Treatment of Axillary Hyperhidrosis
David L. Larson
DEFINITION
Hyperhidrosis is excessive sweating beyond the normal physiologic response to heat or emotional stimuli.
Any such sweating is excessive when it so negatively affects the daily life of individuals that their normal interactions with the world around them are compromised.
ANATOMY
The greatest concentration of eccrine (sweat-producing) glands is in the palms, axilla, and soles of the feet, where only about 5% of the glands are normally active at any one time.1
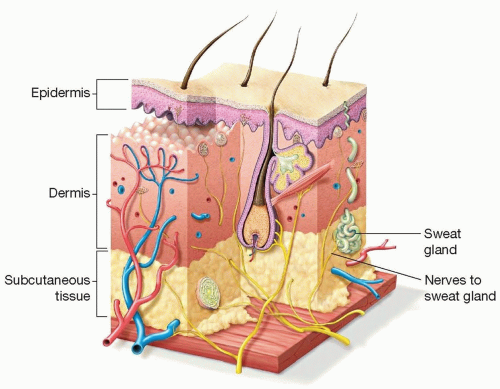
These glands are located in the subcutaneous tissue of the axilla and not in the dermis (FIG 1)—a fact that is of particular significance when considering the rationale for and effectiveness of axillary shaving in the treatment of hyperhidrosis.
PATHOGENESIS
Primary hyperhidrosis is not psychological in nature, is not self-limiting, and can significantly impact quality of life (QOL), as validated by QOL scales, showing it to be comparable to end-stage renal disease, rheumatoid arthritis, multiple sclerosis, and severe psoriasis.2,3
Secondary hyperhidrosis is associated with many common diseases (eg, Parkinson’s, hyperthyroidism, gout), conditions (eg, pregnancy, obesity, menopause), and drugs (eg, neuropsychiatric, antimicrobials, urologic) that can cause diaphoresis. Once these etiologies have been ruled out by history and/or pattern of sweating, a diagnosis of primary or idiopathic hyperhidrosis should be entertained.
NATURAL HISTORY
Though previously viewed as a benign condition, it is now recognized as a potentially extremely debilitating disease, impairing the social interactions and occupational activities of those affected.
Affecting 1.4% of the US population, axillary hyperhidrosis generally appears spontaneously in puberty or early adulthood (less than 30 years old). About one-third of these patients will be so negatively affected by the embarrassment, need of frequent change of clothes, and/or malodor that it may eliminate careers such as education, sales, and marketing.
PATIENT HISTORY AND PHYSICAL FINDINGS
Many patients (over 40%) will not seek medical aid because of embarrassment, the thought that nothing can be done, or misdirection by caregivers (eg, “learn to live with it”).
Diagnosis is made primarily by history, which includes focal, visible, excessive sweating of at least 6 months duration without apparent cause. In addition, there must be at least two of the following characteristics: bilateral and symmetric, impairment of daily activities, at least one episode weekly, onset in youth (eg, 13 to 25 years old), positive family history (usually positive in 25% of patients), and cessation of sweating during sleep. Many times, all of these findings are noted.
The only physical finding is excessive moisture in the affected area.
IMAGING/DIAGNOSIS
Diagnosis can be confirmed by measuring the transepidermal water loss (g/m2/h) using a VapoMeter (Delfin Technologies, Stamford, Connecticut) (FIG 2).4
Alternatively, the Minor test (starch-iodine test) can be used for confirmation:
Clean and thoroughly dry the axilla.
Paint the entire underarm with iodine solution or povidone-iodine.
Use a makeup brush, sifter, or gauze pad to evenly dust the site with fine starch powder.
After 10 to 15 minutes, areas of sweat will turn the mixture dark purple-blue, which should be documented with a photo.
DIFFERENTIAL DIAGNOSIS
N/A
NONOPERATIVE MANAGEMENT5
Topical antiperspirants: “clinical-grade” topical deodorants have usually been initiated by the patient. Locally applied powder can also be used, but Drysol (prescription item) only lasts 3 to 4 days, is messy, is difficult to apply, and causes local skin irritation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree