Transverse cross section of female buttocks. The DEEP gluteal fascia (green) lies on top of the surface of the gluteus maximus muscle. The SUPERFICIAL gluteal fascia (yellow) is a distinct fascial layer analogous to Scarpa’s fascia in the anterior abdomen and lies above the deep gluteal fascia and below the dermis, dividing the subcutaneous region into two spaces
The superior surface of the gluteus maximus muscle is covered with a fascial plane (the deep gluteal fascia) that the Multi-Society Task Force has recommended surgeons do not penetrate [9, 13]. However, there also exists a second fascial layer (the superficial gluteal fascia) within the subcutaneous zone above the deep gluteal fascia and below the dermis. The superficial gluteal fascia is thick, is impregnated with fat, and can only be appreciated in an open dissection or with ultrasound visualization.
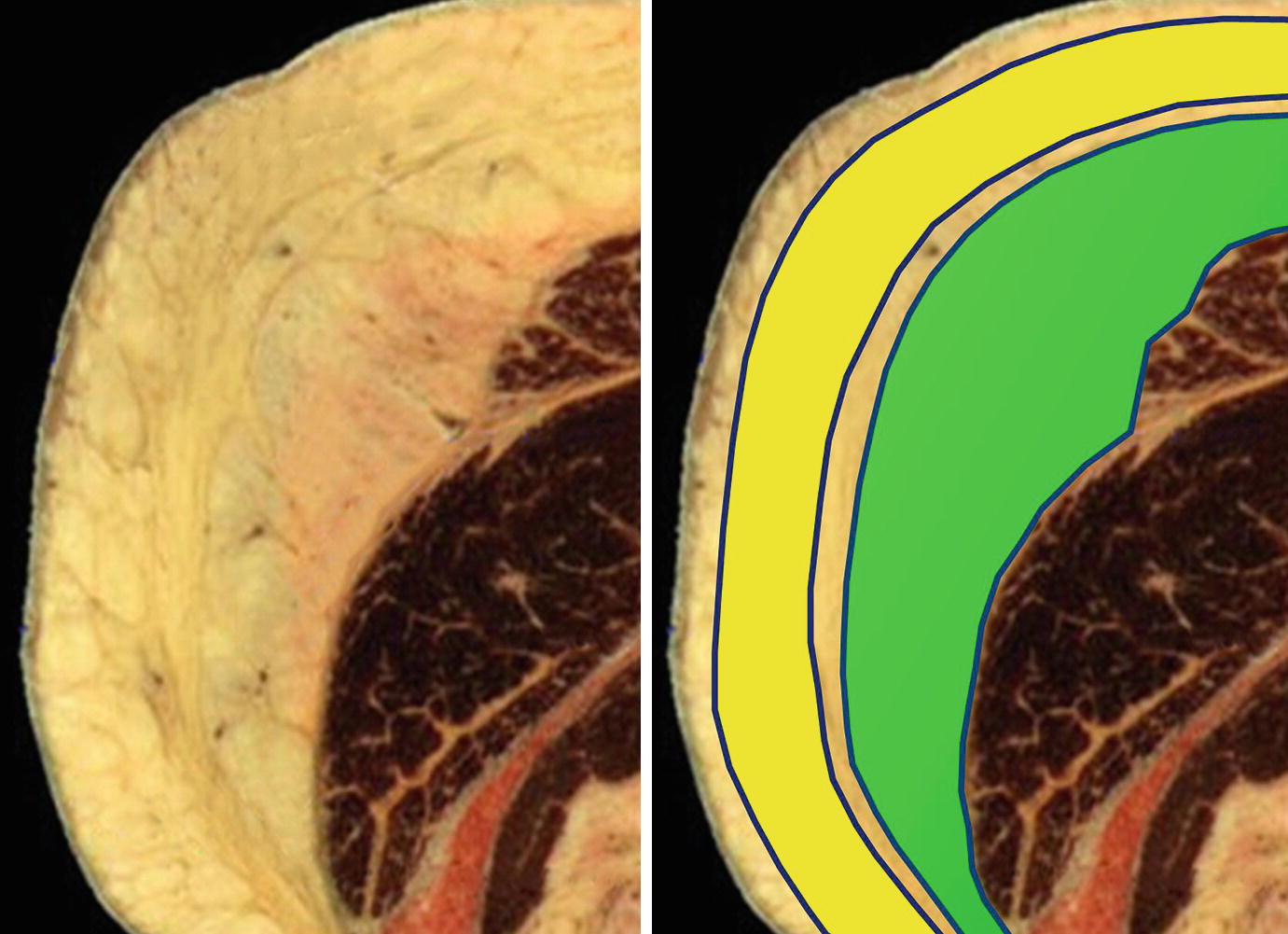
Transverse cross section of female buttocks. The superficial gluteal fascia divides the subcutaneous region into two spaces. The SUPERFICIAL subcutaneous space (yellow) is below the skin and above the superficial gluteal fascia. The DEEP subcutaneous space (green) is below the superficial gluteal fascia and above the deep gluteal fascia. Ultrasound allows the surgeon to accurately enter each space and manipulate it while always remaining above the deep gluteal fascia
More important clinically, if the superficial gluteal fascia remains intact, it can retain the fat graft that is specifically injected above or below it, like the casing of a sausage. Fat graft injected into the deep subcutaneous space (above the deep gluteal fascia and below the superficial gluteal fascia) can create excellent volume and central dome projection, similar to a subfascial implant. Fat graft precisely injected into the superficial subcutaneous space (above the superficial gluteal fascia and below the skin) can correct superficial contour deformities and depressions. The consistent accurate injection of fat graft into either the superficial or deep subcutaneous spaces can only be performed with real-time intraoperative ultrasound visualization.
It is also important to remember that the entire subcutaneous zone (including both the superficial and deep gluteal spaces) ranges in thickness from 1 cm (outer hips) to 3–4 cm (central gluteal dome). This thickness may also vary significantly between patients. This means that gluteal surgeons must graft in a thin space under a curving dome of varying thickness. This small variable target may account for the inadvertent deep intramuscular injections by well-intentioned surgeons grafting without ultrasound visualization.
A surgeon can use real-time intraoperative ultrasound to not only avoid an intramuscular fat graft injection but to accurately target fat graft into the superficial or deep subcutaneous spaces. Neither of these techniques are possible without ultrasound. Real-time intraoperative ultrasound during a Brazilian butt lift (ultraBBL) can not only make fat grafting safer but much more powerful and accurate as well.
Preoperative Assessment
Like all plastic surgery, careful preoperative assessment and planning before gluteal contouring and fat grafting is essential. The surgeon should sit with the patient to understand their goals, priorities, and areas of importance. Asymmetries must be identified before surgery and a discussion should be held about the preoperative shape of the patient’s waist, hips, buttocks, thighs, and back. The surgeon should ask what kind of shape the patient would like and understand how the patient would like to specifically change their waist, hips, point of maximum lateral hip projection, buttocks, thighs, and back. Within each anatomic zone, the bony framework, the muscles, fatty layer, and skin should be assessed to determine how each of these components affects the contour. Ultrasound can be used to determine the thickness of the subcutaneous envelope in each region and plan the quantity and location of the fat graft in each subcutaneous space as well as any areas of adhesion that should be released.
Digital imaging which can simulate the patient’s possible postoperative shape is helpful to show the patient the effects of liposuction, fat shifting, and fat grafting. It is even more useful in managing expectations and showing the patient what is not possible. If the patient has requested a very large volume result, digital imaging can illustrate what is reasonable and safe and open a discussion on staging the procedure. Patients interested in large-volume results that would be best served with staged procedures can be shown where fat can be left undisturbed and ready for harvest in a second round of fat harvest and grafting.
Once the final operative plan has been decided, the surgeon should discuss the recovery, expected fat resorption rates, and limitations on postoperative activity.
Surgical Equipment and Setup
Intraoperative Ultrasound Systems
Over the past 7 years, the author has used five different ultrasound systems with gluteal fat grafting. Real-time intraoperative ultrasound can actually be used with any cannula or liposuction/fat grafting system. However, when a syringe fat grafting system is used, both of the surgeon’s hands are occupied. One hand must hold the syringe while the other hand pushes the plunger to inject the fat. In this scenario, the surgical assistant or scrub tech must control the sterile ultrasound probe, making coordination with the injecting surgeon difficult. To allow the surgeon to control the fat grafting system and the ultrasound probe simultaneously, a power-assisted liposuction system (PAL, MicroAire Charlottesville, VA) is used in conjunction with a peristaltic pump for controlled propulsion of the fat graft. In this manner, the surgeon can inject fat via expansion vibration lipofilling [18] with one hand and control the ultrasound probe with the other hand.

The Clarius ultrasound probe is a 4–13Mhz high-frequency linear L7 portable, waterproof, wireless ultrasound probe (maximum depth of 7 cm) that can be placed entirely in a sterile probe cover and can stream a high-resolution ultrasound video to Apple iOS or Android tablets

The Butterfly iQ ultrasound probe is a new generation probe that uses microchips rather than piezoelectric crystals to generate and interpret ultrasound waves. This is a wired system that is currently compatible with iOS devices
Fat Trap Canister
It is preferable that the fat graft remain in a liquid state for smooth propulsion through our peristaltic pump system. A fat trap within the liposuction tubing circuit is used to collect the fat that has been aspirated. This trap or canister is connected by liposuction tubing between the harvest cannula and the liposuction machine/suction source. Many canister models are available and have been tried, but the simplest one is preferred – a reusable plastic canister with a lid and no openings or spigots at the bottom [19]. For a fat grafting procedure using a peristatic pump and the MicroAire system, two different types of liposuction tubing are necessary. Standard liposuction tubing (both ends with large openings) (PSI-TEC Tubing, Ref PT-5558, Mentor, Irving, TX) is used to connect the suction source to the canister lid. MicroAire tapered tubing (Ref PAL-1200, MicroAire, Charlottesville, VA) is then used to connect the other port on the canister lid to the MicroAire liposuction cannula. When harvesting fat, a vacuum is established through the tubing and any aspirated fat is captured within the canister. The lipoaspirate that is collected is allowed to separate with gravity and time to allow the fat to separate from the tumescent fluid. Openings or spigots at the bottom of the fat trap canisters act as chokepoints in the fat grafting system during EVL and are not recommended.
Peristaltic Pump for Fat Grafting

Sterile silicone insert kit connects the standard liposuction tubing (two large openings) with the MicroAire tubing (one large opening, one tapered opening) and the silicone insert is then placed into the peristaltic pump. The surgeon can control the flow of the fat graft with a foot pedal connected to the peristaltic pump
Surgical Technique
Liposuction of the torso and fat grafting to the gluteal areas and hips is designed to be an outpatient procedure performed under general anesthesia. Specific types of anesthesia do not effectively protect the patient from fatal complications such as fat pulmonary emboli. What does protect the patient is ensuring that there is no intramuscular fat injection. Ultrasound visualization can continuously confirm the real-time position of the cannula tip and keep the patient safe. The ultraBBL is performed under general anesthesia to facilitate comfortable controlled extraction of deep and superficial fat and for maintenance of the airway when the patient is in the prone position.
Circumferential Sterile Prep of the Patient Post-Induction
The surgical prep and draping is important as it provides a sterile field with circumferential access to the torso and permits safe position changes without the use of a bean bag, redraping, the use of an extra stretcher, or extra staff. The position changes can be performed without breaking sterility in under 30 seconds. This prep and draping technique is now used in all of our body contouring procedures allowing circumferential treatment of every torso.
The patient never receives a standing prep because sterility is usually broken by the time the patient has climbed onto the operating table. More importantly, a standing prep is extremely uncomfortable for the patient and the operating room staff. The minutes before induction are important for the patient’s perception of the procedure and are usually the only thing they remember about the surgery. All of our cases begin with the patient supine as anesthesia is being induced followed by intubation. Sequential compression devices are placed on both legs. A Foley catheter is placed and taped securely to the left inner thigh and left inner calf of the patient. The Foley passes off the OR table between the patient’s feet. This is important as securing the Foley in this manner will prevent nerve compression injuries or urethral traction injuries during the multiple position changes.
The surgical team (four people including the sterile surgical tech, the non-sterile circulating nurse, the anesthesia provider, and the non-sterile surgeon) circumferentially preps the patient. The surgical tech begins by rolling a sterile table cover with an impermeable surface (44″ × 90″, Ref 8377 Cardinal Health, Waukegan, IL) to the midpoint and holds the rolled edge superiorly.
The surgeon is standing on the left side of the patient and places the patient in the left lateral decubitus position facing the surgeon while the anesthesia provider secures the endotracheal tube and supports the head to keep the neck in a midline position. Lateral and prone support for the head and neck is maintained with a square anesthesia head pillow. (Wilson Foam Frame Kit, REF FP-WILSON Cardinal Health Waukegan, IL). The circulating nurse then preps the patient (any prep is acceptable; Betadine will be used in this description) beginning with the anterior abdomen at the umbilicus, over the right waist and flanks, and down to the entirety of the exposed back down to the surface of the operating room table. Once the back has been prepped, the surgical tech places the rolled edge of the sterile table cover on top of the exposed operating room table and pushes the rolled drape as far under the patient as possible. The surgical tech places a halfway rolled blue towel on top of this drape at the level of the pelvis. This blue towel will be used to lift the patient during all position changes. The area that the nurse has just prepped is now sterile and this sterile surface will lie on the sterile under body drape in the next step.
At this time, the patient is returned to the supine position and the entire prepped back and right side is now resting on the sterile under body drape. The surgeon and the circulating nurse now switch sides around the operating room table and the surgeon now places the patient in the right lateral decubitus position, rolling the right side, flanks, waist, back, and thighs that have previously been prepped onto the sterile drape. The left side, flanks, waist, back, and thighs are now exposed and facing up and are ready to be prepped. The circulating nurse now preps the left torso. With the patient in this position, the surgical tech unrolls the underbody drape and blue towel to cover the operating room table and arm board. At this point, both of the patient’s sides, flanks, waist, thighs, and back are sterile and are laying on top of a sterile underbody drape. The patient is finally returned to the supine position where the circulating nurse now preps the anterior abdomen and sides from one edge of the table to the other.
Blue towels are secured with staples to cover the genitalia, both thighs and breasts. A three-quarter drape (56″ × 76″, Ref 29350 Cardinal Health, Waukegan, IL) is placed across the patient’s lower body from the mid thighs to the feet. An extra large drape (77″ × 98″ REF 9444 Cardinal Health, Waukegan, IL) is used to cover the upper body and arm boards. During the position changes, the patient will rotate freely under the drapes so the paper drapes are not secured to the patient or the operating room table. In this way, the patient’s torso can be accessed circumferentially and repositioned without changing the drapes or breaking sterility.
Liposuction and Liposculpture
Surgeons often struggle with identifying the endpoint in liposuction. Some surgeons record the volume removed from one side and match this to the contralateral side. Other surgeons count the minutes of liposuction or VASER liposelection in one treatment area and match it to the contralateral side. We must keep in mind that ultimately, liposuction is sculpture. A sculptor does not weigh the amount of stone removed from one side and continues to chisel the opposite side until the same amount of stone has been removed. Like all sculpture, our liposuction surgical endpoint must be anatomic and symmetric.
The anatomic endpoint of liposuction should be to achieve a consistent thickness of the skin fat flap throughout the torso and to ultimately create the specific anatomic shape the patient requested. This process begins before surgery when the skin and fat thickness in all treatment areas are assessed and asymmetries are highlighted. A strategy should be in place to differentially remove fat until the flap has a consistent thickness.
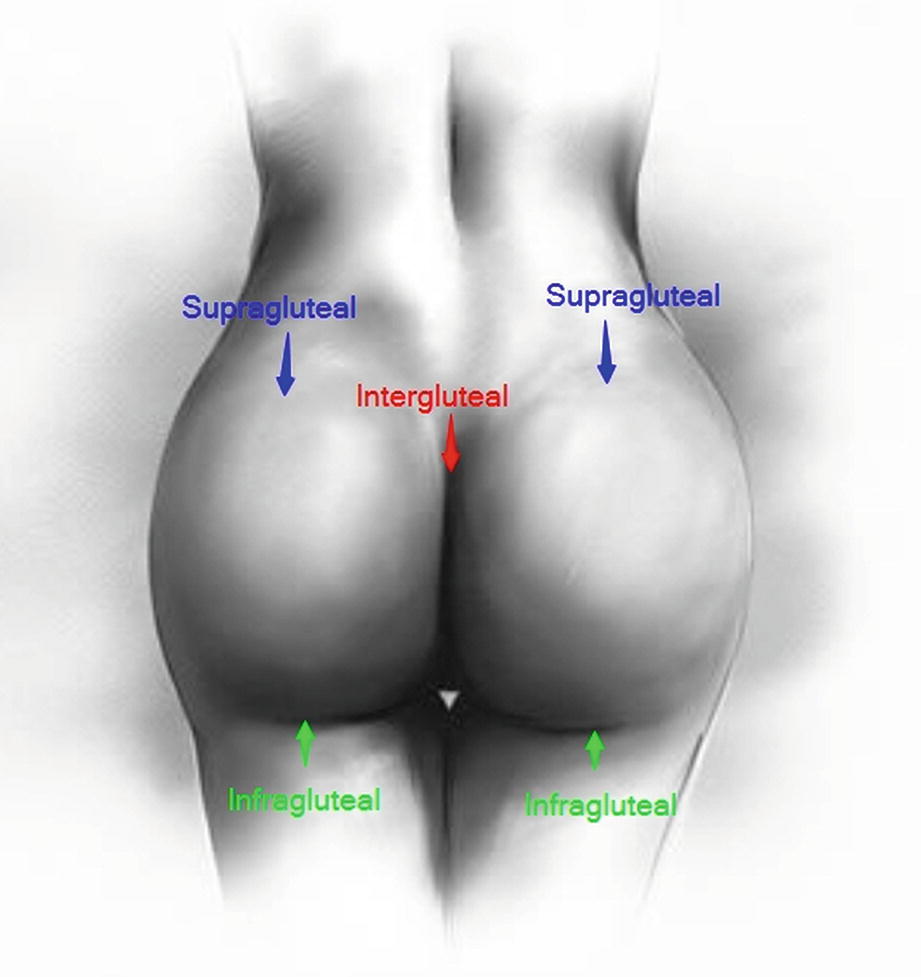
Posterior gluteal access incisions: the supragluteal incisions are used for fat harvest of the back, waist, hips, flanks, and sides as well as fat grafting to the central dome and superior outer hip. The intergluteal incision is used for fat harvest of the back, along the lower latissimus dorsi and for contouring the superior buttock as well as fat grafting to the dome and the supragluteal region. The infragluteal incisions are used for fat harvest, fat shifting, and fat grafting to the outer hips and thighs

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








