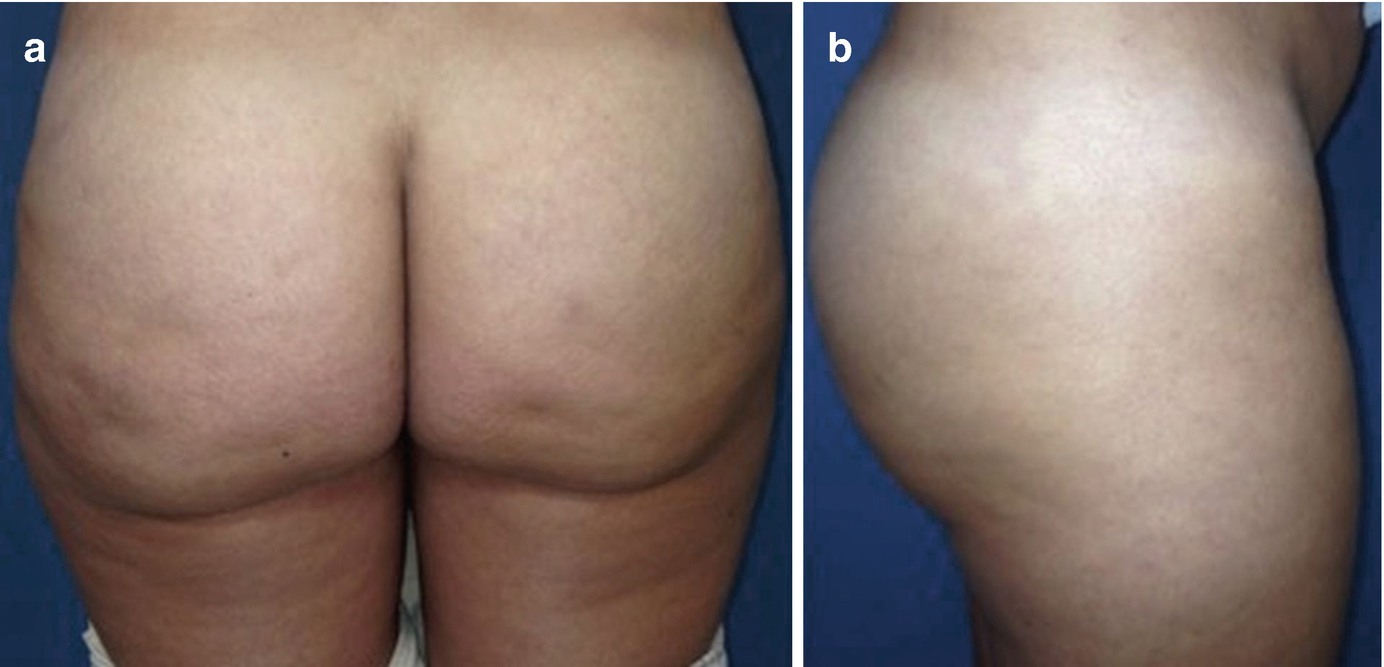
(a) PA and (b) lateral views of Stage I silicone toxicosis. There are no significant findings on physical exam, but the patient may endorse occasional symptoms, including pain, and diffuse inflammation. Medical management with NSAIDs is the treatment modality of choice in these cases
Stage IIa
(a) PA and (b) lateral views of Stage IIa silicone toxicosis. Several palpable nodules are present throughout the gluteal region; however no chronic skin changes are identified. Patients report frequent pain, in conjunction occasional cellulitis or abscess formation. Treatment may consist of a combination of antibiotics, anti-inflammatory agents, and immunomodulators. These patients are ideal candidates for UAL
Stage IIb
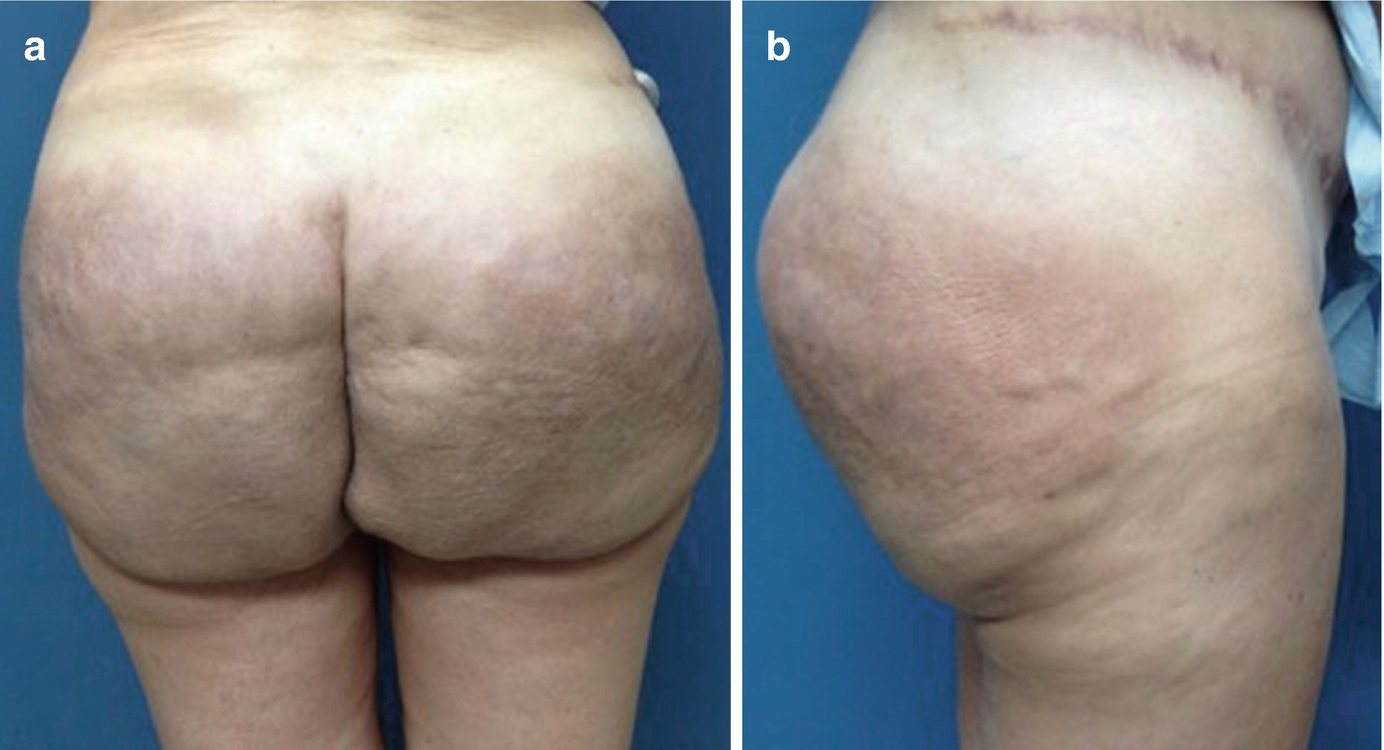
(a) PA and (b) lateral views of Stage IIb silicone toxicosis. There is evidence of diffuse erythema, palpable masses, and associated gluteal contour abnormalities. Patients report increasing pain, abscess formation, and worsening skin changes with occasional drainage of serous fluid or oil-like material. These patients are candidates for treatment with UAL in a deeper plane due to the degree of skin compromise [16]
Stage III
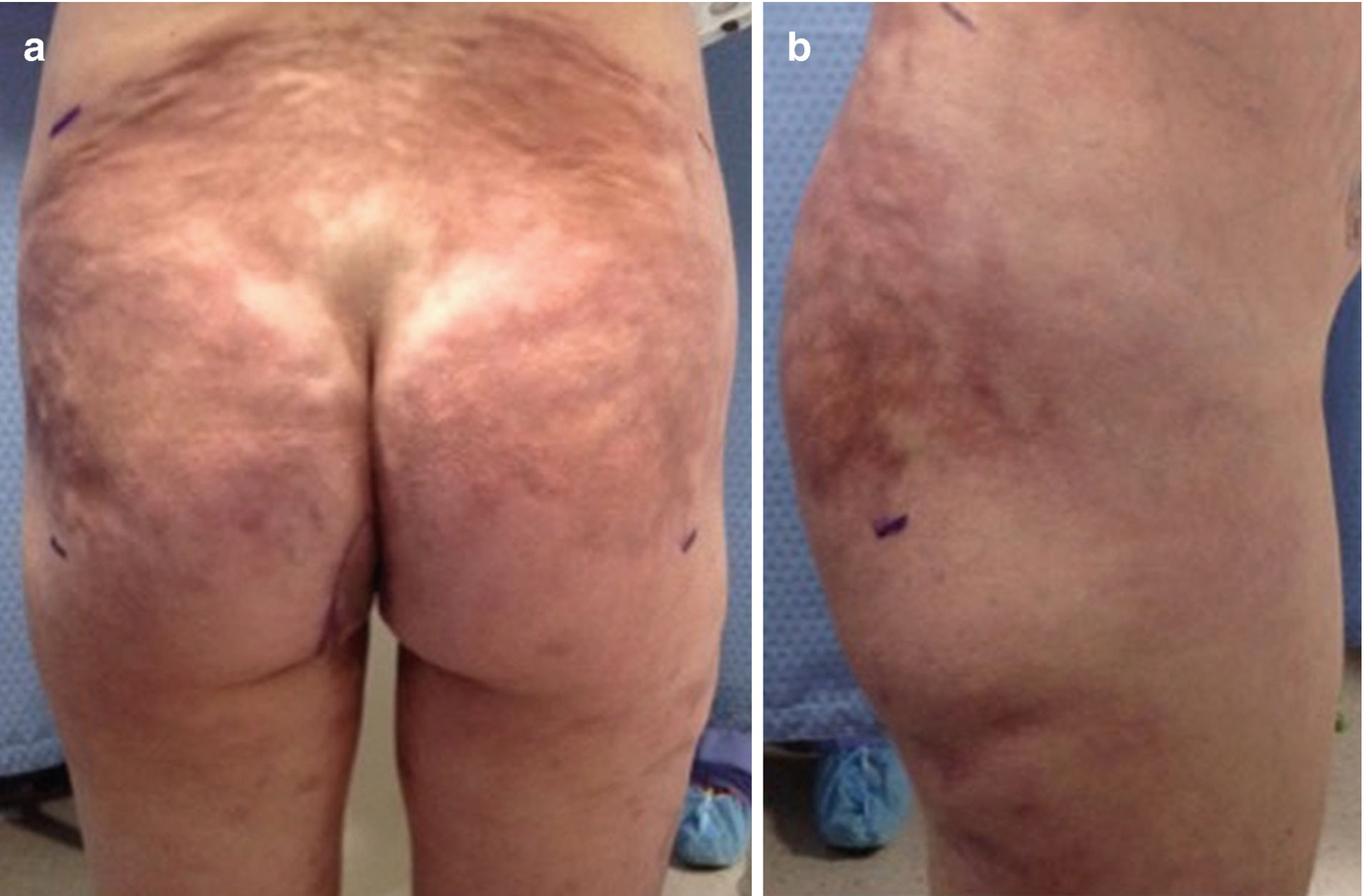
(a) PA and (b) lateral views of Stage III silicone toxicosis. Dramatic scarring is present, with leather-like changes to skin, deep contour abnormalities, and chronic non-healing wounds which occasionally drain silicone oil. Palpable tender masses will likely still be present despite prior surgeries. Repeated surgical resection is the only treatment option for these patients
Treatment Options
Medical management should always be attempted in patients with Stage I and IIa silicone toxicosis. NSAIDs are a good starting point for oral treatment regimens but are rarely successful in completely resolving symptoms in even the mildest of cases. Thus, combination treatments are usually employed for a multimodal approach to symptom relief. Intra-lesional steroid injections, systemic steroids, immune-modulators, and antibiotics work well in combination and are useful for temporary improvement in symptoms [1]. Systemic corticosteroids are an excellent option for tempering inflammation, but results are transient and symptoms tend to return once the patient has begun to taper the dose [7, 19]. Minocycline has been most commonly cited as a useful agent for the treatment of silicosis, as it possesses both anti-inflammatory and immunomodulating properties [1]. It is a safe and efficient way to combat the chronic inflammation of siliconomas [1]. Minocycline is typically dosed at 100 mg twice daily, with or without the addition of a tetracycline, and had been reported to provide good results in several clinical reports [12]. The addition of the tetracycline is thought to aid the patient by combating any biofilm on the silicone spheres and augmenting the anti-inflammatory activity of minocycline on the granulomatous immune reaction [12]. If there is concern for a deep infection or progressive cellulitis, patient may need parenteral antibiotics for infection control prior to surgical intervention [3].
It is important to note that, once injected, silicone permanently resides in the tissues and surgery may be the only way to definitively treat chronic symptoms. However, traditional options for surgical resection, including en bloc excision, dermolipectomy, or suction-assisted lipectomy (SAL), can be technically difficult and have disfiguring results [10, 16]. While surgery is unquestionably indicated for patients with Stage III changes who may have deep tissue abscesses, fistulas, and fasciitis, alternatives should be considered in most other cases [3]. Standard liposuction has been suggested as an alternative to surgical excision, but it is difficult to pass a standard liposuction cannula through the inflamed tissues in a controlled fashion, and there is risk of injury to adjacent, non-affected areas with this technique [13, 16, 19]. UAL, however, performs better when faced with dense fibrotic tissues and, thus, is a good option for select cases of silicone toxicosis [16].
Specifically, patients with Stage IIa and IIb silicone toxicosis are the best candidates for UAL. UAL is a safe and effective method of removing silicone infested tissue while avoiding extensive surgical mutilation and results in minimal bleeding and less pain than traditional surgical excision or SAL [7]. Additionally, UAL of the gluteal region can be combined with SAL of the abdomen and flanks to allow for immediate intramuscular fat grafting for buttock augmentation, if desired by the patient [7]. Lipofilling can be particularly useful for patients with expected large volumes of toxin removal to prevent deflated or irregular contours following UAL [16].
Patient Selection
Candidates for UAL often have severe symptoms related to their silicone toxicosis but opt to delay their medical care in an effort to prevent the embarrassment and fear associated with admitting to receiving illicit injections [6]. It is important for physicians to thoroughly question patients with atypical symptoms when there is a concern for toxicosis, as silicone can mimic other inflammatory conditions or even malignancy and an incorrect diagnosis could result in a thoroughly mismanaged patient [6]. Patients will usually have a history of gluteal augmentation injections from a friend or acquaintance [16]. The substance is typically unknown to the patient, though they might believe it to be silicone [16]. Since patients who receive silicone injections usually place a great deal of importance on their appearance, even moderate degrees of silicone-related skin changes can cause psychological embarrassment with withdrawal behaviors [2, 6]. Furthermore, there is usually a concern that surgical excision is the only treatment option, and the fear of permanent scarring and further deformity may cause patients to refuse treatment [6]. In these cases, UAL is just one of several alternate treatment options that should be considered [6]. However, before deciding to proceed with UAL, it is important for the physician to rule out severe and atypical infections or open wounds in the gluteal region which should be treated prior to any liposuction procedures [7, 19].
Preoperative Evaluation and Imaging
Patient Expectations
During the preoperative consultation, it is important for the physician to set realistic expectations for the patient [16]. Informed consent must be obtained and there should be discussions regarding cost, likely outcomes, limitations of correction, and other issues that may arise when treating a complicated problem like silicone toxicosis [12]. Patients need to be aware that it can be hard to predict results of UAL because there is usually limited information regarding the technique used during the original injections, as well as the amount and composition of the material injected [4, 19]. Photographic documentation is imperative so that any preexisting contour irregularities are noted in the medical record [12]. Most importantly, patients need to understand that it is difficult or impossible to remove all of the foreign material and affected tissue [13, 16, 20]. There is no cure [16]. The realistic goal should be to decrease the patient’s pain while optimizing their function and form [16].
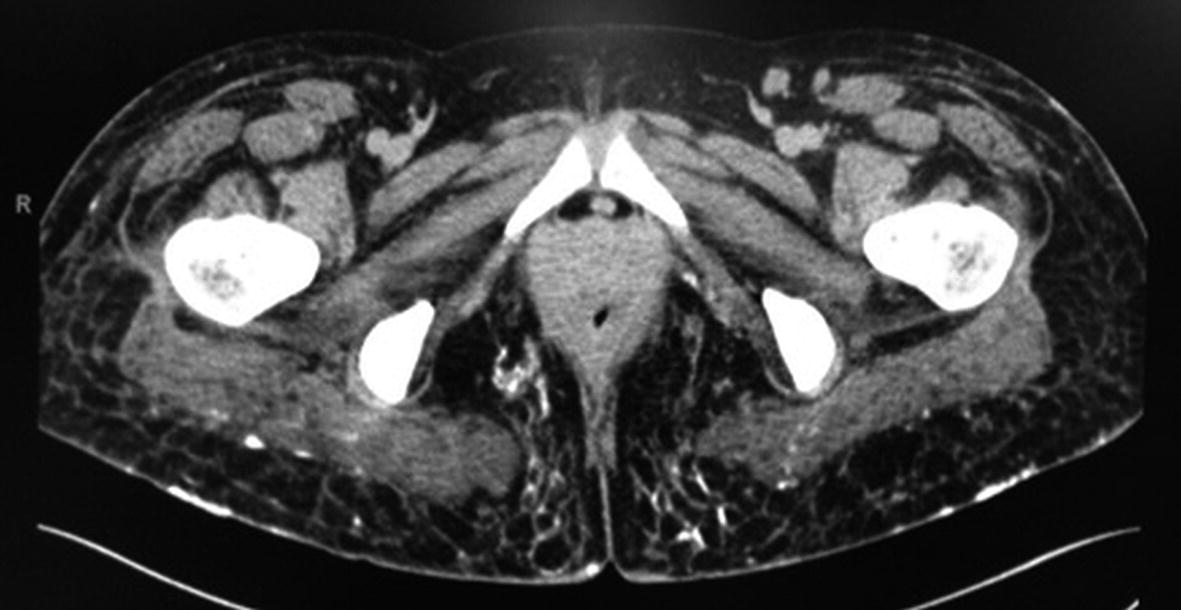
Imaging

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








