16
Ulnar Tunnel Syndrome
Robert M. Szabo
History and Clinical Presentation
A 59-year-old right hand dominant physician fell off a curb on the outstretched hand 14 months prior to this evaluation. At that time, he was treated for a fracture at the base of his right fifth metacarpal and a fracture of his left radial neck. He noticed paresthesias along the ulnar side of his right fifth finger and right-sided hand weakness. The patient is a non–insulin-dependent diabetic who suffered a subarachnoid hemorrhage complicated by uncontrolled seizures, for which he had a hippocampectomy and still takes carbamazepine (Tegretol).
PEARLS
- Routine release of the ulnar tunnel in patients with carpal tunnel syndrome and mild ulnar symptoms is not indicated; carpal tunnel release alone increases the volume of the ulnar tunnel and changes its shape from triangular to ovoid.
- Anatomy in this area is quite variable, so always start dissection proximal to the wrist crease and proceed distally and anticipate anomalies.
- Clawing of the small and ring fingers is seen much earlier with compression of the ulnar nerve at the wrist than at the elbow because of the intact flexor digitorum profundus innervation.
PITFALLS
- Patients with coexisting polyneuropathy may benefit from ulnar tunnel release but should be warned that not all of their symptoms may resolve.
- Do not cross the wrist crease with a perpendicular incision or a hypertrophic scar may form.
Physical Examination
Point tenderness was noted over the hook of the hamate. There were no other areas of tenderness, signs of previous trauma, or any swelling, masses, or bruits. Sensibility testing with Semmes-Weinstein monofilaments revealed 3.61 in the little finger and ulnar half of the ring finger and 2.44 in the remainder of the hand. Two-point discrimination was 7 mm in the little finger and ulnar half of the ring finger and 6 mm in the remaining fingers. Light-touch perception was normal on the dorsal-ulnar aspect of the hand and wrist. Nerve percussion and Phalen’s tests were negative. Manual motor testing was 5/5 throughout except for 0/5 of the third palmar interosseous muscle and the first dorsal interosseous muscle, which was 2/5 with moderate atrophy present. Mild clawing of the ring and small fingers was present, as was a positive Froment-Jeanne sign. Wrist range of motion was symmetric except for flexion, which was 45 degrees on the right compared with 80 degrees on the left. Key pinch on the right was 0 lb compared with 7 lb on the left. Tip pinch was 2 lb on the right and 7 lb on the left. Grip strength at the second setting was 60 lb on the right and 65 lb on the left. The Adson’s, hyperabduction, military brace positioning, and 3-minute elevation, as well as the Allen’ test, were normal.
Diagnostic Studies
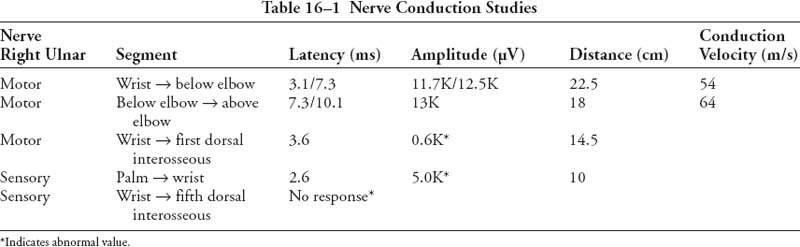
Anteroposterior, lateral, and oblique radiographs and a carpal tunnel view of the right hand revealed no acute fractures, subluxations, or dislocations. A chest radiograph was normal. Computed tomography of the wrist revealed small bone fragments adjacent to the base of the fifth metacarpal predominantly along its palmar-radial aspect. The hook of the hamate appeared intact. In the presence of a normal Allen’s test, Doppler studies were not performed. Nerve conduction study results are shown in Table 16–1.
Electromyographic Study Results
There was no evidence of abnormal spontaneous activity in the right flexor digitorum profundus, abductor digiti minimi, or the abductor pollicis brevis. In the right first dorsal interosseous muscle there was increased insertional activity with 2+ (present at multiple sites) fibrillations and 2+ positive sharp waves; recruitment frequency was 30 to 40 Hz (normal: 5 to 15 Hz); the interference pattern was decreased and discrete, indicating marked loss of motor units; amplitude was decreased with the first recruitment = 1000 μV and the duration of the voluntary motor unit potentials was increased.
Differential Diagnosis
Brachial plexus injury
Upper plexus
Lower plexus
Cervical root compression
Ulna nerve tunnel compression
Elbow
Wrist
Corvical disk disease
The ulnar nerve, containing fibers from the ventral rami of C8 and T1, is the terminal branch of the medial cord of the brachial plexus. Pathologic compression of the ulnar nerve occurs most commonly either at the elbow (cubital tunnel syndrome) or at the wrist where the ulnar nerve passes through the confines of the canal of Guyon (ulnar tunnel syndrome). With either of these conditions the patient may present with numbness along the little finger and ulnar half of the ring finger, often accompanied by weakness of grip, particularly in activities in which torque is applied to a tool, and rarely by wasting of the intrinsic musculature in the hand. The site of the compression may be determined by a careful physical examination; pain at the medial aspect of the elbow, a positive percussion test at the cubital tunnel, or exacerbation of symptoms by full flexion of the elbow suggests cubital tunnel syndrome. Sensory involvement on the ulnar dorsal aspect of the hand also suggests cubital tunnel syndrome, as the dorsal cutaneous branch of the ulnar nerve originates proximal to the canal of Guyon. Weakness of the deep flexors to the ring and little fingers as well as weakness of the flexor carpi ulnaris signal proximal ulnar nerve entrapment. Grip and pinch strength measurements may demonstrate weakness in more advanced lesions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree