 8-3), especially fat. In some, the upper eyelid crease scar becomes hypopigmented (Fig. 8-9) and usually more visible with time, usually at a much higher level (15–20 mm). This is especially true in the patient with a prominent globe, negative upper periorbital vector, or in those who habitually elevate their eyebrows for a variety of reasons. The color transition can also at times become quite obvious, as the upper edge of the incision is placed in the darker and thicker sub-brow skin. The pretarsal skin also becomes progressively less taut (more ‘crepey’ in appearance) due to the sliding effect as most original points of fixation have been compromised by over-dissection.
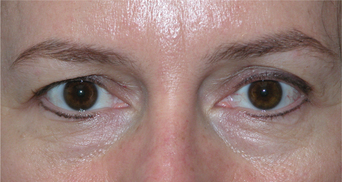
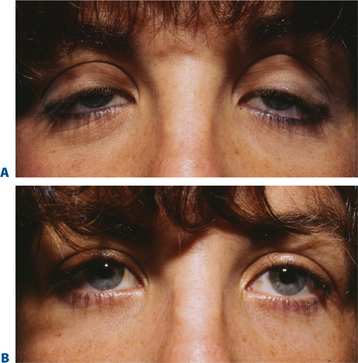
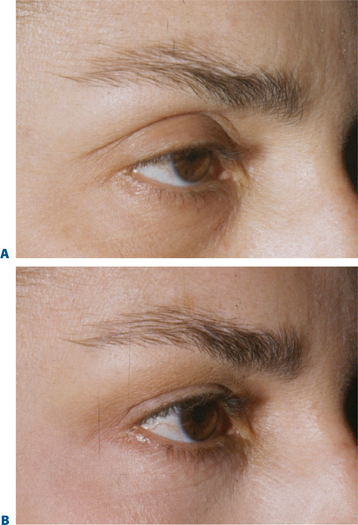
Comparative anatomy and aesthetics of upper eyelid ptosis and periorbital aging
Some of the changes that can occur in the aging upper periorbita parallel the findings seen with true upper eyelid ptosis at any age. Alternative and improved surgical repair has shed light on the effects that can be created by alterations in the upper eyelid crease. Often in those with significant blepharoptosis, there is an apparent, unusually elevated (from youth), upper eyelid crease, at times >15–20 mm (Fig. 8-10A). This is also typically associated with a deep, hollow, upper eyelid sulcus and apparent volume depletion from either fat atrophy or retraction of the central preaponeurotic fat pad. This is further accentuated by the patient’s subconscious efforts to raise the eyebrow in an attempt to elevate the upper eyelid to enhance visual function (Figs 8-10A, 8-11A). Although the mechanism for these latter changes has been challenged (in both non-surgical and post-surgical14 states) I believe that it is, in part, a result of atrophic orbital effects causing loss of adherence of the multiple eyelid layers with subsequent loss of the lower positioned upper eyelid crease of youth. With this, the relationship of the levator aponeurosis and orbital septum loses the tight compartmentalization of the central preaponeurotic fat that is normally sandwiched between the levator aponerosis and orbital septum that now can retract into the orbit. Traditional methods of blepharoptosis repair using levator advancement or resection techniques have had much less predictable influences on the eyelid crease. These techniques led to variable excision of the skin and orbicularis oculi muscle, septum, and preaponeurotic fat in order to address the presumed levator aponeurosis dehiscence for repair. I believe this yields less aesthetic results and contributes to the appearance of upper periorbital aging. Minimally invasive surgical solutions to blepharoptosis repair15 (posterior approach/soft tissue sparing such as the Müller’s muscle conjunctival resection) even combined with skin excisional blepharoplasty may improve the upper eyelid soft tissue plane relationships by recreating supratarsal volume that re-establishes the youthful upper eyelid appearance (Figs 8-10, 8-11, see Chapter 11). The analogy of the aging upper periorbita with upper blepharoptosis and a greater sense of the physiologic and anatomic changes that occur in upper facial aging suggest a more sound and logical approach for rejuvenation.